Description of the disease
Paresis is a medical term for muscle weakness due to the fact that nerve impulses do not reach them.
The state of paresis differs from paralysis in that the body does not completely lose muscle functionality. In this article we will talk about hemiparesis on the left side of the body.
The disease most often occurs either in older people as a result of serious illnesses, or in young children as a result of perinatal pathologies (cerebral palsy).
Hemiparesis is a consequence of damage to neurons in the brain or spinal cord.
Left-sided hemiparesis may vary:
- By localization:
- Central;
- Peripheral.
- According to the speed of flow:
- Spicy;
- Slowly developing.
- By severity:
- Easy;
- Moderate;
- Deep.
Help: Symptoms of left-sided hemiparesis may differ, it all depends on the degree of damage to the central nervous system, the cause of the pathology, and the age of the patient. When the disease invades the brain and facial nerve, patients begin to experience problems with facial expressions.
In addition, you can identify the following symptoms:
- Increased muscle tone;
- Prolonged migraine;
- Fever;
- Lack of appetite and fatigue;
- Aching bones;
- Weight loss;
- Muscle resistance when trying to bend a limb;
- Muscles are affected unevenly;
- Strengthening tendon reflexes;
- Rossolimo reflex, Babinski reflex;
- Emotional swings, personality disorders.
Sudden onset or very rapidly progressing hemiparesis
Stroke
When encountering a patient with acute hemiplegia, the doctor usually assumes the presence of a stroke.
Strokes occur, of course, not only in elderly patients with arteriopathy, but also in young ones. In these rarer cases, it is necessary to exclude cardiogenic embolism or one of the rare diseases such as fibromuscular dysplasia, rheumatic or syphilitic angiitis, Sneddon syndrome or other diseases. But first it is necessary to establish whether the stroke is ischemic or hemorrhagic (arterial hypertension, arteriovenous malformation, aneurysm, angioma), or whether there is venous thrombosis. It should be remembered that sometimes hemorrhage into the tumor is possible.
Unfortunately, there are no other reliable methods for differentiating the ischemic and hemorrhagic nature of stroke lesions other than neuroimaging. All other indirect evidence mentioned in textbooks is not reliable enough. In addition, a subgroup of ischemic stroke, which appears to be uniform, can be caused by both hemodynamic disturbances due to extracranial arterial stenoses, and cardiogenic embolism, or arterio-arterial embolism due to plaque ulceration in extra- or intracerebral vessels, or local thrombosis of a small arterial vessel. These different types of stroke require differentiated treatment.
Space-occupying formations in the brain with a pseudo-stroke course
Acute hemiplegia may be the first symptom of a brain tumor, and the cause is usually hemorrhage into the tumor or surrounding tissue from the rapidly forming internal tumor vessels with a defective arterial wall. An increase in neurological deficit and a decrease in the level of consciousness, together with symptoms of generalized hemispheric dysfunction, are quite characteristic of “apoplectic glioma.” In diagnosing a tumor with a pseudostroke course, neuroimaging methods provide invaluable assistance.
[10], [11], [12], [13], [14], [15], [16], [17]
Traumatic brain injury (TBI)
TBI is accompanied by external manifestations of injury and the situation that caused the injury is usually clear. It is advisable to interview eyewitnesses to clarify the circumstances of the injury, since the latter is possible when the patient falls during an epileptic seizure, subarachnoid hemorrhage, and falls from other causes.
Encephalitis
According to some publications, in approximately 10% of cases, the onset of encephalitis resembles a stroke. Usually, a rapid deterioration of the patient’s condition with impaired consciousness, grasping reflexes and additional symptoms that cannot be attributed to the basin of a large artery or its branches requires urgent examination. EEG often reveals diffuse abnormalities; neuroimaging methods may not detect pathology during the first few days; CSF analysis often reveals slight pleocytosis and a slight increase in protein levels with normal or elevated lactate levels.
Clinical diagnosis of encephalitis is facilitated if meningoencephalitis or encephalomyelitis occurs, and the disease manifests itself with a typical combination of general infectious, meningeal, cerebral and focal (including hemiparesis or tetraparesis, damage to the cranial nerves, speech disorders, ataxic or sensory disorders, epileptic seizures) neurological symptoms.
In approximately 50% of cases, the etiology of acute encephalitis remains unclear.
[18], [19], [20], [21], [22], [23]
Postictal state
Sometimes epileptic seizures go unnoticed by others, and the patient may be in a coma or in a state of confusion, having hemiplegia (in some types of epileptic seizures). It is useful to pay attention to tongue bite and involuntary urination, but these symptoms are not always present. It is also useful to interview eyewitnesses, examine the patient’s belongings (to look for antiepileptic drugs), and, if possible, make a telephone call home or to the district clinic at the patient’s place of residence to confirm epilepsy according to the outpatient card. An EEG taken after a seizure often shows “epileptic” activity. Partial seizures that leave behind transient hemiparesis (Todd's palsy) can develop without aphasia.
Disease in children
It is generally accepted that left-sided hemiparesis in children is a type of cerebral palsy.
Most often in children, hemiparesis is externally manifested in the tone of the arm muscles, which are responsible for flexion, and vice versa, the tone in the legs is in the muscles responsible for extension.
Most often, this pathology is congenital.
Symptoms in children:
- The child stops recognizing familiar people;
- Cognitive impairment;
- Inability to control movements;
- Deterioration of sensitivity;
- Epileptic seizures;
- Headache;
- Fever;
- Loss of appetite, fatigue;
- Pain in bones and joints.
Congenital hemiparesis becomes noticeable in children by three months of life; the following initial symptoms can be identified:
- Arms and legs move asymmetrically;
- Often the hand is clenched into a fist;
- Weak support function.
Important! Basically, the final diagnosis is made by the age of one or even one and a half years, at which time children begin to walk and the symptoms become especially noticeable. Severe cases of hemiparesis also affect the child’s intellectual and psychological development.
Left-sided spastic hemiparesis
Spastic hemiparesis occurs when the head or cervical region is affected, and causes stiffness of the muscles on the opposite side of the body, in this case, the left.
Spastic hemiparesis manifests itself gradually. First, spasticity appears - tension in the limbs , which is felt as a kind of stiffness. Without treatment, this condition eventually develops into full-fledged hemiparesis.
People with spastic hemiparesis typically have characteristic external symptoms that are noticeable to others, such as the Wernicke-Mann gait.
About the disease
Right-sided hemiparesis is a pathology that is a right-sided lesion of the muscles of the body.
It is characterized by a noticeable decrease in strength and general motor ability of muscles, and incomplete paralysis of the limbs is possible.
This condition manifests itself due to acquired or congenital pathological changes in the pyramidal tracts and the brain.
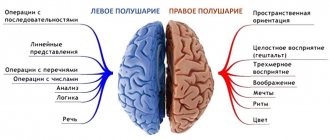
Doctors observe deviations from the norm when a lesion appears in the left hemisphere of the brain.
This disease leads to the following consequences for the patient:
- Mobility and the patient’s ability to move independently, as well as to care for themselves independently, are reduced when hemiparesis occurs on the dominant side (right-sided hemiparesis in right-handed people);
- The patient experiences inflammatory changes that are associated with prolonged skeletal muscle cramps . This consequence occurs after serious disorders - intracerebral hemorrhages and strokes;
- A problem arises when trying to follow instructions for physical therapy when the patient is undergoing motor recovery due to limited mobility. This happens when there is spastic increased muscle tone.
In children
In children, this pathology occurs as a congenital disease . The reasons for its occurrence are abnormal functionality and structure of the brain , as well as birth injuries. In medical terminology, this disorder is called cerebral palsy - cerebral palsy.
Cerebral palsy appears due to a circulatory disorder in the brain. This pathology affects the fetus while still in the womb and leads to erroneous development and damage to brain structures.
Right spastic hemiparesis
Spastic hemiparesis, often called central, occurs when there is inflammation of the brain or cervical spinal cord.
With this disease, stiffness and muscle tension are observed in the limbs of the opposite side of the body. If individual nerves of the spinal cord are subject to inflammation, then hemiparesis is combined with weakness and decreased muscle tone.
This pathology does not immediately become noticeable; it manifests itself over several months. First, muscle tone increases, which creates tension in the arm and leg, a feeling of stiffness arises, and the ability of the limbs to move decreases. Then, if no treatment is followed, muscle tone continues to increase.
Important! An increase in muscle tone indicates damage to parts of the central nervous system - the brain and spinal cord.
Disturbances in movements that are accompanied by spasticity are seen by others from the outside based on distinctive signs - people have difficulties in gait, it acquires special features. Doctors call it Wernicke-Mann gait . This indicates diseases suffered by the brain - stroke and traumatic brain injury.
Symptoms of right-sided spastic hemiparesis are varied. These include speech disorders, fever, cognitive impairment and seizures similar to epileptic seizures.
Increased muscle tone indicates that the brain and spinal cord are damaged. To reduce tone, the doctor prescribes drugs that relax the muscles. The period of admission is usually long - up to six months, but sometimes longer.
Causes
By and large, hemiparesis is not an independent disease, but a manifestation of the pathology of the nervous system in which damage to the motor center or pathways has occurred.
The resulting muscle weakness leads to paresis.
Most often, the process occurs in one part of the brain and, interestingly, pathological external processes will be noticeable in the opposite direction.
That is, if the right hemisphere is affected, the left half of the body will be affected, either completely or partially, such as an arm or leg.
This occurs due to the fact that there is an anatomical decussation of nerve fibers that originate from the brain at the level of the transition of the medulla oblongata to the spinal cord.
In children
In childhood, the cause of hemiparesis can be:
- Birth injury;
- Intrauterine infection;
- Hypoxia, that is, oxygen starvation, during pregnancy or childbirth;
- Previous infections: polio, meningitis, tetanus, tuberculosis.
In adults
The cause of left-sided paresis in adults can be:
- Oncology of the central nervous system;
- Head injury;
- Degenerative diseases of the central nervous system, such as Parkinson's disease and Alzheimer's disease;
- Epilepsy;
- Consequence of a serious infectious disease: encephalitis, meningitis, tetanus, rabies, etc.;
- Thrombus;
- Hemorrhages in the head (stroke);
- Lumbosacral plexitis;
- Aneurysm;
- Frequent stress or severe one-time stress.
Factors in the development of cerebral palsy
The causes of the disease include:
- premature or difficult labor
- hypoxia or asphyxia;
- infections during pregnancy;
- having a twin;
- congenital anomalies of the spinal cord or brain;
- impaired cerebral circulation;
- chronic diseases, hypo- and vitamin deficiency in the mother;
- smoking and drinking alcohol by the mother;
- Rhesus conflict.
There are often multiple risk factors present. It is not possible to name a specific reason in all cases.
Diagnostics
Accurate diagnosis is carried out in a clinical setting and includes:
- Taking anamnesis and visual examination of the patient;
- CBC and biochemical blood test;
- Analysis of urine;
- ECG;
- CT or MRI of the brain, cervical spine, spinal cord;
- EEG;
- Dopplerography of cerebral vessels;
- Electroencephalography;
- CSF analysis;
- Cerebrospinal fluid analysis;
- The muscle strength of both sides of the body is compared;
- Muscle resistance test;
- Barre test - holding hands in weight;
- For children, in addition to early examination by a neurologist, ultrasound of the brain is used.
Subacute or slowly developing hemiparesis
Most often, such disorders are caused by the cerebral level of damage.
The reasons for this type of weakness are:
Strokes
Vascular processes such as developmental stroke. Most often there is gradual progression. This cause may be suspected based on the patient's age, gradual progression, presence of risk factors, arterial murmur due to stenosis, and previous vascular episodes.
Brain tumors and other space-occupying processes
Intracranial mass lesions such as tumors or abscesses (most often progressing over weeks or months) are usually accompanied by epileptic seizures. With menigiomas there may be a long-term history of epilepsy; As a result, the volumetric process leads to increased intracranial pressure, headaches, and increasing mental disorders. Chronic subdural hematoma (mainly traumatic, sometimes confirmed by a history of mild trauma) is always accompanied by headache and mental disorders; Relatively mild neurological symptoms are possible. There are pathological changes in the cerebrospinal fluid. Suspicion of an abscess appears in the presence of a source of infection, inflammatory changes in the blood, such as acceleration of ESR, rapid progression. Due to hemorrhage into the tumor, symptoms may suddenly appear, quickly increasing to hemisyndrome, but not similar to a stroke. This is especially true for metastases.
Encephalitis
In rare cases, acute hemorrhagic herpetic encephalitis can cause a relatively rapidly growing (subacute) hemisyndrome (with severe cerebral disorders, epileptic seizures, changes in the cerebrospinal fluid), soon leading to a coma.
Multiple sclerosis
Hemiparesis can develop over 1-2 days and be very severe. This picture sometimes develops in young patients and is accompanied by visual symptoms such as retrobulbar neuritis and episodes of double vision. These symptoms are accompanied by urinary disorders; often pallor of the optic nerve head, pathological changes in visual evoked potentials, nystagmus, pyramidal signs; remitting course. In the cerebrospinal fluid there is an increase in the number of plasma cells and IgG. A rare form of demyelination called Balo concentric sclerosis can cause subacute hemisyndrome.
[33], [34], [35], [36], [37], [38], [39], [40], [41]
Atrophic cortical processes
Localized unilateral or asymmetric cortical atrophy of the precentral region: impairment of motor functions can be slowly increasing, sometimes taking years to develop hemiparesis (Mills' palsy). The atrophic process is confirmed by computed tomography. The nosological independence of Mills syndrome has been questioned in recent years.
[42], [43], [44], [45], [46], [47], [48], [49], [50]
Treatment
Since left-sided hemiparesis is a consequence of the underlying disease, then, first of all, it is necessary to treat it. But at the same time, it is equally important to devote time to symptomatic therapy against hemiparesis.
In children
Mainly, in the treatment of children, emphasis is placed on:
- Classes with a speech therapist for the treatment of speech dysfunction ;
- Classes with a defectologist for developmental delays;
- Treatment of episyndrome;
- Drug therapy.
In addition to this, it can help a lot:
- Gymnastics;
- Therapeutic baths and mud;
- The use of orthopedic cribs, orthopedic shoes (website of children's orthopedic shoes);
- Surgical intervention, if necessary;
- Holidays at resorts.
In adults
To treat hemiparesis, drug treatment is used primarily to improve neuromuscular conduction. Muscle relaxants to relieve tone, medications to improve blood circulation, anticonvulsants.
In addition, adults can also be prescribed:
- Orthopedic treatment: shoes, splints;
- Physical therapy and gymnastics;
- Massage.
Water procedures:
- cold and hot shower;
- water gymnastics.
Exercise therapy and a set of exercises
A therapeutic set of exercises shows good results in the treatment of left-sided hemiparesis. You can practice both in specialized centers and at home. The main thing is that the classes are constant, or better yet, daily .
Exercise sets are usually developed individually for each patient . You can give an example of such a system of exercises as:
- Pulling the chin to the chest;
- Tilt of head to shoulders;
- Rotational movements of the hands;
- Raising your arms to shoulder level;
- Rotational movements of the feet;
- Raising on toes;
- Flexion and extension of the legs in a lying position;
- Raising your legs while lying down.
We invite you to visually familiarize yourself with an interesting video on the topic:
Prognosis for adults and children
The prognosis for left-sided hemiparesis depends on many factors: the patient’s age, his medical history, how quickly treatment and recovery began. But, most often, with acquired hemiparesis, the prognosis is favorable, and most patients can restore all muscle functions .
Information: In cases of congenital hemiparesis in a child, doctors usually give cautious prognoses. Because mild forms of left-sided hemiparesis respond well to treatment, while severe forms can only be partially corrected.