Cerebrovascular disease (CVD) is a disorder of cerebral circulation due to the occurrence of lesions of cerebral vessels. Frequent causes of this disease are atherosclerotic plaques, surges in blood pressure, which are manifested by ruptures of blood vessels when damaged (hemorrhage, aneurysm, ischemia, etc.).
Cerebrovascular disease in its sudden, severe manifestation is a stroke. Fatal cerebral blood flow disorders occupy 2nd place in the statistical analysis of groups of diseases that lead to rapid death.
Types
- Hemorrhagic stroke. It is characterized by necrotic processes in the walls of arteries and veins. The most common cause is long-term chronic hypertension. A sharp increase in pressure can lead to ruptures of the walls of blood vessels and the formation of hematomas. The fatal outcome of stroke is 35-60% of the total number of patients; some survivors become disabled for life, without any positive prognosis.
- Ischemic stroke.
- Occlusion of arteries and veins. Violation of the general blood flow, leading to the formation of blood clots. There are many reasons for the occurrence of occlusions: foreign bodies, tumors, plaques, aneurysms, etc.
- Hypertensive encephalopathy.
- Moyamoya disease.
- Cerebral arteritis.
- Transient ischemic attack. Cerebrovascular accident with focal neurological symptoms. The manifestations are the same as for strokes, but disappear within 24 hours. If symptoms persist longer, a stroke is diagnosed.
- Hypertensive cerebral crisis is a particular form of hypertensive crisis, characterized by a significant jump in blood pressure and aggravation of existing cerebral disorders. Symptoms most often indicate focal damage to the trunk. Women suffer more often. This type of CVD has a malignant course.
- Discirculatory encephalopathy is a concept used in domestic medicine. The disease progresses slowly, cerebral circulation disorders take on a diffuse, increasing character, and a general disturbance of higher cerebral functions occurs.
Cerebrovascular diseases: retribution for carelessness or an inevitable reality?
Russia - half a million strokes per year
Cerebrovascular diseases (CVDs) are the most important medical and social problem of modern neurology, as they give the highest rates of morbidity, mortality and disability.
CVD is divided into acute (stroke and transient cerebrovascular accidents - transient ischemic attacks), as well as chronic forms (chronic cerebral ischemia - “dyscirculatory encephalopathy”, vascular dementia). This division is conditional, since stroke, as a rule, develops against the background of chronic cerebral ischemia, being a certain stage of cerebrovascular disease.
Within the framework of the ICD X, the classification of CVD is carried out in connection with the predominant lesion of the vascular system of the brain, which is reflected in the corresponding headings: I 65—“Occlusion and stenosis of the precerebral arteries, not leading to cerebral infarction”, I 66—“Occlusion and stenosis of the cerebral arteries, not leading to cerebral infarction"; and also depending on the leading clinical syndrome in headings I 67—“Other cerebrovascular diseases”: I 67.2—cerebral atherosclerosis, I 67.3—progressive vascular leukoencephalopathy, Binswanger’s disease; I 67.4—hypertensive encephalopathy, “other specified cerebral vascular lesions: acute cerebrovascular insufficiency, chronic cerebral ischemia” (I 67.8).
Vascular dementia is also distinguished - heading F 01 (F 01.0 - vascular dementia with acute onset, F - 01.1 multi-infarct dementia, F 01.2 - subcortical vascular dementia, F 01.3 - mixed cortical and subcortical dementia), as well as a number of neurological syndromes considered as consequences of previous cerebrovascular diseases (section I 69). In ICD-10, the term “dyscirculatory encephalopathy” is absent. However, in our country it is the most commonly used.
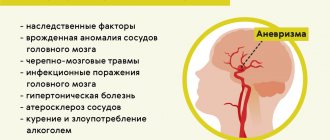
The etiology of CVD is extremely complex and involves complex interactions between numerous factors. According to WHO, there are over 300 risk factors associated with stroke, which are grouped into four categories:
- main modifiable risk factors (high blood pressure, atherosclerosis, smoking, physical inactivity, obesity, unhealthy diet, diabetes);
- other modifiable factors (social status, mental disorders, emotional stress, alcohol abuse, certain medications);
- non-modifiable risk factors (age, heredity, nationality, gender);
- “new” risk factors (hyperhomocysteinemia, inflammation, abnormal blood clotting).
“Axis of evil” of cerebrovascular pathology
The main “axis of evil” in the pathophysiology of CVD is endothelial dysfunction and changes in the rheological properties of blood, which underlie the increase in its coagulation activity.
However, despite the presence of universal patterns, the process of cerebral ischemia is individual. The features of its course are determined by the compensatory capabilities of cerebral blood flow, the background state of brain metabolism and the reactivity of the neuroimmunoendocrine system.
On average, about 400-500 thousand strokes (80-85% ischemic) are registered annually in Russia, of which up to 200 thousand are fatal, and of the surviving patients, at least 80% remain disabled. There is also a tendency towards an increase in the incidence of stroke in young people.
Therefore, modern neurology is dominated by the doctrine of the dynamic nature and potential reversibility of cerebral ischemia and the need for urgent measures to restore cerebral blood flow. Moreover, the stages of the pathophysiological cascade of the acute period of acute ischemic disturbance of cerebral hemodynamics have been revealed and it has been shown that the leading links of the pathological cascade are glutamate “excitotoxicity” with the activation of intracellular enzymes and the accumulation of intracellular Ca2+, increased synthesis of nitric oxide and the formation of oxidative stress, the development of a local inflammatory reaction, damage to the blood-brain barrier and microcirculatory disorders.
Genetic factors (latent and lifelong risk factors) are among the main non-modifiable risk factors and are receiving increasing attention in clinical trials of vascular diseases.
However, association studies between specific genotypes and diseases are often difficult to replicate. The extreme complexity of the physiological mechanisms mediating the influence of molecular genes on human physiology suggests that genotype-phenotype association studies will have one of the lowest signal-to-noise ratios of any type of epidemiological case-control study. In fact, the influence of many genetic factors appears only under certain environmental influences (smoking, taking certain medications, alcohol). For example, the presence of the Leiden variant increases the risk of thrombotic events by 2.6 times. When patients with this nucleotide variant of the F5 gene (or other genetic defects affecting blood clotting) also take oral contraceptives, the risk of sinus thrombosis increases almost 30 times, thus making sinus thrombosis almost inevitable. All external factors, such as diet and lifestyle, can theoretically be properly adjusted to minimize the risk of vascular disease. Genetic factors thus provide a unique opportunity for long-term prevention of cerebrovascular diseases in accordance with the individual genetic characteristics of patients.
Taking into account the above, the following pathogenetic forms of chronic CVD are distinguished:
- Atherosclerotic - characterized by damage to large main and intracranial vessels by the type of stenosis with the development and preservation of collateral circulatory pathways.
- Hypertensive - the pathological process develops in smaller branches of the vascular system of the brain (subcortical arteriosclerotic encephalopathy, Binswanger encephalopathy - the development of lacunar zones of ischemia and severe neuropsychological disorders with epileptic syndrome). In this variant, multi-infarct encephalopathy often develops - multiple, predominantly lacunar, small infarcts that occur against the background of arterial hypertension, with minor cardiogenic embolisms, angiopathy and coagulopathies.
Three stages of cerebrovascular insufficiency
The initial manifestations of CVD are cerebrovascular disease (weakness, increased fatigue, decreased mental performance), mild cognitive impairment. As the disease progresses, movement disorders, a sharp decrease in memory, and transient cerebral vascular crises occur. In the future, the development of vascular dementia, impaired control over the function of the pelvic organs, extrapyramidal syndrome and other various neurological complications is possible.
The most common type of chronic cerebral failure is its vertebrobasilar form, the causes of which can be not only atherosclerotic stenosis of the vertebral arteries, but also their deformation, congenital hypoplasia, compression caused by pathology of the cervical spine, etc.
This clinical form of CVD is characterized by: frequent attacks of dizziness, accompanied by nausea and sometimes vomiting; unsteadiness of gait; occipital headaches; hearing loss, tinnitus; memory loss; attacks of “blurred” vision, the appearance of “fly spots” in the field of vision; attacks of sudden falling, usually without loss of consciousness.
Pseudobulbar syndrome is characterized by disorders such as dysarthria, dysphagia, dysphonia (the voice becomes quiet, monotonous), drooling, decreased control over the functions of the pelvic organs and cognitive disorders.
Emotional and affective disorders (psychopathological syndrome) are observed at all stages of CVD. The early stages are characterized by neurosis-like, asthenic and asthenodepressive disorders, then they are joined by dysmnestic and intellectual disorders. Moreover, depression is observed in 25% of patients with vascular dementia.
In the domestic literature, there are three stages of chronic cerebrovascular insufficiency:
- Stage I is characterized by asthenoneurotic disorders, anisoreflexia, discoordination phenomena, mild oculomotor disorders, and symptoms of oral automatism.
- Stage II is characterized by a deepening of memory and attention impairments, an increase in intellectual and emotional disorders, a significant decrease in performance, mild subcortical disorders and gait disturbances, more distinct focal symptoms in the form of revitalized reflexes of oral automatism.
- At stage III, clearly defined discoordination, amyostatic, psychoorganic, pseudobulbar or pyramidal syndromes arise, and paroxysmal disorders are observed. At this stage of the disease, patients are sometimes completely capable.
Vascular dementia is a difficult diagnosis
The diagnosis of CVD is based on identifying, using clinical and instrumental methods, a cause-and-effect relationship between impaired cerebral blood supply and brain damage. It is important to note that the line between acute and chronic forms of cerebrovascular accident is very arbitrary. The cause of discirculatory encephalopathy and vascular dementia can be ischemic strokes caused by stenosis of large cerebral vessels and cardiogenic embolisms. Vascular dementia in this case occurs either due to several foci, often in both hemispheres of the brain, or due to a single ischemic focus.
The presence of an elderly patient with neuropsychological changes in a history of stroke is a compelling argument for diagnosing vascular dementia. Relative signs confirming the diagnosis of CVD can be considered: vascular risk factors, especially arterial hypertension, a history of transient ischemic attacks, the appearance of pelvic disorders or difficulty walking in the early stages of the disease, local changes in the electroencephalogram.
The compensatory mechanisms of the brain are so powerful that at any given time they can provide adequate needs of the nervous system and maintain clinical well-being. But when these mechanisms become depleted due to either a sudden decrease in the lumen of the vessel or damage to the vascular wall, a stroke occurs.
With computed tomography or magnetic resonance imaging, multiple ischemic foci are visualized in such patients. The location and size of the infarction and the total number of foci are important. At the same time, it is worth remembering that the differential diagnosis between degenerative forms of age-related dementia and CVD is not always simple, especially since almost 20% of cases of elderly dementia are mixed dementia.
Even at the morphological level there is no complete clarity. In Alzheimer's disease, in most cases, signs of previous strokes are found, and in cases of seemingly definite vascular dementia, histological signs of specific degenerative changes are found. At least half or more of all dementia cases have morphological features of both types of lesions.
The most characteristic sign confirming the vascular nature of dementia is the presence of multiple ischemic foci. In general, due to the vagueness of diagnostic criteria, the category of patients with “cerebrovascular pathology” is constantly expanding, incorporating patients with arterial hypertension, various chronic psychosomatic disorders, etc., since doctors purely subjectively and speculatively formulate a clinical diagnosis based on “cerebral” complaints.
On the other hand, the problem of so-called silent strokes, traces of which are detected by neuroimaging both in patients with a newly diagnosed acute clinical episode and in people without a history of stroke, has attracted much attention. Such instrumental findings confirm the idea of the cerebrovascular pathological process as a continuum: brain damage does not occur just like that, without an already established morphological background, in particular, changes in the vascular wall.
Restore hemodynamics and metabolism
Treatment of CVD should include interventions aimed at the underlying disease that initiated the damage to brain tissue, correction of the main syndromes, effects on cerebral hemodynamics and metabolism. Prevention of progression of CVD is carried out taking into account their heterogeneity.
In case of subcortical arteriosclerotic encephalopathy and multi-infarction condition against the background of arterial hypertension, the basis is normalization of blood pressure with correction of the perverted circadian rhythm of blood pressure. In case of a multi-infarction condition against the background of multiple cardioembolism, angio- and coagulopathies, the use of antiplatelet agents (acetylsalicylic acid at the rate of 1 mg per 1 kg of body weight per day, or clopidogrel, or dipyridamole 150-200 mg/day) and anticoagulants (for cardiac arrhythmias) is indicated warfarin is absolutely indicated).
Preventive treatment includes, as necessary, vasoactive drugs: pentoxifylline, vinpocetine, etc. Treatment of the main syndromes includes the use of nootropics, amino acid drugs and neurotransmitters (glycine, neuromidin, choline alfo-scerate), in case of impaired cognitive functions - ginkgo biloba preparations, anticholinesterase drugs. For dizziness and tinnitus, it is advisable to prescribe betahistine 16 mg 3 times a day.
Nootropics have an effective effect on cerebral hemodynamics and metabolism due to the implementation of multilateral (membrane stabilizing, antioxidant, neuroplastic, antihypoxic, neurotransmitter) neuroprotective effects. Particular attention has recently been paid to combination drugs that simultaneously improve cerebral perfusion and metabolism, such as the drug piracetam + cinnarizine. Moreover, primary neuroprotective therapy should begin within the “therapeutic window”, since its implementation during this period reduces the likelihood of severe strokes, extends the safe period for thrombolic therapy and in some cases has a protective effect against excessive reperfusion syndrome.
Since strokes are considered the most serious and obvious sign of progression of CVD, the main direction in the management of such patients is the organization of effective measures for primary and secondary prevention of acute cerebrovascular accidents (ACVA).
Primary prevention of stroke means preventing stroke in healthy individuals, patients with initial forms of CVD and in high-risk groups. Secondary prevention aims to prevent recurrent strokes.
Rehabilitation of patients and prevention of stroke are carried out according to a step-by-step program:
- stage 1 - establishment of a rehabilitation diagnosis, reflecting the clinical form, stage of the disease, the presence of concomitant pathology, psycho-emotional disorders;
- stage 2 - development of an individual rehabilitation program taking into account the biopsychosocial model of the disease (with the active participation of the patient) based on complex treatment;
- stage 3 - monitoring of effectiveness according to clinical neurological examination and neuropsychological testing, followed by correction of the complex of rehabilitation measures;
- stage 4 - final - assessing the effectiveness of the rehabilitation and drawing up a plan for further management of the patient.
“Three pillars” of secondary prevention of CVD
Today these are considered antiplatelet agents, antihypertensive drugs and statins. The use of antiplatelet agents (aspirin in a daily dose of 50-325 mg, clopidogrel, dipyridamole), according to a meta-analysis of the results of 287 clinical trials, demonstrated a reduction in the risk of serious vascular events (non-fatal myocardial infarction, non-fatal stroke and death from vascular causes) by 25% in patients previously suffered an ischemic stroke. However, antiplatelet agents, in the absence of constant monitoring, can cause complications, in particular, exacerbation of gastritis or peptic ulcer, the development of a vascular event while taking an antiplatelet or anticoagulant, and hemorrhage.
Drug lowering of blood pressure leads to a significant proportional reduction in the risk of stroke (indapamide - by 29%, perindopril [4 mg] together with indapamide [2-2.5 mg] - by 43%). After a stroke, blood pressure (regardless of its level) is recommended to be reduced with diuretics and/or angiotensin-converting enzyme inhibitors, taking into account individual tolerance to such therapy (evidence level I). Most clinical studies do not support the benefits of one therapy or another, with the exception of data on the advantage of losartan over atenolol and chlorthalidone over amlodipine.
Neurological disorders in CVD are grouped into five main syndromes: vestibular-atactic, pyramidal, amyostatic, pseudobulbar, psychopathological.
The third component of effective secondary stroke prevention is considered to be lowering blood cholesterol levels (the use of statins reduces the risk of a recurrent cerebral event by an average of 24%). In patients with a history of ischemic stroke, the appropriateness of prescribing a statin (simvastatin) should be considered first (level of evidence I). Probably, the pleiotropic effect of statins is important - their anti-inflammatory effects, which are realized in the area of atherosclerotic plaques, leading to the stabilization of the latter. During this period, statin use appears to be quite adequate even without cholesterol control. Prescribing 20 mg/day of atorvastatin, simvastatin or rosuvastatin provides a targeted preventive effect of these drugs with mandatory monitoring of liver function during therapy.
Antioxidants in the fight for a healthy brain
Since free radical oxidation acts as a nonspecific pathogenetic link in CVD, the feasibility and necessity of using antioxidants in the complex treatment of such patients is obvious. Among various medicines, the Russian antioxidant-antihypoxant Mexidol® (2-ethyl-6-methyl-3-hydroxypyridine succinate), which has neuroprotective properties, stands out. In accordance with the instructions for use, Mexidol® inhibits the processes of lipid peroxidation (LPO), increases membrane fluidity, increases the activity of antioxidant enzymes, activates the energy-synthesizing functions of mitochondria and improves energy metabolism in cells, modulates receptor complexes of brain membranes, enhancing their ability to bind. Mexidol® increases the body's resistance to damaging factors and has a cerebroprotective effect.
Our clinic has accumulated significant experience in using the drug Mexidol® in the complex treatment of patients with acute and chronic cerebral circulatory failure and other CVD.
In the vast majority of cases, we used a standardized drug administration regimen:
- daily intravenous drip administration of the drug Mexidol® in a dose of 5 ml of a 5% solution (250 mg) per 200 ml of physiological solution for 5-10 days;
- Subsequently, the drug was administered orally in tablet form at a dose of 125 mg three times a day for 30 days.
All patients received complex therapy, including dehydration, cardiovascular (as indicated) drugs, drugs that selectively improve cerebral circulation, neuroprotective drugs, and anticholinesterase drugs.
In the process of summarizing clinical experience on the use of antioxidants, the following tasks were solved:
- conducting a detailed analysis of the dynamics of the symptom complex of the disease in persons receiving Mexidol® in complex treatment (including based on the results of scoring on scales in relation to different nosologies);
- comparison of the results of therapy in patients receiving Mexidol® with the results in individuals in the control group, in whom Mexidol® was not used in complex treatment.
As a result of the treatment, which included Mexidol®, all patients with CVD showed an improvement in their condition in the form of almost complete regression of the general cerebral syndrome, as well as partial regression of focal symptoms (for example, a decrease in motor deficit by 1-2.5 points, cerebellar insufficiency and sensory disorders ). A comparison of two groups of patients, one of which used Mexidol®, indicates the high effectiveness of the drug in patients with CVD.
A characteristic sign of vascular dementia is the presence of multiple ischemic foci. Due to the vagueness of diagnostic criteria, the category of patients with “cerebrovascular pathology” is constantly expanding, incorporating patients with hypertension and psychosomatic disorders, as doctors speculatively formulate a clinical diagnosis based on “cerebral” complaints.
It should be noted that the use of Mexidol® in patients where CVD was accompanied by epilepsy led to an increase in the threshold of convulsive readiness of the brain according to EEG data, which determines not only the possibility of adequate neuroprotective therapy, but also the possibility of reducing the dose of antiepileptic drugs. Another significant criterion for the effectiveness of the use of the drug Mexidol® in patients with CVD is its pronounced anxiolytic effect, verified according to the Hamilton Anxiety Scale (anxiety reduction by an average of 4.5 points) one month from the start of therapy. While using Mexidol®, patients noted a significant improvement in general well-being, an increase in vitality, which correlated with an increase in activity, assessed using the Barthel index (an average of 18 points).
The use of the drug Mexidol® in patients with CVD in all studies has proven not only its effectiveness, but also its safety. There were no significant side effects recorded, and in no case was it necessary to either discontinue the drug or reduce the course dose, which significantly distinguishes Mexidol® from other drugs, since the problem of their safety is currently very relevant and is often considered one one of the main factors in choosing treatment strategies and tactics.
Thus, the drug Mexidol® belongs to the group of highly effective drugs with a multimodal spectrum of action and undoubtedly deserves the attention of not only neurologists, but also doctors of other specialties (therapists, psychiatrists, neurosurgeons, resuscitators). By increasing the body's resistance to the effects of various stress factors (ischemia, inflammation, shock, intoxication), Mexidol® is effective for the prevention, first of all, of decompensation of cerebral blood flow in individuals at risk for cerebrovascular pathology. However, this drug should be prescribed in adequate dosages (and it is advisable to use it intravenously at the beginning of therapy, and then in tablet form) and for a certain time (at least 5 weeks), which will allow achieving a higher therapeutic effect when using it.
Sometimes an impossible task
Thus, the variety of etiological factors causing the development of CVD makes the task of differential diagnosis of their pathogenetic forms extremely complex and sometimes impossible. In this regard, the strategy and tactics for treating patients with this pathology fall into the field of entropy and are unlikely to become ideal in the coming years. Taking this into account, therapy for victims becomes long-term and multidisciplinary. This should be understood and accepted by both doctors of various specialties and patients, because the treatment of cardiovascular diseases (atherosclerosis, coronary heart disease, hypertension, thrombosis, congenital heart defects and rheumatic heart disease) should not take place in isolation, without taking into account concomitant CVD. Recently, priority has been given to outpatient preventive and rehabilitation measures for patients with CVD. First of all, this is due to the significantly lower cost and availability of treatment in outpatient settings compared to inpatient ones. But can the measure of the correctness of patient management be a “coin”, when the price of manipulation is human life?
Symptoms
The main symptoms that may indicate CVD and are a reason to consult a doctor:
- decreased performance due to general fatigue
- decreased emotional background, mood swings
- sleep and wakefulness disorders, problems falling asleep, insomnia, frequent awakenings
- general cognitive impairment, characterized by problems with short-term memory, the appearance of stringiness of thinking, the formation of mental cud, getting stuck in one job and the inability to switch attention to another process; there are problems with mental counting
- excessive fussiness
- headaches become constant and persistent
- cerebral crises occur occasionally, severe disturbances in brain function are observed
- the appearance of weakness in the limbs, speech impairments take on severe symptoms, sensitivity decreases or changes, and visual acuity decreases.
If you notice the slightest manifestation of the listed symptoms in yourself or your loved ones, immediately contact a neurologist. In these cases, only the timely intervention of a qualified specialist can preserve legal capacity, and in some cases even life.
Prevention
Preventive measures are best carried out in specialized medical rehabilitation centers. Here the patient is under constant medical supervision, his health indicators and the effectiveness of the procedures are monitored. It is advisable to visit such an institution once every six months.
At home, you must follow the following rules:
- Stick to a diet - you should exclude fatty and fried foods. It is necessary to enrich the diet with lean fish, beef, rabbit meat, nuts, and eat a couple of eggs twice a week. These products contain calcium, which is necessary for blood vessels.
- Drinking 2 liters of liquid daily will reduce blood viscosity and improve brain nutrition.
- Walking in the fresh air every day - such procedures will benefit cerebral circulation and the entire body.
- Sleep 8 hours a day.
- Visit your doctor once a month.
- You can expand the program with breathing exercises.
Diagnosis of CVD
Primary diagnosis is carried out by a neurologist and includes:
- thorough examination of complaints, medical history and life history
- assessment and analysis of symptoms, including those preceding the disease
- full neurological examination
According to indications, additional examination methods are prescribed:
- laboratory research
- ultrasound examinations, including duplex and triplex scanning of blood vessels with Dopplerography
- functional, incl. 24-hour blood pressure monitoring and ECG
- X-ray
- MRI and CT of the brain
According to indications, a consultation with other medical specialists is prescribed, including a cardiologist, endocrinologist, therapist, nephrologist, psychotherapist, etc.
Treatment of CVD
When treating CVD, a systematic approach to the patient’s body condition is very important. Here are just a few of the hundreds of aspects that should be taken into account by a neurologist when prescribing a course of treatment for CVD:
- If blood pressure correction is necessary, it should be done gradually, avoiding a sharp decrease in pressure, as this can lead to a worsening of encephalopathy (brain damage). To normalize blood pressure in patients with CVD, it is recommended to use drugs from the ACE inhibitor group.
- Antiplatelet drugs are indicated for all patients suffering from vascular diseases or having a predisposition to their development.
- The use of acetylsalicylic acid derivatives is recommended as basic therapy for CVD.
- For patients with lipid metabolism disorders that cannot be corrected, statins are prescribed. Contraindications to statins are liver failure, myopathies and atherosclerosis (presence of plaques in blood vessels).
The general course of treatment is selected individually and is based on a thorough study of each specific case of CVD. The neurologist will take into account all the nuances of the disease and prescribe:
- medications that improve metabolism, blood circulation and restoration processes in nervous tissue
- Medicines can also be used in injection form, including intravenous drips in a cozy day hospital
- classic massage
Treatment is prescribed only by a competent neurologist. Self-medication is not only inappropriate - it is contraindicated.
Causes
The list of causes of neurocirculatory dystonia is extensive. It includes:
- hormonal changes: puberty, pregnancy, menopause;
- acute and chronic stress;
- physical or mental fatigue;
- lack of sleep;
- bad habits: smoking, alcohol abuse;
- poor nutrition and excess body weight;
- change of climate and time zones;
- hereditary predisposition;
- drinking large amounts of coffee, energy drinks, and certain medications;
- infectious diseases;
- pathology of the endocrine glands;
- mental disorders;
- osteochondrosis of the cervical spine;
- chronic pathology of the gastrointestinal tract, kidneys, digestive or cardiovascular systems.
Make an appointment
FAQ
Does CVD only occur in older people?
Naturally, CVB occurs more often in old age, but it also happens in young people. Especially in the presence of congenital vascular anomalies and predisposition. Therefore, it is incorrect to base the diagnosis of this disease only on age.
I had a stroke. Could it happen again?
Recurrent strokes are quite common. Especially if adequate preventive treatment is not carried out. With regular monitoring by a neurologist and following the doctor’s recommendations, the likelihood of recurrent strokes is significantly reduced.
What tests should I undergo if I have cerebral vascular disease?
The scope of necessary laboratory and instrumental tests should be determined by a neurologist at the appointment, because it is individual. Most often, laboratory tests examine indicators of blood clotting, kidney and liver function, pancreas and blood lipid metabolism; from instrumental studies: ultrasound examination of blood vessels, brain tomography and others.
Management of patients with cerebrovascular diseases and headache
The general principles of management of this category of patients are the determination of the etiopathogenetic cause of existing disorders, a thorough diagnostic search in order to identify primary or secondary forms of hypertension, treatment of existing diseases and modification of risk factors for the development of CVD and the progression of chronic cerebrovascular accidents. In particular, it is necessary to control glucose and blood pressure levels, adequate antihypertensive therapy, correct metabolic disorders, stop smoking, take statins and antiplatelet therapy, and regular physical activity.
The choice of further treatment tactics in patients with CICI is based on determining the nature and severity of existing disorders, reducing the degree and preventing the progression of detected disorders. Therapy for patients with CICI should be aimed, if possible, at the pathological mechanisms of disease development, which is not always possible in real clinical practice. The most accessible medicinal method of intervention is symptomatic therapy, which makes it possible to reduce the severity of various disorders in the patient, especially in the earliest stages of the pathological process, thereby significantly improving his quality of life.
The initial stage of CIGM often occurs in fairly young patients of working age, in whom hypertension, dizziness, asthenic and vegetative manifestations, as well as cCI in the form of a slowdown in the pace of cognitive processes, decreased concentration and impaired executive functions, significantly affect professional, and over time - and for household activities. In this case, the use of drugs with a multimodal mechanism of action, which can effectively, safely and pathogenetically influence existing disorders, is important for patients with CICI.
One of these drugs is Vasobral® (Chiesi Pharmaceuticals LLC), which is a combination of a dihydrogenated ergot derivative α-dihydroergocriptine and caffeine, which improves its absorption. Most of the universal effects of the drug Vasobral® are due to the blockade by α-dihydroergocriptine of α1- and α2-adrenergic receptors of vascular smooth muscle cells and a stimulating effect on dopamine and serotonin receptors [32]. According to experimental data, when using the drug Vasobral®, the aggregation of platelets and erythrocytes decreases, the permeability of the vascular wall decreases, metabolic processes in the brain improve and the resistance of cerebral tissues to hypoxia increases [3]. The second component, caffeine, has a direct stimulating effect on the central nervous system, mainly on neurons of the cerebral cortex, increases mental and physical performance, reducing fatigue and drowsiness, and also increases the bioavailability of α-dihydroergocryptine [32].
In one of the studies [3] involving 293 patients with the initial stages of CICI, 3 months of use of the drug Vasobral® showed a significant decrease in the severity of CI and subjective manifestations in the form of headache, dizziness and other nonspecific symptoms, and an improvement in the quality of life of these patients. The authors of the study [3] demonstrated the feasibility of long-term therapy with Vasobral®, since positive clinical dynamics increased throughout 3 months. therapy and was more significant than after 1 month. use of this medicine. In addition, there was a high patient adherence to therapy with Vasobral® and its good tolerability in patients with CICI in the presence of arterial hypertension, against the background of antihypertensive therapy.
In another open multicenter study [33] of the drug Vasobral® in 1341 patients (average age 59 years) with stages I and II CICM for 1 month. a significant improvement in the condition was shown in the vast majority of patients - in 82.1% of cases. This was manifested in a decrease in the intensity and frequency of headaches, improved concentration, memory and increased mental performance. The best effect was observed when high doses of the drug were prescribed, with good tolerability of treatment, no registered side effects or undesirable interactions with other drugs used by patients with CICI [33].
A survey of 1,189 patients with CVD taking Vasobral® as the main drug or as part of complex therapy, using a specially designed questionnaire, found that the most valuable properties of the drug, in their opinion, were a positive effect on memory, thinking, dizziness and other symptoms that impair them habitual functioning (75% of patients), as well as an affordable price (69%) and almost constant availability of the drug in the pharmacy network (70%) [34]. A similar test of 419 neurologists showed that 22% of respondents consider this drug the most effective drug among other medications, especially in the initial stages of CICI. Doctors considered the advantages of the drug to be good tolerability of the course of treatment (18%), a wide range of indications and clinical effects observed in practice (17%) [34].
Treatment stories
Case No. 1
Patient K., 49 years old, suffered headaches, nausea and dizziness after stress at work. Blood pressure was 190/100 mmHg. After 2 hours, difficulties (blurredness) in speech and numbness in the right hand suddenly appeared, which lasted for about an hour. The next day I went to see a neurologist at the EXPERT Clinic. The patient was diagnosed with a transient ischemic attack and hospitalization in a neurological hospital was recommended, which he refused. In this regard, the patient was prescribed treatment and examination. The patient underwent a course of intramuscular and intravenous drip injections in the day hospital of the EXPERT Clinic. Headaches and dizziness have completely regressed. During examination, patient K. was found to have significant stenosis of the left internal carotid artery due to an atherosclerotic plaque. The patient was referred for consultation with an angioneurosurgeon and subsequently underwent a planned operation, during which the stenosis was eliminated and adequate blood circulation in the left internal carotid artery was restored.
Types of pathology
Depending on the prevailing symptoms, several types of NCD are distinguished.
- Cardiac. Symptoms related to the heart come to the fore. A person experiences stabbing or pressing pain in the chest, which is accompanied by an increased or decreased pulse, and a feeling of interruptions in the functioning of the heart. The pain syndrome often spreads to the left arm, completely simulating a serious pathology. At the height of an attack, a person often feels weak, dizzy, and afraid.
- NCD of hypotonic type. This type of dystonia is manifested by a periodic decrease in blood pressure. Insufficient oxygen supply to the brain leads to severe dizziness or even fainting. Against the background of low pressure, a spasm of the capillaries occurs, as a result of which the skin turns pale, the hands and feet become very cold. Lack of oxygen leads to a subjective feeling of stuffiness and shortness of breath.
- NCD of the hypertensive type. Manifests itself with periodic increases in blood pressure. During an attack, a person feels hot, his face turns red, and a severe headache appears. Vomiting often occurs during an attack. Often the trigger is a change in weather. Patients get tired quickly and experience mood swings.
- NDC of mixed type. This type of pathology is the least predictable. Blood pressure rises and falls, which is accompanied by corresponding symptoms. Often there are malfunctions in the gastrointestinal tract (diarrhea, flatulence, vomiting), and kidneys (frequent urination). The person becomes emotionally unstable and has trouble sleeping at night.
Depending on the type of flow, the following types of NDC are distinguished:
- mild: symptoms of the disease appear extremely rarely, the person leads a normal lifestyle;
- moderate: manifests itself in single crises, the frequency of attacks affects daily life;
- severe: a person experiences symptoms of NCD almost constantly; against their background, vegetative crises regularly occur.