home
/
Branches and centers
/
Headache Treatment Center
/
Overuse headache (Headache caused by excessive medication)
Branches and centers
Treatment methods
Diagnostic methods
Diseases and symptoms
Frequent headaches are a good reason to immediately contact a neurologist. Otherwise, you can miss the onset of a serious illness or lead yourself to the development of an abusive headache. Most patients suffering from chronic daily headaches overuse tranquilizers, analgesics, and combination drugs that include codeine and barbiturates. It is due to the frequent use of analgesics that abuse headaches develop. Translated from English, “abuse” means abuse.
Description of the disease
Overuse headache occurs due to long-term use of painkillers and sedatives. In addition to painful sensations, this pathology is dangerous because it changes the initial picture of the disease, which blurs the clinical picture and leads to treatment errors. Changing the pattern of primary headaches may lead to changes in therapeutic methods, which will not cure the underlying cause. The patient will fight the investigation.
In addition, uncontrolled and long-term use of analgesics and tranquilizers leads to the development of diseases of other organs and systems: circulatory, gastrointestinal tract, kidneys, liver.
Important! Overuse headache can develop exclusively in patients suffering from frequent headaches. Under other circumstances, even with long-term use of similar drugs, this pathology does not develop.
Symptoms
The symptoms of abusive headaches depend mainly on which drug was most often used to relieve pain. Overuse syndrome develops three or more months after taking high doses of analgesics and/or ergotamine.
Characteristic symptoms:
- The intensity of pain is observed in the first hours after waking up, i.e. in the morning.
- Abuse pain is daily in nature and feels like a dull, squeezing pain. Sometimes turning into migraine-like or tension pain - squeezing/tightening.
- In most cases, the pain is moderate.
- Increased pain is observed with physical or mental stress.
- The culmination of pain is associated with the cessation of the use of habitual analgesics.
- The peak of pain may be accompanied by sound and photophobia, nausea, and sometimes vomiting.
- The pain relief effect of the drugs is short-lived
Additional symptoms:
- constant feeling of fatigue;
- decreased performance;
- fast fatiguability;
- sleep disturbances, problems falling asleep;
- irritability;
- "fog" in the head.
Do I have medicinal (“abuse”) headaches?
To answer this question, it is necessary to highlight certain characteristics of this type of headache:
- Occurs daily and persists throughout the day, varying in intensity;
- Present already at the moment of awakening;
- Described as mild, moderate, dull, bilateral, localized to the fronto-occipital region or the entire head;
- A significant increase in pain can be observed with the slightest physical or intellectual stress, as well as if medication is interrupted;
- Relief from painkillers is temporary and incomplete;
- A sudden change in the characteristics of the original headache (for which medication is taken), sometimes within one day (for example, migraine pain may take on the typical features of a tension-type headache (see other articles)).
In many cases, the diagnosis of drug headache becomes apparent only after the pain has subsided following cessation of exposure to a particular substance. If the headache does not stop or improve noticeably within 2 months after stopping the offending drug, the diagnosis should be questioned.
The most informative method confirming the presence of drug abuse (see above) is for a person to keep a diary, which notes the time of occurrence of headache attacks and the number of painkillers taken.*
*Additional studies are not required to diagnose overuse headache.
Causes
The main, and perhaps the only reason why patients develop an overuse headache is the uncontrolled use of medications or an unauthorized increase in the dose of painkillers recommended by the attending physician. Regular use of analgesics leads to the development of abusive pain. This is a secondary disease that appears against the background of untreated headaches or abuse of prescribed drugs.
Based on 29 studies of more than 2,500 patients, Diener and Tfelt-Hansen concluded that in more than 65% of cases migraine pain is caused by an overuse factor, about 25% suffer from tension pain and approximately 10% remain with mixed pain. According to statistics, women are 3.5 times more likely than men to suffer from the abuse factor. Keeping a special diary allows you to identify the real number of hundreds of tablets consumed. These numbers are different for each patient, ranging from 2 to 25 pieces per day. The average figure is 5 tablets. In more than half of all cases, patients use over-the-counter forms of drugs, only a third of them turn to specialists in a timely manner.
The abuse factor is characterized by a peculiar course; at the beginning of the disease, patients use mainly paracetamol and aspirin, after a while, resorting to complex analgesics, which include:
- coedeine
- tranquilizer
- ergotamine
- caffeine
- barbiturate.
There are cases of frequent use of pentalgin. Drug abuse is considered recognized when combined analgesics are used more than 10-12 times a month for 3 months or more, and simple analgesics more than 15 times a month. The diagnosis is considered confirmed when taking medications more than 15 days within one month.
Headache (HA) associated with excessive drug intake is defined as chronic cephalalgia, occurring for 15 days a month or more often, which develops as a result of excessive intake of any painkillers and regresses after discontinuation of these drugs. Other terms that define this form of headache are: “drug-induced headache - LIHB”, “abusive headache”, “rebound headache”. The International Classification of Hypertension identifies several forms of cephalalgia associated with excessive use of painkillers, depending on the class of drug abused by the patient: simple analgesics, combined analgesics, ergotamine drugs, triptans, opiates [2]. Patients with the most severe headache may overuse multiple classes of medications to relieve headache attacks. LIHB is a form of secondary headache and always develops from another form of primary or, less commonly, secondary cephalalgia [6].
According to the results of European and North American studies, the prevalence of LIHD in the population is 1–2% [12, 22, 25]. In a study from Brazil, the prevalence of LIHB was as high as 8% [26]. In a large Russian epidemiological study that included 2,753 people, the prevalence of LIHB was 6.43% [2]. LIHB is observed in 10% of patients visiting specialized headache centers and is the third most common form of hypertension when seen by a general practitioner.
In 1999, HC Diener and CG Dahlof conducted a meta-analysis of 29 studies, including 2612 people, which showed that the primary form of headache for 65% of patients with LIHB is migraine, for 27% - tension-type headache (TTH), for 8% - a combination of migraine and tension-type headache or another form of cephalalgia [16]. Women are more likely to develop LIHB. According to a large study conducted in a population of patients at a hypertension center, the primary form of headache in patients with LIHB in 87% of cases is migraine [9].
Primary hypertension before the development of LIHD usually lasts a long time - on average 20.4 years. The average duration of frequent use of pain medications is 10.3 years, and the average duration of chronic headache at the time of presentation is 5.9 years [17].
In a study by V. Limmroth et al. An analysis of the clinical manifestations of various forms of LIGB was carried out. It has been shown that among patients with migraine, when ergotes and analgesics are abused, headache phenomenologically becomes more similar to chronic tension headache, and when triptans are abused, it retains the “migraine” pattern: it remains one-sided, pulsating, with accompanying symptoms. The time required on average for the development of LIHB is the shortest for the abuse of triptans – 1.7 years, and longer for the abuse of ergotics (2.7 years) and analgesics (4.8 years) [23]. The multiplicity of single doses taken per month required for the development of abuse is 18 for triptans, 37 for ergots and 114 for analgesics.
Most experts share the view that patients suffering from migraine and tension-type headaches have a much greater risk of developing migraine headaches compared to patients taking pain medications for other reasons. It has been shown that patients taking large amounts of analgesics for the treatment of arthritis do not experience increased frequency of headache attacks [6]. A large prospective study examined the risk of developing chronic headache in patients with episodic headache and back pain [31]. The study included 32 thousand patients who were observed for 11 years. Patients who took painkillers daily had a higher risk of developing chronic migraine or chronic headache, while the risk of chronic neck pain was significantly lower.
It has been shown that within a year, 3% of patients with episodic forms of headache transform into a chronic form [30]. Another study [20] found that the risk of transformation from episodic to chronic migraine within a year was 14%. In patients taking painkillers more than 5 times a month, the risk of chronicity increases 20 times. The risk of chronicity is even higher in patients who abuse drugs of several classes. Thus, in a large epidemiological study conducted in the USA and including more than 8000 patients, it was shown that the risk of developing chronic migraine increases only with the abuse of combined analgesics containing opiates and barbiturates [10]. According to the results of another study [30], abuse of caffeine-containing analgesics also increases the risk of developing chronic migraine.
Other risk factors for chronicity can be divided into non-modifiable, modifiable and probable. Non-modifiable risk factors include older age, female gender, Caucasian race, low socioeconomic status, low level of education and hereditary predisposition, including a family history of emotional-affective disorders and addictions. Modifiable risk factors are frequent attacks of hypertension, obesity, consumption of large amounts of caffeine or interruption of caffeine intake, sleep disorders (snoring, sleep apnea, insomnia, hypersomnia), stressful life events, emotional and affective disorders (depression, anxiety disorder), behavioral strategies .
Experimental studies of drug abuse in experimental models carried out in recent years have made it possible to largely understand the pathophysiology of LIHB. This primarily concerns the serotonergic system. Chronic use of triptans has been shown to suppress the sensitivity of serotonin receptors in the trihymenal ganglion and also reduces serotonin synthesis in the dorsal raphe nucleus of the brainstem [27]. Chronic administration of non-narcotic analgesics to rats led to a significant decrease in the activity of 5-HT2a serotonin receptors and an increase in the activity of the serotonin transporter in the central nervous system [17]. Dysregulation of the activity of propain 5-HT2a serotonin receptors on platelets was also found in patients with PHB [17]. Moreover, in patients with LIHB, regardless of the class of abused drugs, there is an increase in serotonin reuptake [7]. Deficiencies in serotonergic systems in patients with LIH may be enhanced by the presence of genetic polymorphisms in the serotonin transport protein gene discovered by JW Park et al. [24]. Patients with LIHB also have a deficiency of other analgesic systems: C. Rossi et al. showed a decrease in two main endocannabinoids, anandamide and 2-acylglycerol, in the platelets of patients with LIHB [28].
The results of these studies allowed us to make the assumption that central sensitization plays a key role in the development of chronic hypertension and PH. Patients with chronic daily headache have reduced pain thresholds, and also more often than among patients with episodic headache (migraine or tension-type headache), the phenomenon of allodynia is noted, which is a correlate of central sensitization [13]. The indicated clinical features of patients with LIHB, which allow us to talk about the development of central sensitization, are confirmed using electrophysiological techniques [3]. Thus, in patients with chronic tension-type headache who abuse analgesics, an increase in the amplitude of laser evoked potentials was found [15].
With the introduction of functional neuroimaging methods in patients with LIH, a reversible decrease in metabolism in the areas of the brain that make up the “pain matrix” has been shown after discontinuation of analgesic drugs. However, hypometabolic changes persisted in the orbitofrontal cortex, even despite the withdrawal of the “culprit” drug, and the changes were more pronounced in patients taking a combination of drugs [19]. The results of this study provide new insight into the psychological component of excessive use of painkillers. It is a known fact that patients with hypertension often take analgesics even in the absence of headache - prophylactically, especially before an important event, when the development of an attack is extremely undesirable. Another factor that causes patients to take pain medication over and over again is withdrawal headaches. Clinically, it is manifested by a significant increase in cephalalgia when the next dose of analgesic is missed, in particular the development of headache in the morning. Patients continue to take analgesics despite their lack of effect. Moreover, patients with LIHB often abuse other classes of drugs, such as decongestants or laxatives. Keeping a headache diary allows you to identify the abuse of analgesics, tranquilizers and other drugs.
Any active substance included in a drug used to relieve headaches can cause drug abuse. Barbiturate- and opiate-(codeine)-containing combined analgesics have the greatest potential for the development of drug dependence. The characteristic signs of abuse and withdrawal symptoms from excessive use of caffeine-containing drugs and ergotamine preparations are described. Even with excessive use of simple analgesics such as paracetamol, LIHB can develop. In 90% of patients, it is not possible to identify the “culprit” substance, because a combination of drugs is taken.
Headaches with a frequency of more than 10 days per month require a differential diagnosis of LIHB. Anamnesis collection in patients with LIHB should include clarification of the type of headache at the onset of the disease (probable migraine, probable headache, another type of cephalgia), the process of transformation of episodic headache into chronic. As already mentioned, the most common cause of drug abuse is frequent episodic migraine. The transformation of episodic migraine into chronic includes not only an increase in days with headache, but also a transformation of the cephalgia itself: headache becomes bilateral, may be less intense, and there is a smaller number and severity of accompanying symptoms (nausea, vomiting, sensitivity to light and sound, worsening with physical activity) , the pulsating nature of the pain is less often noted. Thus, in its clinical characteristics, chronic migraine resembles tension-type headache to a greater extent than episodic migraine. Moreover, 80% of patients with chronic migraine abuse analgesics.
It is also important to analyze the pattern of taking painkillers: at the onset, patients usually take simple or combined analgesics that do not contain codeine or opiates. Subsequently, as the disease progresses, the effectiveness of these drugs decreases, and patients begin to use codeine- and/or barbiturate-containing drugs. The effectiveness of these products also decreases over time. Many patients resort to using injectable forms of combined analgesics. At this stage, most patients with migraine actively seek help from doctors and receive information about triptans and ergotamine-containing drugs, which at first appear to be effective. If preventive treatment aimed at reducing the frequency of headache attacks is not prescribed at this stage, patients will soon begin to take excessive amounts of triptans, creating another type of drug abuse. It is also important to identify the factors that influenced the increase in headache attacks and, consequently, the frequency of taking painkillers. You should ask the patient in detail about stressful events, background mood, anxiety, and quality of sleep. It must be remembered that headache can change its pattern due to organic reasons. Therefore, if “danger signals” are detected (the presence of focal neurological symptoms, signs of a systemic disease, cancer, including a history, symptoms of hypertensive hypertension), it is necessary to conduct neuroimaging.
The main principle of management of patients with LIHB is complete withdrawal of the drug of abuse. Clinical observations and research data indicate that until the “culprit” drug is discontinued, there will be no effect from either drug or non-drug therapy [18]. Discontinuation of analgesics by patients with LIH may be accompanied by a withdrawal syndrome that lasts from 2 to 10 days. For patients who abuse only triptans, the withdrawal period is shorter. Withdrawal syndrome is manifested by a significant increase in headache, nausea and even vomiting, increased blood pressure, tachycardia, sleep disturbance, restlessness, anxiety and irritability. For patients who abuse barbiturate-containing combination analgesics, the withdrawal period in rare cases may be accompanied by the development of epileptic seizures and hallucinations.
The analgesic can be withdrawn immediately or the dose can be gradually reduced. Optimal is immediate withdrawal, but in a quarter of patients it is not possible to immediately discontinue the abusive drug. Patients who require tapering tend to overuse combination analgesics, have a higher frequency of headache attacks, and take more analgesic doses per day [5].
There are various programs for drug withdrawal in outpatient and inpatient settings. A recent study did not show any benefit from discontinuing the drug in an outpatient or inpatient setting, therefore, it is first necessary to advise the patient to discontinue the drug in an outpatient setting [14]. Moreover, in a study by P. Rossi et al. [29] compared three groups of patients with LIHB. Patients of the first group were recommended to discontinue only the abuse drug and standard preventive therapy, patients of the second group were recommended to stop taking the abuse drug and were prescribed an outpatient detoxification program (prednisolone + standard preventive therapy), patients of the third group were also recommended to stop taking the abuse drug and undergo detoxification in the hospital (prednisolone + rehydration + antiemetics + standard preventive therapy). The proportion of patients who managed to discontinue the abusive drug did not differ between the groups – 77.5, 71.7 and 76.9%, respectively.
Treatment recommendations for the withdrawal period vary widely. These include rehydration, analgesics, tranquilizers, antipsychotics, antidepressants, valproate, intravenous dihydroergotamine, oxygen and electrical stimulation. The effectiveness of intravenous valproate was demonstrated in a large open-label study [21]. However, a double-blind, placebo-controlled study [11] did not confirm these data. Another double-blind, placebo-controlled study demonstrated superiority of injectable sumatriptan, but headache returned within 12 hours [18]. Treatment of headache with naproxen was effective in another open-label study.
Two controlled studies have shown that preventive treatment of chronic migraine will not be effective until the overuse drug is discontinued. However, in a study by C. Diener et al. Taking topiramate by patients with LIHB reduced the frequency of attacks so much that the patient stopped abusing analgesics. Most guidelines recommend starting prophylactic treatment with topiramate at or before detoxification [1, 17].
Cancellation of an abusive drug in a hospital setting is carried out in the following cases:
• abuse of drugs containing tranquilizers, barbiturates, opiates;
• if an attempt to discontinue the drug on an outpatient basis is unsuccessful;
• with accompanying anxiety and depression.
In the hospital, analgesics are withdrawn simultaneously. If vomiting occurs, it is especially important to rehydrate and use antiemetics (metoclopramide, domperidone). If withdrawal headaches occur, non-steroidal anti-inflammatory drugs (naproxen 500 mg 2 times a day) may be prescribed. If migraine-like headache attacks occur, the drugs ergotamine or dihydroergotamine may be used, provided they are not abused. An effective means of preventing withdrawal headaches is prednisolone (100 mg on the first day, and then reducing the dose by 20 mg per day). Patients with high levels of anxiety are prescribed anxiolytics, but not longer than 7-10 days.
When treating patients with LIHB, it is extremely important to use non-drug treatment methods, primarily psychotherapy. Informing the patient about the cause of his headache, the absence of organic brain pathology, as well as recommendations for the prevention and relief of attacks of cephalgia are part of cognitive behavioral therapy, which can be carried out by the attending physician. Relaxation techniques may also be recommended to patients. Outpatients should be advised to avoid barbiturate- and opiate-containing analgesics and to take simple analgesics or triptans no more than 10–12 times per month.
After discontinuation of abusive drugs, it is necessary to continue preventive treatment for at least 6 months. Topiramate is recommended as a first-line drug for preventive therapy in patients with LIHB [17]. Withdrawal symptoms such as restlessness, tachycardia, and tremor can be reduced by beta-blockers. For patients in whom LIHB occurred against the background of TTH, the drugs of choice are tricyclic antidepressants.
Treatment for LIHB is assessed as effective if the patient's number of days with HH has decreased by more than half. The effectiveness of rational therapy for LIHB is 72% over the next 1–6 months of observation [17]. In several studies, the follow-up period was 9–35 months after discontinuation of the abuse drug, and the effectiveness was 60–73% [17]. In longer follow-up (4–6 years), it was noted that 40–60% of patients experience recurrence of LPH. Predictors of recurrence are difficult to assess, but the most significant are the form of primary headache from which PHH arose (patients with tension-type headache have a higher risk of recurrence), and the duration of uncontrolled use of drugs to relieve headache.
Thus, LIHB is a complex medical and neurological problem that requires long-term dynamic monitoring of the patient, selection of rational pharmacotherapy to relieve headache attacks, their prevention and treatment of withdrawal symptoms.
Consequences
Any disease that is not treated in a timely manner has its consequences for a person. In some cases, the consequences are minimal and go away with proper therapy. Sometimes it happens that a seemingly “frivolous” disease, like a snowball, gains momentum, turning into truly catastrophic consequences for a person. In the case of the abuse factor, sleep disturbances and increased headaches are noted, nausea appears and excessive anxiety appears.
These symptoms last from several hours to 6-8 days, depending on the severity of the initial condition. Therefore, doctors recommend taking care of sick leave or a short vacation in advance during treatment. This measure will allow you to endure the withdrawal of painkillers and sedatives in the most comfortable conditions and without additional stress. As a rule, 2 weeks after stopping medications that provoke abuse factor, the intensity of headaches decreases by more than 50%.
Diagnostics
Often, diagnosing the abuse factor is difficult, since this type of pain can manifest itself individually in each patient. However, there are general criteria on the basis of which laboratory and diagnostic tests are carried out. Diagnostic methods include a comprehensive neurological examination, including the following procedures:
- Doppler ultrasound of the vessels of the brain and cervical spine;
- ECHO-encephalography;
- rheoencephalography;
- electroencephalography;
- magnetic resonance imaging of the brain;
- computed tomography of the brain;
- radiography of the skull;
- laboratory research;
- fundus examinations;
- specialist consultations.
Important! The main task of diagnosing the abuse factor is to identify the root cause of the headache. Only then can effective therapy be prescribed.
A decrease in the frequency and intensity of headaches 1-3 weeks after discontinuation of medications is considered confirmation of abuse syndrome. According to epidemiological studies, overuse headaches account for about 10% of headache complaints. American specialists at leading clinics for the treatment of diseases associated with headaches note that 75-80% of patients with headache complaints abuse analgesics.
Abuse of analgesic drugs and/or products containing ergotamine is considered recognized when the patient takes for 30 days or more:
- more than 1000 mg per day and more than 5 times a week simple analgesics: paracetalol, acetaminophrene, acetylsalicylic acid;
- more than 3 tablets per day and more than 3 times a week combined analgesics containing barbiturates, caffeine, codeine;
- more than 1 tablet per day and more than 2 times a week narcotic analgesics;
- more than 1 tablet per day and more than 2 times a week ergotamine-containing drugs.
Treatment of drug-induced headaches
A drug-induced headache goes away if you stop taking uncontrolled painkillers. Scientists at the Danish Headache Center studied patients with medication overuse headaches. For two months, 216 subjects were drug-free, although 8 patients had previously abused ergot, 12 narcotics, 43 triptans, 62 painkillers, and 90 combination analgesics. After 60 days, 144 patients (67%) had reduced headache frequency.
Headache requires examination and consultation with a doctor. Competent therapy will allow you to safely stop attacks.
Take a migraine test
Questionário ID-Migraine™ eo adequado diagnostico da migrânea
Treatment methods
Self-medication for abusive headaches is unacceptable, as it can blur the existing clinical picture and worsen the condition. When contacting a doctor, it is important to talk as objectively as possible about the nature of the pain and the medications you are taking. Concealing the fact of taking a particular group of medications leads to a distortion of the picture of the disease and the prescription of ineffective therapy. For competent treatment, it is necessary to know the doses and names of regularly used medications, since almost every patient suffering from abuse factor takes more than one medication. This is due to a decrease in the analgesic effect due to addiction. Taking medications becomes a habitual way of life for the patient.
When the usual medications are discontinued after 3-4 weeks, the patient’s condition significantly improves, the frequency of abusive pain decreases and their intensity decreases. Some patients complain of pain that preceded the development of the abuse factor.
Therapy
The main condition for successful therapy is the complete abolition of analgesics and other painkillers. During the withdrawal period, the patient must continue to regularly keep a patient diary. With abusus cephalgia, improvement occurs in about two months. Otherwise, it makes sense to doubt the correctness of the diagnosis. The treatment process consists of three stages:
- The withdrawal period for an analgesic drug depends on the type of pharmaceutical product. If the medicine belongs to the narcotic group, withdrawal should occur gradually with parallel detoxification. Non-narcotic analgesics are removed abruptly;
- During the withdrawal period, auxiliary therapy should be carried out, including antidepressants (amitriptyline has proven itself well), antipsychotics (especially when withdrawing from narcotic painkillers), anticonvulsants (for example, topiramate, valproate). Otherwise, withdrawal syndrome may be accompanied by sleep disturbances, nausea, increased anxiety, increased headaches, tachycardia, arterial hypotension, vomiting;
- Therapy after the elimination of abusive cephalgia should be aimed at treating the primary disease that led to treatment with analgesics. A few months after the abuse has stopped, the symptoms accompanying the primary pathology may begin again. In addition to the correct selection of medications, the specialist will need to prevent the recurrence of abusive headaches. Ideally, the prescription of the drug that provoked the pathology should be avoided or carried out under strict control, reducing the dosage and frequency of use as much as possible.
Therapeutic measures:
- Identifying the form of primary headache
- Intoxication of the body
- Relieving pain attacks
- Prescription of prophylactic agents
- Manual therapy
- The use of nootropic, vascular drugs, as well as homeopathic remedies and antidepressants
- Acupuncture and psychotherapeutic methods
- Prevention of relapses
The main therapeutic tactic is to discontinue the usual drugs and replace them with drugs of a different class. It is important to remember that prolonged use of analgesics leads to increased pain in these patients.
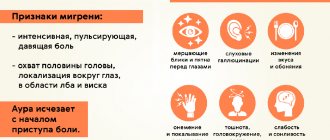
How do you know if you have a migraine?
Migraine symptoms are easy to describe. A typical migraine headache is one-sided, often in the frontotemporal region of the head, intense, pulsating, and worsens with changes in body position and physical activity. The pain is accompanied by increased sensitivity to bright light and loud sounds. At the height of pain, nausea, vomiting, fever, or, conversely, chills may appear.
However, some attacks can be moderate in intensity, involve the entire head, or sometimes occur without any pain at all in the form of a migraine aura.
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Mizonov Sergey Vladimirovich
The doctor is a neurologist. Chiropractor. Osteopath. Physiotherapist. Experience: 8 years.
Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Read also
Monoclonal antibodies against migraine
About 11% of people in the world suffer from migraines, and a third of them are forced to stay in bed during attacks.
This significantly reduces the quality of life: it interferes with work, communicating with friends and engaging in hobbies.… Read more
Orgasmic or coital headache
Orgasmic pain occurs during sex. This form of headache occurs more often in males. Symptoms of orgasmic headache: acute (paroxysmal) headache *throbbing…
More details
Tension headache
Tension headache (TTH) is one of the most common types of headache that periodically occurs in anyone, even an absolutely healthy person. It does not pose a serious threat to...
More details
Migraine
Migraine or headache seriously worsens a person's condition, especially with frequent attacks - chronic migraine. At the same time, people often do not take migraine seriously, not even thinking about seeing a doctor.…
More details
Trigeminal neuralgia
Trigeminal neuralgia is a chronic disease characterized by excruciating paroxysmal shooting pains in the area of innervation of one or more branches of the trigeminal nerve. Neuralgia…
More details
What is the cause of migraine?
It has long been believed that migraine is associated with the blood vessels that supply the brain and other structures of the head. It was believed that the aura occurs due to spasm of the cerebral arteries, and the throbbing pain is caused by compensatory vasodilation.
It is now known for sure that migraine is based on increased excitability of the brain’s nerve cells (neurons). How it arises is not known exactly, but heredity plays a significant role here. If both parents suffer from migraines, then it is very likely that the disease will manifest itself in the child. During an attack of pain, excitation from the affected brain cells spreads to neighboring neurons, then pathological pain impulses spread to large areas of the brain, including those responsible for pain. Thus, an attack of pain occurs. The hyperexcitability of neurons can be influenced by various provoking factors: certain foods (certain types of cheeses, wines, coffee), physical and emotional stress, disturbances in the rhythm of sleep and wakefulness or insufficient sleep, changes in hormonal levels during the menstrual cycle in women.