12 April 2021
11794
0
3 out of 5
Neck pain is a very common problem. After all, according to medical statistics, more than 70% of people experience this periodically or regularly. Nevertheless, there are many reasons that can provoke pain of varying intensity in the neck. Most of them lie in diseases of the cervical spine. At the same time, the characteristics of pain, its localization, and the nature of other existing symptoms are important diagnostic signs that help to correctly determine what triggered them and prescribe treatment appropriate to the situation. It is very important to identify the disease causing pain in the neck as early as possible and take measures to eliminate it, since they can cause severe complications, including disability.
Possible causes of headache on the right side
Pain in the right side of the head can occur due to various diseases and conditions. It is important to understand that it sometimes manifests itself in a healthy person and does not always indicate any violations. It can be sharp or aching, concentrated only on the right side of the head or spread over its entire surface, radiating to the neck, arms, shoulders or back.
The simplest causes of headaches on the right include physiological factors that periodically occur in every person.
- Stressful situations are one of the most common reasons for a headache on the right side. They are accompanied by the release of adrenaline into the bloodstream, which constricts blood vessels and causes an increase in blood pressure. Doctors at the Clinical Institute of the Brain recommend avoiding stress and ensuring proper rest, otherwise there is a risk of developing chronic hypertension.
- Excessive physical activity is another cause of pain on the right side of the head. After training or a busy day at work, characteristic signs appear: accelerated heartbeat, pain and discomfort in the chest, difficulty breathing. These are dangerous symptoms that indicate the need for rest.
- Bad habits can cause headache attacks on the right side. Smoking and alcohol abuse quickly worsen the condition of blood vessels and affect the functioning of the heart, reducing the speed of blood circulation in the brain. Atherosclerosis, hypertension and other diseases, as well as increased risks of stroke and heart attack can be a consequence of an unhealthy lifestyle.
- Coffee, tea, and energy drinks not only tone up, but also affect the condition of blood vessels. They narrow, which can lead to an attack of hypertension, rapid pulse and acute pain in the right side of the head.
At home, you can lead a healthy lifestyle, choose healthy foods and exercise. Taking care of the state of the cardiovascular system and physical training, as well as getting enough sleep and regular rest will help avoid pain in the right side of the head. However, during diagnosis, more serious causes of headaches in the right hemisphere may be detected - they require complex treatment, which can be obtained at the Clinical Brain Institute.
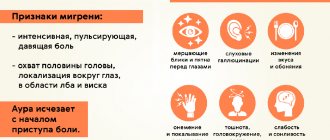
Migraine
Migraine is an attack of headache, usually one-sided. The exact cause that causes it remains unknown, but a hereditary predisposition has been found. Migraines can also appear in adulthood as a result of injuries, falls, concussions, and vascular diseases. During an attack, the patient has a headache on the right or left, and general health, performance, and concentration deteriorate. Often the overall picture is preceded by a “migraine aura” - a set of characteristic symptoms that can be used to determine the imminent onset of acute pain. These include:
- nausea, vomiting;
- increased sensitivity to bright lighting, tearing eyes;
- feeling of numbness, trembling of the hands;
- deterioration of hearing and vision.
A headache in the right hemisphere of a migraine can spread over the entire surface of the head, and also spread to the arms, neck and shoulders. The attack can last from several hours to several days. According to statistics, migraines occur more often in women. Painkillers will help reduce symptoms, but after their effect wears off, the pain returns.
Intracranial pressure
Intracranial pressure is represented by several types of fluids, including blood and the contents of the cerebral ventricles, as well as the brain. It is impossible to measure this value at home, and the diagnosis is made based on characteristic symptoms:
- headache in the right hemisphere, back of the head or temples - it is acute, throbbing, and can spread to the entire surface of the head;
- pain in and behind the eyes;
- nausea and vomiting, general deterioration of health.
With increased intracranial pressure, pain on the right side of the head radiates to the temples and often has a girdling character. Its intensity depends on the cause of hypertension. This symptom can appear one-time, due to stress, strain, or lack of oxygen in the room. Frequent attacks of headaches in the right side of the head, which are associated with pressure, require more detailed diagnosis and may indicate cerebral circulatory insufficiency.
Cluster headaches
Cluster headaches are the rarest, but at the same time the most intense type. Their exact cause is unknown. This type of pain in the right area of the head is accompanied by additional symptoms:
- drooping of the upper eyelid;
- difficulty breathing, shortness of breath;
- redness of the skin, sweating;
- lacrimation in one or both eyes, pain, increased sensitivity to light.
Acute pain in the head on the right, left, or along its entire surface lasts for 5–10 minutes, then it becomes less intense and persists for several hours. Cluster pain can occur daily, over a long period of time (several months) at specific times.
Headache on the right side due to tonsillitis
Infectious tonsillitis (tonsillitis), as well as other viral and bacterial colds, can cause headaches on the right side. It is often one-sided and appears in the half on which the inflamed tonsils are located. The patient also exhibits additional symptoms common to influenza, ARVI and other colds:
- temperature increase;
- general weakness, muscle aches;
- swelling in the throat and pain;
- nasal congestion.
A characteristic sign of tonsillitis is enlarged tonsils. This results in a severe sore throat and difficulty swallowing. White spots or plaque may be visible on them - foci of bacterial purulent infection.
Injuries and their consequences
An acute headache on the right side of the head can occur with a severe injury or fall. Bleeding from the vessels that supply the brain provokes the formation of hematomas, which put pressure on the nerve tissue. Symptoms of a traumatic brain injury may vary depending on the location of the injury and the severity of the impact:
- sharp pain in the head on the left or right side, in the temples or on the back of the head;
- impaired coordination of movements;
- incomprehensible speech, unusual behavior;
- visual defects: swelling, changes in head shape, wounds;
- nausea, vomiting, fainting;
- pain on the right side of the head radiates to the ears.
Traumatic brain injuries cannot be treated at home. They can lead to memory loss and other dangerous complications. If the right side of your head hurts due to a strong blow, it is recommended to consult a doctor immediately.
Concussion
A fall or blow can also cause a concussion. This is a disruption of its functioning that causes loss of consciousness, and in some cases short-term amnesia. If the concussion occurs on the right side, it is accompanied by pain in the right hemisphere of the head, nausea, dizziness, blurred vision and hearing, and loss of coordination. Painful sensations can persist for a long time and recur in the future, in response to physical activity, weather changes and other factors.
Stroke
Stroke is an acute disorder of cerebral circulation. This is a dangerous condition that requires emergency medical attention and poses a threat to the patient's life. The most common type is ischemic stroke. It occurs when there is insufficient oxygen supply to the brain. Its causes may be obstruction or compression of the arteries, low intracranial pressure, blood clots and other factors in which the flow of blood to the nerve tissues is stopped. It can be determined by the following characteristics:
- sharp pain in the head on the right or left;
- impaired coordination and symmetry of movements, deterioration of memory and attention;
- redness, pallor or blueness of the mucous membranes;
- muscle paralysis, decreased sensitivity of the skin in one part of the body.
A stroke occurs suddenly, but sometimes an attack can be recognized several hours before it worsens. At risk are men and women over 50 years of age with chronic heart and vascular diseases. An attack can also be triggered by excess weight, abnormalities of the arteries and atherosclerosis, irregular work hours and lack of rest, as well as bad habits: smoking and alcohol abuse.
The cause of a headache on the right or left, which occurs suddenly and is of high intensity, may be a hemorrhagic stroke. It is more dangerous to human life because it is a hemorrhage into the cerebral ventricles or the spaces between the membranes. An attack occurs when an artery supplying the brain ruptures and in most cases leads to loss of consciousness. The main task in case of hemorrhagic stroke is to seek emergency help as quickly as possible, but this does not guarantee a positive outcome.
Neoplasms
One of the causes of pain on the right side of the head is brain tumors, so it is always worth undergoing additional examination if this symptom occurs frequently. The danger is that the pain may not be too intense even with large or fast-growing tumors. Then they intensify, appear more often and become more acute. In addition, doctors at the Clinical Brain Institute recommend undergoing periodic examinations regularly - tumors in the initial stages may not cause pain or other symptoms.
Neck diseases
In the neck area there are important vessels that feed the brain and saturate its cells with oxygen. With some injuries and diseases, the movement of blood through the vessels becomes difficult, which is accompanied by headache attacks. There are several disorders that are often diagnosed in patients with chronic pain in the right side of the head:
- osteochondrosis is a disease of the intervertebral discs associated with a violation of their nutrition, in which the cartilage tissue becomes less elastic and elastic;
- protrusion - protrusion of intervertebral cartilage, often in the lateral direction (hernia is the terminal stage of protrusion);
- curvature of the spine - scoliosis of the cervical spine causes disruption of the blood supply to the brain;
- displacement of individual vertebrae is the result of injuries or weakness of the muscles of the cervical spine.
For pain in the neck that radiates to the head and arms, it is important to undergo an examination. X-rays will show the affected areas, type and stage of the disease. Based on these data, the doctor decides on the method of treatment.
Chronic paroxysmal hemicrania
Another cause of headaches on the right side of the head is chronic paroxysmal hemicrania. This is a rare autonomic disorder in which severe unilateral headaches are combined with other symptoms (nausea, photophobia, constriction of the pupils, drooping of the upper eyelid). Sharp pain in the right side of the head is often located in the temples. An acute attack lasts on average 10 minutes, but its duration can range from 5 to 40 minutes. During an exacerbation of the disease, up to 40 attacks per day can occur, in most patients - up to 5 to 10.
Meningitis
Pain in the head on the right side from above, in the temple or back of the head, which over time becomes acute and spreads over its entire surface, may be the first sign of meningitis. This is a dangerous infectious disease that affects the meninges and requires timely comprehensive treatment. The disease can be determined by the results of laboratory tests, as well as by characteristic signs:
- pain in the right side of the neck and head;
- nausea, vomiting;
- temperature rise to high levels;
- impairment of memory, consciousness, concentration;
- reduction of pain sensitivity;
- Herpes may appear in the mouth and other mucous membranes.
Meningitis can cause dangerous complications even if promptly diagnosed and treated. Nerve cells damaged as a result of infection propagation are not restored, and areas of necrosis appear in the membranes and cortex of the brain. The clinical picture differs depending on the location and size of the affected area. These may be mental, motor or sensory disorders, nervous tics and other complications, developmental delays in children. Cases of death cannot be ruled out either.
Costen's syndrome
Costen's syndrome is a rare, specific disease that is caused by dysfunction of the temporomandibular joint and jaw. It can appear only on the left or right side, as a result of which the pain will also be one-sided. Patients complain of typical symptoms:
- the right side of the head, arm and half of the neck hurts - symptoms intensify during exacerbation of the disease and decrease during periods of remission;
- fatigue, soreness, crunching while chewing;
- pressing pain on the right or left, which manifests itself during active and passive movements in the temporomandibular joint, as well as when pressing on this area;
- limited jaw movements, the patient is unable to open his mouth wide.
Patients with Costen syndrome often have additional symptoms caused by the underlying disorder. Thus, changes in bite, bruxism, one-sided abrasion of dental surfaces, and incorrect placement of teeth in the oral cavity are characteristic.
Causes of pain at the base of the skull
There are numerous causes of pain at the base of the skull, ranging from traumatic exposure to stiff neck muscles due to damage to cerebral structures. You should not try to diagnose yourself, as many pathologies may develop. Next, we will talk about some common causes of pain in the back of the head at the base of the skull, which can occur in both young and elderly patients.
First, let's look at the risk factors that are highly likely to lead to the appearance of pain due to the development of pathological changes:
- sedentary work with excessive static tension in the muscles of the neck and collar area;
- lack of regular physical activity in this area, as a result of which the muscle fiber ceases to provide a sufficient level of diffuse nutrition to the cartilage tissue of the spinal column;
- curvature of the spine and poor posture - entails a change in the lumen of the spinal canal, which negatively affects the level of intracranial pressure;
- injuries, including falls from a height, can cause a fracture of the base of the skull (this injury can be fatal);
- excess body weight, due to which there is an increase in depreciation pressure on the spinal column;
- wearing tight and uncomfortable clothes;
- incorrect placement of the foot (flat feet or club feet), as a result of which a greater than normal shock-absorbing load is transferred to the cervical spine during walking and running;
- improper organization of sleeping and working spaces;
- smoking and drinking alcohol (microcirculation of blood and lymphatic fluid suffers, which provokes tissue breakdown);
- improper diet;
- the presence of chronic inflammatory processes in the body, which can provoke the development of rheumatoid damage to the cartilage tissue of the spinal column.
Eliminating these risk factors from your daily life is a serious prevention of multiple diseases that manifest as pain at the base of the skull.
Potential causes of this symptom include the following common pathologies:
- degenerative dystrophic changes in the cartilaginous tissues of the spinal column (cervical osteochondrosis, intervertebral protrusion, extrusion or disc herniation);
- instability of the position of the vertebral bodies, leading to their displacement and rotation, due to which the nerve fiber is pinched and pressure is exerted on the spinal cord tissue;
- compensatory change in posture against the background of thoracic curvature of the spinal column;
- posterior vertebral artery syndrome;
- pinching of paired cranial nerves extending from the brain through the foramen ovale at the base of the skull;
- assimilation of the first cervical vertebra by the occipital bone;
- spinal canal stenosis;
- cerebrovascular accident in the brainstem area;
- increased levels of arterial and intracranial pressure;
- compression of the nerve responsible for the innervation of the scalp in the occipital area;
- stiff neck, for example, with encephalitis, meningitis, cerebral infarction, etc.
Only a neurologist can establish an accurate diagnosis and identify the potential cause of pain at the base of the skull. Make an initial free appointment with this doctor at our chiropractic clinic. He will conduct an examination and make an accurate diagnosis. Will give individual recommendations for effective and safe treatment.
Headache on the right side - diagnostic methods
It is important to determine the exact cause of the headache on the right side. This is impossible at home, so it is better to consult a doctor at the first alarming symptoms. The Clinical Institute of the Brain has developed general and individual programs for diagnosing headaches on the right side of the head, as a result of which it is possible to differentiate between strokes, neoplasms, infectious and chronic diseases, as well as analyze herbal disorders.
If the right side of the head hurts, the following examination methods may be required:
- X-ray of the cervical spine;
- Dopplerography - ultrasound diagnostics of the vessels of the head, which will allow you to assess the degree of blood supply to the nerve tissues;
- encephalography - studies of the electrical potential of individual areas of the brain;
- Magnetic resonance and computed tomography are one of the most informative methods for detecting tumors, cysts, areas of necrosis and other abnormalities in brain tissue;
- laboratory blood tests to determine infectious diseases.
Based on the diagnostic results, treatment is prescribed. The course is selected separately for each patient and will be most effective if the exact cause of pain and disorders caused by the underlying disease are determined. If painful sensations in the area of the right side of the head, neck, forehead occur once and do not recur, a full examination is not necessary. It is enough to monitor your health on your own and consult a doctor if the attack recurs.
Why does my whole head hurt?
Physiological reasons
One of the most common etiological factors of headaches in healthy people is stress.
Possible insomnia and mood disorders. Unlike neuroses, changes in state are short-term and quickly disappear after the end of the experience. Another common cause of the symptom is weather dependence. The headache is mild or moderate, dull, squeezing. Complemented by dizziness, irritability, depression, and increased fatigue. Occurs due to changes in atmospheric pressure, temperature and humidity. Pain throughout the head can be observed in coffee lovers who decide to stop drinking the drink. Caused by reflex vasodilation after the cessation of caffeine. The pain is pressing and varies in intensity. Unpleasant manifestations disappear within a few days, after the body adapts to new conditions. Sometimes the symptom is observed during fasting or following strict diets. Associated with the vascular response to decreased sugar levels. The pain is pressing, diffuse.
Tension headache
Develops against the background of prolonged overexertion, chronic stress, mental fatigue or depression. The painful sensations are dull, aching, squeezing, tightening, appear during the day, and rarely bother you at night. Patients say that their head is “splitting” and describe their sensations as if their head was “squeezed with a bandage” or “squeezed in a vice.” Fatigue, anxiety, and irritability are revealed.
Vascular pathologies
The symptom often worries people suffering from vascular diseases. Most often occurs with increased blood pressure against the background of essential hypertension and secondary hypertension. It occurs in the forehead or back of the head and spreads symmetrically throughout the head. As a rule, it is celebrated in the morning. The pain syndrome is bursting or pulsating, intensifies with loud sounds, physical activity, and sudden turns of the head.
In patients with hypotension, the head feels heavy. The pain is dull, bursting. Possible weakness and dizziness. Cerebral atherosclerosis is characterized by diffuse pain, which intensifies when bending over, appears in the afternoon, more often against a background of stuffiness, overwork, and is supplemented by tinnitus and sleep disturbances.
In patients with vegetative-vascular dystonia, the headache is compressive, dull, less often bursting, of a burning nature. It is part of a diverse clinical picture, which includes circulatory and sweating disorders, disorders of the digestive system, respiratory system and urination caused by autonomic dysfunction. Symptoms bother you most of the time or appear during attacks.
Pain all over my head
Intracranial hypertension
Pain is the main symptom of liquor-hypertensive syndrome. With a sudden increase in intracranial pressure - intense, rapidly increasing, with chronic pathologies - dull, constant or wavy. The pain is symmetrical, most pronounced in the area of the forehead and crown of the head, and spreads across the head. In addition, intracranial hypertension is often manifested by a feeling of pressure from the inside on the eyeballs and increased discomfort when moving the eyes.
Inflammatory lesions of the central nervous system
In patients with inflammatory pathologies, pain throughout the head is caused by intoxication syndrome, increased intracranial pressure, and cerebral edema. Meningitis is characterized by a very intense, rapidly growing pain syndrome, most pronounced in the projection of the back of the head, spreading to other areas of the head. Significant hyperthermia, chills, severe weakness, nausea, and vomiting are noted. Meningeal symptoms are positive.
Encephalitis also manifests itself acutely, accompanied by increasing headache, fever, and severe intoxication. Sometimes there are disturbances of consciousness, convulsions, and mental disorders. With arachnoiditis, painful sensations are bursting, dull, worse in the morning, after physical activity, complemented by insomnia, hyperthermia, nausea, and fatigue.
Traumatic injuries
Headache occurs in all types of traumatic brain injuries. Other characteristic symptoms are loss of consciousness at the time of injury, amnesia for previous events, nausea, vomiting, weakness, and dizziness. Manifestations vary depending on the severity of the injury. In case of a concussion, the loss of consciousness is short-term, pain and other symptoms persist for 2-3 weeks.
The bruise is manifested by a more prolonged loss of consciousness, intense pain observed for 1-2 months. The pain increases with movement, in an upright position, and decreases in a lying position. Neurological symptoms are noted: asymmetry of reflexes, nystagmus, anisocoria, mild meningeal disorders, and sometimes mild hemiparesis.
Infectious-toxic syndrome
The causes of development are ARVI, influenza, acute forms or periods of exacerbation of diseases of the respiratory system (bronchitis, tracheitis, pneumonia), and urinary tract (glomerulonephritis, pyelonephritis). Similar symptoms are observed with local purulent lesions of soft tissues (cellulitis, abscesses), deep pyoderma (carbuncle, hidradenitis).
The pain appears in different parts of the head or is diffuse. Weak or moderately expressed, pressing, aching, exhausting, monotonous. General hyperthermia ranges from low-grade fever to febrile fever. There are complaints of weakness, weakness, arthralgia, myalgia. With general infections and respiratory diseases, catarrhal symptoms are expressed: runny nose, cough, sore throat.
Exogenous and endogenous intoxications
The most common type of poisoning is a hangover after alcohol intoxication. Pain in the head occurs the morning after drinking alcohol, ranging from dull, insignificant to sharp, intense. Often pulsating. Complemented by weakness, weakness, heaviness in the body, nausea, rapid heartbeat. Disappears after lunch or in the late afternoon.
With food poisoning, the headaches are aching, minor or of moderate intensity. Abdominal pain, tenesmus, bloating, diarrhea, nausea, and vomiting are noted. Possible increase in body temperature. In victims of carbon monoxide poisoning, pain in the entire head appears due to oxygen starvation, moderate, dull, aching. It is possible to reduce criticism of your own condition.
In addition, the symptom may occur due to taking medications, poisoning with various poisons, or contact with occupational hazards (for example, odorous substances). An example of endogenous intoxication accompanied by headache is the toxic effect of malignant tumors. Pain syndrome is observed almost constantly, complemented by loss of weight and appetite.
Other reasons
Sometimes pain in the entire head is detected in the following conditions:
- Cyclic hormonal changes
. Pressing or aching painful sensations bother some women during PMS or appear during menstruation. Emotional lability, sleep disturbances, slight swelling, and tenderness of the mammary glands are noted. - Allergic reactions
. Mild or moderate pulsating pain in the head with allergic rhinitis, conjunctivitis, angioedema is explained by swelling of the mucous membranes, vascular reaction, and difficulty breathing. - Mental disorders
. Complaints of headache are often made by patients with hysterical and anxiety neurosis, depressive disorders, especially somatized depression.
Treatment of right-sided headaches
Treatments for right-sided headaches will vary depending on the cause. Tactics are aimed at eliminating both the underlying disease and its symptoms to make the patient feel better. The Clinical Brain Institute offers inpatient treatment, recovery after stroke, and observation after injury and concussion. The treatment regimen may include several stages:
- drug treatment: painkillers, anti-inflammatory and vasodilator drugs, medications to improve heart function, specific therapy for infectious diseases;
- additional techniques: massage, gymnastics, physiotherapy;
- surgical treatment is required only if tumors, hematomas, cysts and neoplasms are detected that are prone to growth and interfere with the normal functioning of the brain;
- specific schemes for stroke and traumatic brain injury, aimed at restoring nervous activity.
The Clinical Brain Institute specializes in the diagnosis and treatment of pain that occurs on the right side of the head. There are all the necessary conditions for patient examination, instrumental and laboratory diagnostics, hospital treatment and constant supervision by specialists. Doctors warn: frequent attacks, during which there is a headache and nausea, additional symptoms appear, require timely examination. In the early stages, treatment will be simpler, take less time and prevent complications.
Clinical Brain Institute Rating: 5/5 — 4 votes
Share article on social networks
Osteomyelitis is a purulent or purulent-necrotic lesion of bone tissue, bone marrow, periosteum, surrounding soft tissues and, in principle, can affect any bone, but most often long tubular bones are involved in the inflammatory process [2]. Osteomyelitis of the skull bones is a rare disease, its prevalence is 1.5%, and among cases of osteomyelitis of flat bones - 3% [5, 6]. According to foreign authors, from 57 to 95 cases of osteomyelitis of the skull are recorded annually [5]. Mortality when intracranial complications occur reaches 20-40% [1, 8]. Lack of clinical experience, features of the structure and location of the bones of the skull (spongy bone structure, proximity to important anatomical structures and the brain, a small array of soft tissue covering the bones) lead to certain difficulties in the diagnosis and treatment of osteomyelitis of the skull. Early diagnosis and adequate treatment of this disease will prevent the development of neurological complications and significantly reduce mortality.
The cause of osteomyelitis of the skull can be complicated trauma, surgical intervention on the bones of the skull, purulent diseases of the soft tissues of the head and paranasal sinuses [5-7]. Hematogenous osteomyelitis of the skull occurs extremely rarely due to resistance to infection of the flat bones. Predisposing factors for the development of osteomyelitis of the skull, leading to a decrease in bone vascularization, are diabetes mellitus, anemia, dysproteinemia, exposure to ionizing radiation, tumor lesions of the bone, osteoporosis, Paget's disease [5-7]. Osteomyelitis of the skull can occur at any age, but it mainly affects children and young people. The frontal, temporal and parietal bones are most often affected [1, 3]. Osteomyelitis of the skull occurs in acute, subacute and chronic forms, characterized by certain clinical and structural changes [3]. Moreover, depending on the nature and extent of the pathological process, superficial and deep osteomyelitis are distinguished, the latter is divided into limited and diffuse [3]. The superficial form of osteomyelitis of the skull is characterized by the involvement of the superficial bone plate in the pathological process, while in deep osteomyelitis all layers of the bone are affected. Damage to the outer bone plate often leads to the formation of a subperiosteal abscess, which, when the periosteum melts, becomes subgaleal and then subcutaneous. Damage to the internal bone plate makes it possible for the purulent-septic process to spread to the membranes and substance of the brain, which causes the occurrence of often fatal intracranial complications in the form of meningitis, brain abscess, sinus thrombosis, meningitis. Diffuse forms of deep osteomyelitis occur, as a rule, with thrombophlebitis of the diploic veins, which leads to “metastasis” of the infection and extensive bone damage [1-3].
The clinical picture of osteomyelitis of the skull depends on the etiology, prevalence and nature of the pathological process and is characterized by the predominance of local inflammatory changes. Damage to the external bone plate is characterized by swelling of the soft tissues and the formation of a subcutaneous or subgaleal abscess, deep - local headache, pain when tapping the affected area [1, 4]. Chronic osteomyelitis of the skull often manifests itself in the formation of a fistula. When intracranial complications occur, general cerebral and focal symptoms, pronounced signs of intoxication, and the general condition of the patient worsen.
The X-ray picture of osteomyelitis of the skull appears only after 2-3 weeks from the onset of the disease, allows you to diagnose mainly gross changes and is characterized by heterogeneity of the bone structure in the acute process and thickening, sequestration, blurred contours, and bone defects in the case of chronicity [2, 5]. Due to certain shortcomings of the method, at the present stage it is advisable to use computer and magnetic resonance imaging, which makes it possible to identify structural changes in the bone and surrounding soft tissues even in the early stages of the disease.
Treatment of osteomyelitis of the skull is divided into surgical and general. Radical surgical treatment is carried out provided that the inflammatory process subsides; it consists of osteonecrectomy and surgical treatment of the surrounding soft tissue. In case of superficial osteomyelitis, the affected bone is removed with pliers to its unchanged structures, the wound is sanitized with antiseptic solutions, drained and sutured tightly.
In the case of deep osteomyelitis, the osteomyelitic focus is widely exposed, the sequesters of the outer and inner bone plates are removed, the affected edges of the bone are bitten down to visually unchanged tissue, the epidural space is inspected and all purulent granulations are removed from the surface of the dura mater, the wound is drained and sutured tightly. Cranioplasty is performed no earlier than 6 months, provided there is no progression of the inflammatory process in the bone [1, 3, 7]. Surgical treatment is supplemented with antibacterial, detoxification, and corrective therapy.
We present a clinical observation.
Sick Ya.,
22 years old, was admitted to the clinic with a referral diagnosis: suppurating atheroma of the frontal region.
Upon admission, he complained of facial swelling and a painful lump in the forehead. From the anamnesis: he considers himself sick for 2 days, when, for no apparent reason, he noted the appearance of the complaints described above. This is the first time this disease has occurred; no changes in the frontal region have been noted before. As a child, he suffered a bruise in the forehead area and did not seek medical help. Upon admission, the general condition was satisfactory. Body temperature 37 °C. In the forehead area on the left, at the border with the scalp, there is a moderately painful infiltrate of dense consistency measuring 3x1.5 cm, the skin above it is not changed. The fluctuation symptom is negative. No laboratory signs of inflammation were detected. Since at the time of admission there were no convincing data indicating the process, antibacterial and anti-inflammatory therapy was started. However, during dynamic observation (within 24 hours from the moment of hospitalization), negative dynamics were noted in the local status in the form of progression of inflammatory phenomena, and therefore the patient was operated on urgently: the abscess was opened under intravenous anesthesia. Intraoperatively, a subcutaneously located abscess with a volume of up to 20 ml was identified; at the bottom of the wound there was a defect in the outer bone plate of the frontal bone with uneven edges, devoid of periosteum, with a diameter of up to 2 cm. A bone biopsy and culture from the walls of the abscess were performed. The operation was completed by sanitation and drainage of the wound with napkins moistened with an antiseptic solution. Taking into account intraoperative data in the early postoperative period, the patient underwent computed tomography of the skull in order to clarify the diagnosis (see figure),
Figure 1. CT scan of the skull. a — sagittal section: defect of the frontal bone with destruction of the outer and inner plates.
Figure 1. CT scan of the skull. b — frontal section: osteomyelitis of the frontal bone with destruction of the outer bone plate, abscess of the soft tissues of the head.
Figure 1. CT scan of the skull. c — horizontal section: through defect of the frontal bone.
Figure 1. CT scan of the skull. d — frontal section: destruction of the frontal bone with destruction of the internal bone plate.
Figure 1. CT scan of the skull. d — three-dimensional reconstruction: a through defect of the frontal bone. in which destruction of the frontal bone was revealed in the form of a through bone defect measuring 19×15 mm, which required differential diagnosis between osteomyelitis and a neoplasm of the frontal bone. Skeletal scintigraphy was performed, which revealed a single focus of hyperfixation of the radiopharmaceutical in the left frontal region. A pathohistological examination revealed hemorrhages and signs of acute inflammation in the bone tissue. Thus, based on clinical history, intraoperative and a number of instrumental data, the patient was diagnosed with hematogenous osteomyelitis of the frontal bone, paraosseous abscess. In the postoperative period, against the background of antibacterial (taking into account the data of the antibiogram), anti-inflammatory therapy, and local treatment, positive dynamics were achieved during the wound process, inflammatory phenomena were completely eliminated. The patient was discharged for outpatient observation by a surgeon with a recommendation to consult a neurosurgeon to resolve the issue of radical surgical treatment.
An observation of acute hematogenous osteomyelitis of the frontal bone in a young man not burdened with chronic diseases is presented. The hematogenous nature of the pathological process was established by excluding other possible routes of infection into the bone. The clinical picture of the disease did not allow us to establish a diagnosis of osteomyelitis of the frontal bone in the preoperative period, however, it did not fully correspond to the local purulent process in the soft tissues of the frontal region. As an additional instrumental research method to clarify the diagnosis, we used computed tomography, which made it possible to study bone changes in detail. Oncological alertness also required skeletal scintigraphy and histological examination. Complex conservative treatment carried out in the postoperative period made it possible to achieve complete elimination of inflammatory phenomena and the transition of the wound process to the second phase. It is preferable to perform radical surgical treatment in the neurosurgery department when the inflammatory process has completely subsided, and therefore the patient is recommended to consult a neurosurgeon.
Thus, the prevalence of osteomyelitis of the skull is low, but the topographic and anatomical features of this area and the danger of intracranial complications dictate the need for timely diagnosis and adequate treatment of this disease. Early diagnosis of osteomyelitis of the skull using modern instrumental examination methods, radical surgical treatment in combination with rational antibiotic therapy will significantly improve the results of treatment of such patients.