Should you worry if you can't sleep? Why is this happening? How can you adjust your lifestyle to ensure healthy sleep? We tell you together with doctors who deal with sleep disorders.
Insomnia refers to various phenomena: difficulty falling asleep, systematic awakenings in the middle of the night and inability to fall asleep again, shallow sleep. This problem plagues about a third of the world's population. Chronic insomnia, lasting more than a week, always leads to a sharp deterioration in the quality of life, decreased performance, and drowsiness during the day.
When is it time to sound the alarm?
“If the process of falling asleep lasts more than 20 minutes, and this situation lasts a week or more, this is a reason to consult a doctor,” says Gleb Lutokhin, a somnologist at the Semeynaya clinic. — If a person tosses and turns for a long time before going to bed, often wakes up during sleep and then cannot fall back to sleep for 5-10 minutes, this is a reason to think about it. Especially if these processes are accompanied by anxiety and obsessive thoughts.”
Insomnia has many adverse effects. The body does not have time to recover, the functioning of almost all systems and organs is disrupted. The nervous system suffers the most; the cardiovascular and endocrine systems, as well as the kidneys, work under stress.
“About 40% of my patients have a sleep disorder,” says GMS Clinic neurologist Sergei Makarov. — In young people, insomnia is a consequence of anxiety disorders or disruption of the daily routine. Due to the coronavirus epidemic, many people work from home until late and then sleep until lunch. And due to overexertion and lack of personal space, insomnia occurs. In older people, sleep disturbances can be caused by diseases of the heart, lungs, other internal organs, or chronic pain.”
So a young girl turned to Doctor Makarov. During the interview, it turned out that in addition to bad habits - smoking and drinking alcohol - she suffered from an incorrect daily routine. At night on weekends, the girl “hanged out” in bars and discos, sleeping off during the day. It is not surprising that the work week was difficult for the patient. The body did not have time to adapt to the daily routine when the weekend came again and history repeated itself.
Who's at risk
Statistics of visits to doctors show that middle-aged and elderly people experience insomnia much more often than young people. According to somnologist Gleb Lutokhin, the two main categories of his patients are men and women 60+, as well as women 40-55 years old. There are also many men over the age of 40 who are prevented from falling asleep by sleep apnea.
In the elderly, insomnia is often caused by vascular lesions of the brain and neurodegenerative diseases such as Parkinson's or Alzheimer's disease. Women almost always experience sleep problems at the onset of menopause. In addition, problems with falling asleep and quality of sleep often plague anxious people with increased responsibility, and these are often women. Men go to the doctor when the symptoms are so severe that they interfere with normal work and life.
Among people of various professions, those who work on irregular schedules with alternating day/night shifts have the most problems with sleep: dispatchers, train drivers, airplane pilots. Therefore, the departmental clinic of Russian Railways has its own staff of somnologists. According to the observations of Gleb Lutokhin, lawyers disproportionately often experience insomnia.
Neurologist Sergei Makarov notes that people who are engaged in intellectual work usually sleep poorly. Physical labor is the best cure for insomnia. When a person is physically tired, he falls asleep soundly and sleeps for a long time.
What are the reasons
Typically, insomnia is just an optional symptom of a more serious problem, such as cerebral circulatory problems. Most often, the real reasons lie in neurotic disorders such as depression or anxiety. Isolated, uncomplicated insomnia is extremely rare.
“As a rule, this is only a symptom in the structure of a psychopathological syndrome, which must be identified first,” says psychotherapist Irina Kolchina. “Patients often underestimate the depth of the problem and come for sleeping pills in order to restore sleep in the easiest and fastest way. This is what my recent patient did, a 32-year-old man who complained of three months of insomnia. The anamnesis showed that the sleep problems lasted for more than two years and were caused by a very serious syndrome. The patient did not agree with the diagnosis and stopped treatment, thereby driving the problem deeper.”
However, there are diseases that manifest themselves only as insomnia. For example, narcolepsy, in which a person's wakefulness at night is compensated by attacks of falling asleep during the day. Or fatal familial insomnia - an extremely rare incurable hereditary disease in which the patient dies without being able to sleep.
“In 70% of cases, the causes of sleep disturbances have their origins in psychiatry,” Gleb Lutokhin shares his experience. — Often these are mild disorders of the mental spectrum that do not manifest themselves in everyday life, but affect sleep. There are, of course, gentle people who lose sleep if they are rude at work or stepped on in a store. But more often the causes of insomnia are anxiety-depressive disorder, anxiety-phobic disorder, depression, bipolar affective psychosis or organic mental disorders.”
Thus, a very anxious man told Dr. Lutokhin that he had not slept normally for a month after being fired from work due to the coronavirus situation. The patient had obsessive thoughts - the same ideas and images, which are extremely difficult to get rid of when falling asleep. There was also a high score on the depression scale. In such cases, insomnia cannot be cured without eliminating the mental disorder, and this is the work of a psychiatrist.
Sleep disturbances in cerebrovascular disease, approaches to correction
Insomnia as a disease or as a symptom of another disease occurs in 25% of the adult population [1, 2]. Numerous factors can cause and maintain sleep disturbances in a significant percentage of older adults, including loss of occupational employment, health problems, bereavement, and changes in circadian rhythms. Changes in sleep patterns may be part of the normal aging process, but many disorders are associated with ongoing or latent diseases of the central nervous system, most notably cerebrovascular insufficiency. Chronic progressive vascular damage to the brain, which is based on cerebral microangiopathy, is the most common form of cerebrovascular disease. The range of subjective complaints in this category of patients is extremely diverse. At the same time, complaints of sleep disturbance and decreased performance are the most common. At the same time, clinicians tend to consider a complaint of sleep disturbance as part of the general aging of the body, ignoring possible other causes of insomnia, which, of course, affects the effectiveness of treatment for this symptom.
Sleep disturbances, which are common among older people and seem harmless, not only lead to a deterioration in the quality of life, worsening cognitive impairment and psychological problems, but also affect the progression of cerebral microangiopathy and mortality. It is now absolutely clear that sleep is a function of the brain and sleep affects brain function, contributing to the progression of cerebral pathology through various direct and indirect mechanisms. Primarily, circadian changes in the sleep-wake cycle may increase the risk of cardiovascular and cerebrovascular accidents.
Etiology of sleep disorders associated with cerebrovascular disease
The World Health Organization defines insomnia as repeated difficulty falling asleep, staying asleep, decreased sleep duration, and/or impaired sleep quality, resulting in disruption of normal daytime activities. It is important to note that the sleep disturbances described above should not be associated with temporary sleep restriction due to external events and/or poor sleep conditions. Insomnia is classified into the following categories: 1) transient, lasting less than 1 week; 2) short-term, lasting from 1 to 4 weeks; 3) chronic, lasting more than 1 month [3]. Chronic insomnia can be primary or secondary, and its prevalence in the population directly depends on age and the presence of chronic somatic and mental disorders [4]. The causes of sleep disturbances in vascular patients are very diverse and include both primary and secondary chronic insomnia.
Among primary insomnias associated with age and cerebral microangiopathy, two categories of sleep disorders are the most common: sleep apnea and periodic limb movements during sleep (PLMS). These disorders may contribute to the manifestation of cerebrovascular disease and may occur as a consequence of cerebrovascular events [5].
Sleep apnea syndrome - periodic cessation of breathing during sleep - can be obstructive (upper airway occlusion), central (primary neurological diseases) or mixed in origin. A patient may be suspected of having sleep apnea if three or more of the following signs are present: indications of respiratory arrest during sleep; loud, intermittent snoring; increased daytime sleepiness; frequent night urination; complaints of prolonged disturbance of night sleep (more than 6 months); arterial hypertension (especially night and morning); obesity 2–4 degrees Since awakening helps resolve obstructive apneas, sedatives and hypnotics are contraindicated in this category of patients. In addition, these drugs relax the muscles of the pharynx, which also increases apnea. Sleep apnea significantly affects physical health, for example, it can lead to hypertension, cardiac arrhythmia, cor pulmonale and sudden death. Epidemiological studies convincingly demonstrate that sleep apnea should be considered a risk factor for early death from cardiovascular diseases, including stroke, due to the development of persistent intractable hypertension [6]. There is a direct relationship between the severity of sleep apnea and the odds ratio of developing arterial hypertension. On the other hand, people who have had a stroke have a high prevalence of sleep apnea, which reduces the potential for recovery, increases the risk of secondary stroke, and increases mortality [7]. On the contrary, correction of respiratory function during sleep leads to normalization of blood pressure [8]. There is evidence that successful correction of sleep apnea with non-invasive positive airway pressure ventilation lowers blood pressure.
Nocturnal myoclonus, or nocturnal myoclonus, is repetitive unilateral or bilateral stereotypic movements (twitching) in the legs that wakes the patient. The severity of movements may vary from night to night. PDCS usually occur during the non-rapid eye movement (NREM) sleep phase in the first half of the night. The likelihood of developing PDCS as cerebral vascular insufficiency increases with age and becomes quite high in older people. For example, in people over the age of 60 years, the detection rate of PDCS reaches 34–45%. Clinical markers of PDS are dissatisfaction with night sleep, kicking at night; the likelihood of these complaints is associated with the absolute number and intensity of movements. Unlike sleep apnea, PDCS does not have such a dramatic effect on the course of cerebrovascular disease, but may be a risk factor for the following conditions: depression, memory impairment, impaired concentration, fatigue.
Chronic insomnia in patients with cerebrovascular disease is most often caused by secondary causes, in particular affective disorders. According to our own research, a complaint of sleep disturbance occurs in more than 90% of patients with chronic cerebrovascular disease, comorbid with anxiety-depressive spectrum disorders [9]. Previously, it was believed that sleep disturbances were a consequence of depression. It is now understood that the relationship between sleep disturbance and depression/anxiety is more complex. Sleep disturbances can cause or worsen depression and vice versa. Regardless of cause-and-effect relationships, insomnia is one of the most serious and difficult to treat syndromes associated with anxiety-depressive spectrum disorders. As a rule, among the symptoms of depression, sleep is the last to be restored. In addition, dyssomnia increases the risk of suicide. Sleep disturbances in depression vary widely: the typical symptom is “early insomnia,” characterized by early morning awakenings at three to five o’clock in the morning, sometimes with feelings of horror and hopeless melancholy. It is in these patients that the prevalence of depressive affect is observed in the morning hours, when complaints of poor health and severe asthenia are at their maximum. Suicides among older adults in the early morning hours are also highly associated with dyssomnia and depression. But some older patients, on the contrary, complain of difficulty falling asleep or even sleep longer at night (hypersomnia) and experience sleepiness during the day. Poor sleep is considered by the patient to be the main cause of daytime fatigue. Apparently, impaired functioning during the waking period is partly due to disturbances in sleep structure, the main of which are increased sleep latency, prolongation of the REM phase, increased time of night wakefulness, decreased slow-wave sleep, and early morning awakening.
One of the clinical manifestations of chronic diffuse ischemic brain damage is cognitive impairment. At the same time, cognitive impairment itself can be a trigger for secondary insomnia. Patients with cognitive impairment are characterized by the following sleep structure disorders: increased duration of the first phase of sleep; reduction in phases 3 and 4 of slow-wave sleep and rapid eye movement (REM) sleep, increasing the number of awakenings; increasing the period of daytime sleep. As a result of these changes, the sleep of patients with cognitive impairment becomes ineffective, which negatively affects the daily functioning of patients.
Finally, insomnia may be due to drug effects. Patients with cerebrovascular disease take on average 3 to 6 medications per day, some of which may interfere with sleep and wakefulness. For example, beta-blockers, especially lipophilic compounds (eg, metoprolol, propranolol), may cause difficulty falling asleep, increase the number of awakenings, and predispose patients to vivid dreams that frighten patients. Chronic uncontrolled use of sedative hypnotics often “confuses” the normal sleep-wake cycle. Many over-the-counter medications, including pain relievers or allergy medications, contain caffeine, which has a stimulant effect that reduces sleep time. The effects of caffeine may be more pronounced in elderly patients due to age-related decreases in caffeine clearance. Nicotine is also a stimulant and affects sleep in a similar way to caffeine. A number of studies have shown that people of all ages who smoke have more sleep problems than people who don't smoke. In smokers, the process of falling asleep is primarily affected and the duration of sleep is reduced.
Additional risk factors for dyssomnia in patients with cerebrovascular pathology may be various chronic somatic diseases (Table 1).
Assessment of sleep disorders
First of all, the doctor needs to determine the type of insomnia and the patient’s sleep habits (sleep hygiene). People with insomnia often neglect sleep hygiene, and this important aspect should be the focus of the doctor’s attention, including when choosing a treatment strategy. It is useful to evaluate a patient's medications for their effect on sleep. Medicines that often cause insomnia are presented in table. 2.
When starting to evaluate sleep disorders in patients with cerebrovascular pathology, it is first necessary to exclude sleep apnea syndrome. Sleep apnea is the most dangerous and requires specific treatment. In addition, sleeping pills are contraindicated in these patients. In the clinical picture, what primarily attracts attention is the typical portrait of a patient suffering from obstructive sleep apnea. Usually this is an overweight person of a hypersthenic constitution, with a red or purple-bluish puffy face, injected scleral vessels and a hoarse voice, whose sleep is characterized by pronounced snoring. Usually, immediately after falling asleep, a person begins to snore. Soon the patient suddenly stops breathing. At this time, no breathing sounds are heard, and snoring stops. However, the patient is trying to breathe, as can be seen from the movements of the chest and abdominal wall. After about 15–30 seconds, the person snores loudly and takes several deep breaths. As a rule, the patient's sleep is very restless: he turns around in bed, moves his arms and legs, and sometimes says something. Additional daytime symptoms of obstructive sleep apnea/hypopnea syndrome are morning headaches, arterial hypertension, and severe daytime sleepiness. Computer monitoring pulse oximetry (saturation and heart rate monitoring) is used to screen for sleep-disordered breathing. Portable devices are now available to diagnose apnea at home. The most effective treatment for sleep apnea is CPAP therapy, which provides continuous positive pressure in the airways.
Since anxiety-depressive spectrum disorders are the most common cause of insomnia in this category of patients, positive diagnosis of these disorders remains a priority.
Insomnia may predict the development of mood disorders, or affective disorders may themselves predispose to insomnia [10]. Depression is a multifaceted disease that manifests itself as a complex of mental and physical (somatic) symptoms, including sleep disturbances. The main symptoms of depression are:
- sad mood (sadness, despondency);
- loss of a sense of pleasure from usual activities;
- loss of interest in life events that previously constituted the “meaning” of life;
- increased fatigue or loss of energy.
When questioning the patient, one should actively identify symptoms of nervous tension (Table 3), which are markers of mental ill-being and require specific treatment, especially if they were observed in the patient before the onset of insomnia.
Treatment
All patients suffering from insomnia should be educated on the basic elements of good sleep hygiene. Sleep hygiene refers to daily activities and habits that contribute to maintaining good quality sleep and full daytime activity.
Patients must be motivated to follow simple rules:
- It is necessary to develop a regular sleep habit, which means going to bed and waking up at the same time, and not spending more time in bed than is necessary for sleep.
- You don't need to stay in bed in the morning to get enough sleep.
- It is necessary to avoid falling asleep during the day, or daytime sleep should be short, no more than 1 hour, and it is imperative to stay awake after three o’clock in the afternoon.
- It is necessary to maintain a regular daily routine; Regularly taking meals, taking medications, doing daily work and physical activity at the same time, which helps keep the internal biological clock running smoothly.
- No need to read, write, eat, watch TV or talk on the phone in bed.
- No need to drink strong coffee or tea after lunch; You should avoid drinking alcohol within 6 hours before bedtime and you should not smoke before bed.
- You don't want to go to bed hungry, but you also shouldn't eat a lot of food right before bed.
- It is useful to relax before bed (about 30 minutes before bedtime), this can be facilitated by a light snack, a certain ritual before bed (getting ready for bed, listening to calm music or light reading).
- You should avoid vigorous (stimulating) activities before bed (for example, vigorous exercise, discussing a stressful issue with your spouse or partner, or thinking about it with yourself).
- It is necessary to keep the bedroom dark, quiet and at a comfortable temperature.
- Daily physical activity is beneficial; Exercise is best done in the late afternoon or early evening (but no later than 6–7 pm).
- You should not force yourself to fall asleep; if you couldn’t fall asleep within 15–30 minutes, then it’s better to get up and do something relaxing (for example, read a book in a dimly lit room); but the main thing is to try not to look at the clock or worry about the likely consequences of a sleepless night.
Drug therapy is necessary for patients in whom sleep anxiety becomes the most pressing manifestation of the disease state. The presence of sleep-related behavioral disorders and/or anxiety and depressive symptoms in a patient is an indication for drug therapy.
Currently, sedative-hypnotics remain the most frequently prescribed drugs for sleep correction at any age. They can provide symptomatic correction in monotherapy or as an adjunct to the treatment of the underlying disease. All groups of drugs have both certain advantages and disadvantages. There is no ideal sleeping pill today. The choice of a particular drug depends both on the cause of the sleep disorder and on the pharmacodynamics of the drug and the patient’s response to it.
Antihistamines are the most popular over-the-counter medications that have sleep-inducing effects. The histaminergic system of the brain belongs to the group of activating systems. Blockade of type 1 histamine receptors (H1) leads to a reciprocal increase in somnogenic effects and the development of drowsiness [11]. Modern antihistamine hypnotics, such as Donormil (doxylamine succinate), do not cause the residual sedative effect characteristic of first-generation drugs. It has been shown that when taking doxylamine as a sleeping pill, the natural structure of sleep is preserved, there is no addiction or dependence (withdrawal syndrome does not develop). The use of the drug is not accompanied by deterioration of cognitive functions. A significant advantage of doxylamine is the possibility of its use by persons with sleep apnea syndrome. All these qualities make it possible to use Donormil in elderly patients suffering from cerebrovascular insufficiency. On the other hand, Donormil is widely used for the treatment of sleep disorders in individuals with organic and stress-related psychopathological syndromes. An open Russian observational study of the effectiveness of Donormil for sleep disorders in people with borderline conditions showed the high safety of Donormil in combination with psychopharmacotherapy and somatotropic drugs [12]. The results of this study demonstrated that Donormil also improves the quality of morning awakening. In particular, patients reported that they woke up rested, cheerful, and did not experience drowsiness, fatigue, or the desire to lie in bed.
When taking doxylamine, undesirable effects are sometimes possible, such as dry mouth, palpitations, constipation, delayed bladder emptying, and impaired accommodation. Therefore, doxylamine should not be prescribed to persons with benign prostatic hypertrophy.
High efficiency and favorable tolerability make it possible to use Donormil for the symptomatic treatment of sleep disorders in patients with cerebrovascular insufficiency. The optimal duration of treatment is two weeks. During this period of time, the main cause of sleep disturbances should be identified and an attempt should be made to correct it. At each visit, the patient must be motivated to strictly follow the rules of sleep hygiene.
Literature
- Wolkove N., Elkholy O., Baltzan M., Palayew M. Sleep and aging: 1. Sleep disorders commonly found in older people // CMAJ. 2007, 176: 1299–12304.
- Fortier-Brochu E., Beaulieu-Bonneau S., Ivers H., Morin C. Insomnia and daytime cognitive performance: a meta-analysis // Sleep Med Rev. 2012, 16: 83–94.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth. Arlington, VA: American Psychiatric Association; 2013.
- Morin CM, LeBlanc M., Daley M., Gregoire JP, Mérette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors // Sleep Med. 2006; 7 (2): 123–130.
- Mims KN, Kirsch D. Sleep and Stroke // Sleep Med Clin. 2016; 11 (1): 39–51.
- Lavie P., Ben-Yosef R., Rubin AE Prevalence of sleep apnea among patients with essential hypertension // Am Heart J. 1984; 108:373–376.
- Culebras A. Cerebrovascular disease and sleep. Curr Neurol Neurosci Rep. 2004; 4 (2): 164–169.
- Fletcher EC Effect of episodic hypoxia on sympathetic activity and blood pressure // Respir Physiol. 2000; 119 (2–3): 189–197.
- Vorobyova O. V. Treatment of depression associated with cerebrovascular disease (according to the Russian multicenter naturalistic study “RESONANCE”) // Doctor. 2012; No. 12: 26–29.
- Baglioni C., Battagliese G., Feige B., Spiegelhalder K., Nissen C., Voderholzer U. et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies // J Affect Disord. 2011; 135 (1–3): 10–19.
- Haas HL, Sergeeva OA, Selbach O. Histamine in the nervous system // Physiol Rev. 2008; 88:1183–241.
- Smulevich A. B., Pavlova L. K., Zheleznova M. V. Use of the drug Donormil in the treatment of sleep disorders of moderate and mild severity // RMJ "Neurology". 2016; No. 13: 1714–1716.
O. V. Vorobyova, Doctor of Medical Sciences, Professor
FSBEI HE First Moscow State Medical University named after. I. M. Sechenov Ministry of Health of Russia, Moscow
Contact Information
Which doctor will bring back sleep?
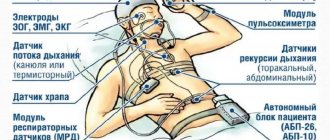
If a person is seriously concerned about a sleep disorder, he or she should contact a somnologist. He must find the root cause of the problem and, if necessary, refer to another specialist. The main type of diagnosis is polysomnography. This is a comprehensive sleep study that records the characteristics of breathing, heartbeat, and bioelectrical activity of the patient’s brain in a sleepy state. The procedure is usually performed in a clinical sleep laboratory.
Polysomnography reliably detects sleep apnea, in which the patient is suffocating and cannot sleep. The procedure allows you to determine heart rhythm disorder syndrome, in which a person wakes up with a heartbeat that is elevated to 150-160 beats per minute. Then he is sent to a cardiologist, and then usually to a surgeon.
Older people often suffer from disturbances in the perception of sleep, when insomnia itself may not exist. Often the patient claims that he has not slept a minute for many years. When the sleep of such a person is studied in detail in the laboratory, it usually turns out that he sleeps superficially, with frequent awakenings, but sleeps through his 6-7 hours a day.
When is sleep disorder especially dangerous?
After just three completely sleepless nights, a seemingly healthy person may experience delusions, hallucinations, attacks of acute psychosis, and epileptic seizures. Seven days spent without sleep ends in guaranteed death. It has long been established that symptoms of insomnia are independent risk factors for heart disease and stroke.
In some cases, sleep disturbance is not even a bell, but a bell signaling a mortal danger to life. Gleb Lutokhin says:
“A strong young man, 28 years old, complains of snoring and sudden cessation of breathing during sleep. At night, the wife had to push her husband away more than 40 times an hour, restarting the breathing process. This is a case of central apnea - a pathology in which the medulla oblongata stops giving the body the command to inhale. Such situations very often end in the death of the patient. As it turned out, the patient had a congenital organic pathology in which the vertebral artery compresses the respiratory center of the medulla oblongata. We have selected the appropriate ventilation option. For the rest of his life, the patient will have to sleep with a device that will control his breathing and breathe for the owner in those moments when he stops doing it on his own. But the patient sleeps well, does not get tired during the day, and has even lost weight.”
Symptoms of insomnia
Insomnia can be easily recognized by a person’s appearance. Insomnia is characterized by redness of the eyes, pale skin, bags under the eyes, and dry lips. A person suffering from insomnia shows lethargy, depression, and in some cases apathy.
The main symptoms of the disease are as follows:
- Difficulty falling asleep, lasting up to several hours;
- Partial or complete lack of sleep at night;
- Light sleep, which does not give the body and psyche proper rest;
- Intermittent sleep or early awakening, after which it is impossible to fall back asleep.
Remember that frequent lack of sleep is dangerous for the body. Insomnia during depression causes disruptions in the functioning of the central nervous system, which is accompanied by irritability and decreased performance. With persistent sleep disturbances, there is a risk of premature death.
When the reason lies in the past
It often happens that the cause of insomnia is an event that happened months or even years before the onset of symptoms. Most often with acute anxiety disorder caused by the death of a loved one. In the first time after loss, insomnia does not occur due to stress and regular adrenaline surges. But when, six months or later, a person relaxes a little, then chronic sleep disorders appear.
Dr. Kolchina says: “A woman over 80 years old encountered the problem of insomnia 3 years after the death of her husband. She tried to regain sleep with the help of alcohol and tranquilizers, although she had never drank before. It was still not possible to get enough sleep, and the patient had problems during the daytime, including impaired motor functions and even falls. In this case, combined drug and psychotherapeutic treatment helped.”
Obese people often complain about the quality of their sleep. They fall asleep easily, but experience breathing problems during sleep due to pulmonary hypoventilation syndrome. Fat tissue puts pressure on the chest, the lungs breathe only due to the diaphragm. As a result, the body receives insufficient oxygen, which aggravates obesity by inhibiting metabolic processes. That's why overweight people often wake up in the middle of the night and don't get enough sleep.
Causes of insomnia due to neurosis, depression, stress
Psychological causes of insomnia include the following:
- Stress associated with the patient’s professional activity, difficulties within the family and domestic conflicts. Under their influence, the patient’s nervous system works ineffectively, resulting in insomnia due to stress;
- Psychotrauma. As practice shows, insomnia, depression, and neurosis go away on their own when a person accepts the problem;
- Strong mental experiences accompanying the loss of loved ones. Of the non-drug methods of therapy, in this case, only time and the support of loved ones help. Often, insomnia after stress is treated by taking antidepressants prescribed strictly by a specialist;
- Personality characteristics. At risk are patients susceptible to anxiety—unreasonable fear. Anxiety before the next day negatively affects the patient’s psycho-emotional state, causing sleep disorders.