Translated from ancient Greek, the term means “split of the mind” or split of the mind,” one might say insanity. But it would be more correct to say “split personality”. Also in early psychiatry, schizophrenic disorder was also referred to as dementia (“dementia praecox”) or schizophrenia. The condition is an endogenous (caused by internal factors) polymorphic disorder of the human psyche, accompanied by the destruction of thinking processes and emotional reactions.
This disorder is characterized primarily by destruction of thinking and perception of reality, which becomes inadequate.
Causes of the disease:
According to modern clinical research, schizophrenia is genetic, that is, it is inherited. However, other theories are also being considered to explain its occurrence:
Neurotransmitter theory
She studies how medications used for treatment, which are collectively called “antipsychotics,” affect patients. This theory includes 3 basic hypotheses:
- Dopamine According to it, the main trigger for the appearance of the disorder is an increased level of the hormone dopamine in the patient. Traditionally, the hormone dopamine has a stimulating effect on the nervous system of a healthy person, but its excess can lead to hyperstimulation of brain activity, which leads to improper functioning of neurons.
- Serotoninova In this case, the cause of the disease is disturbances in the transmission of serotonin through neurons. Receptors begin to work excessively, which ultimately leads to the depletion of certain brain functions.
- Noradrenergic Suggests that the manifestation of schizophrenic symptoms is primarily influenced by the process of decay of neurons that make up the noradrenergic system.
Dysontogenetic theory
Also called the “brain development disorder” theory . Thanks to research, it was found that schizphorenics have constitutional changes in the structure of the brain. It is worth noting that these anomalies are not extensive, so the pathological changes do not progress.
However, in the presence of a stressful or other traumatic factor, the patient may experience decompensation of these structural abnormalities, provoking the development of a mental disorder.
The theory also suggests that the cause of deviations may be complex internal infections, a toxic environment or genetic destruction.
Psychoanalytic theory
It is logical to note that the founder of this approach is Sigmund Freud. He assumed that the disease occurs in people who are closely dependent on the ego, and the origins of such attempts come from childhood. Traumatic situations in childhood and adolescence (cold attitude of parents towards their child) can also be the cause of narcissism and egocentrism, and the symptoms of schizophrenic disorder, including destruction of thinking and delusions of persecution, are their direct consequences.
Genetic theory (constitutional and genetic predisposition)
Some time ago it was believed that schizophrenia, as a disease, has only genetic prerequisites, that is, it is transmitted exclusively by inheritance. There is a significant grain of truth in this conclusion, since the presence of a similar diagnosis in close relatives significantly increases the chances of its development in descendants. Now it is believed that it is not the disease itself that is inherited, but only a predisposition to a number of mental illnesses (alcoholism, epilepsy, suicide, and, in particular), but it can manifest itself or not, depending on the environmental factors in which a person grows.
Theory of internal intoxication (autointoxication and autoimmunization)
It implies that the cause of the development of the disease may be a violation of protein metabolism in the body, and, accordingly, internal poisoning with toxic products that appear as a result of a violation of this metabolism. For example, ammonia, phenol and cresols. Accumulating in the body, they inhibit the correct course of basic processes, which leads to metabolic disorders, the impossibility of timely restoration of the nervous system, and, accordingly, to neurodynamic disorders in schizophrenia.
Cognitive theory
Refers to a cluster of biological hypotheses that consider a biological factor as the fundamental cause that is the trigger in the development of the disease. It is this theory that pays special attention to the study of hallucinogenic symptoms in a patient, which lead to a distorted perception of existing reality.
Infectious theory of genesis of schizophrenia
It assumes the development of the disease as a result of a combination of chronic and acute (usually conditionally pathogenic) infection and, accordingly, inhibition of protective immunobiological mechanisms.
In simpler terms, the reasons can be described as:
- heredity;
- perinatal period (disorders of fetal development in utero);
- destructive social environment (urbanization, low standard of living);
- psychotrauma received in early childhood;
- unfavorable environment;
- brain injury (considered perinatal or early natal periods);
- chemical dependencies (alcoholism, drug addiction);
- any severe stress, anxiety and shock.
The importance of rehabilitation for schizophrenia
This is mainly due to refusal to undergo rehabilitation for schizophrenia and take maintenance therapy. Violation of the regime during rehabilitation for schizophrenia, independent, uncontrolled reduction of doses of medications taken. The easiest way, of course, is to blame patients for lack of consciousness, placing all the blame on them for the next relapse of the disease. However, considerable blame for the current situation still lies with doctors and the healthcare system as a whole.
Often, after discharge from a psychiatric hospital, a patient undergoing rehabilitation for schizophrenia finds himself virtually left to his own devices and unable to continue to cope with his illness. He faces wary glances from his family and work colleagues or even tries to hide the fact of his hospitalization.
He is left alone with fears for his future, which often seems uncertain. In this case, there is a risk of severe mental illness, such as psychosis, the treatment and rehabilitation of which should be carried out in a specialized hospital.
In addition to such “vivid” symptoms as delusions and hallucinations during an attack, schizophrenia can manifest itself as mood swings, causeless anxiety, and peculiar personality changes. It becomes difficult for patients to communicate with people and correctly understand the world in general.
Thus, the patient needs support and rehabilitation for a long period after the acute episode. Help in the recovery of patients with schizophrenia consists, first of all, in informing the patient and his relatives about the course of the disease and debunking “myths” about the disease.
What kind of rehabilitation is needed for schizophrenia?
A person suffering from schizophrenia often does not fully understand the depth of damage to his psyche, so his closest relatives have to monitor his health, nutrition, appearance and adaptation in society.
Often, if a person does not undergo rehabilitation for schizophrenia, the patient’s personality is destroyed to such an extent that he is not capable of independent life, work and starting a family. In this case, disability due to mental illness is issued: the patient is assigned a pension depending on the group and other social benefits are added. For 5 years, the patient must undergo a medical-labor expert commission annually, undergo rehabilitation for schizophrenia, take prescribed medications and regularly visit his doctor. If after 5 years the condition is not restored, then disability is assigned for life. In the absence of visits to a psychiatrist and refusal of recommended treatment, such behavior of the patient can be interpreted by the medical commission as recovery. In this case, the disability is not extended.
The main rehabilitation for schizophrenia is ensuring regular examinations by a psychiatrist, monitoring the intake of antipsychotic medications, maintaining physical health and undergoing socio-psychological rehabilitation. Such complex therapy can be obtained at the Preobrazhenie Clinic.
Patients need rational employment that allows them not to drop out of society and to feel needed and useful for society. Finally, psychotherapy has an important influence in the rehabilitation of patients with schizophrenia, allowing the patient to understand his illness and consult a doctor in a timely manner to prevent relapses, and adapt to the world around him.
Symptoms and signs of schizophrenia
It is quite difficult to determine this disease on your own. Simply the presence of a neurotic state, even if accompanied by pre-hallucinations and delusions, is not yet a stable sign of schizophrenia. The disorder can only be determined by a specialist using special tests. However, there is a primary set of “outpost symptoms” that help identify deviations in the early stages. These symptoms can appear in a person a certain time before the development of the disease itself.
So, early symptoms of schizophrenia:
In most cases, there is a change in hygiene habits (a person becomes unkempt, stops taking care of himself), indifference to the opinions of others appears, social maladaptation of the individual is observed, as well as aggression, inappropriate emotions, unreasonable suspicion, changes in facial expressions, sleep disorders, problems with attention and concentration, disorganized speech, prodromal phenomena, such as a narrowing of the range of interests, changes in personality traits, a person’s feeling that his self has changed, sometimes a decrease in intellectual abilities (a decrease in the motivational factor and volitional component). Bipolar affective disorder very often serves as a harbinger of the development of schizophrenic disorder.
Ambivalence, when the patient simultaneously experiences two opposing feelings or emotions, can also be called a bad symptom. Now he loves, and a few minutes later he hates it; yesterday he liked ice cream, for example, but the next day he didn’t, and so on.
In some cases, on the contrary, the acquisition of certain oddities in behavior is observed: strange hobbies and extremely valuable ideas appear.
General symptoms of schizophrenia
Signs of schizophrenia:
- Violation of logical connections and sequences of actions in social and everyday life. For example, the patient does not take care of his body and personal space because he does not see the point in it.
- Violations of verbal functions and speech saturation. The patient begins to speak very slowly and in monosyllables, and is unable to give a detailed answer to the question.
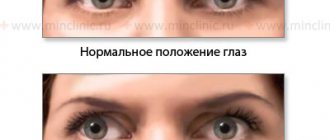
- A decrease in emotional manifestations, up to their complete absence, expressionless facial expressions, glassy eyes, avoidance of eye contact.
- A sharp drop in concentration level, the patient is unable to concentrate.
- Anhedonia is a complete loss of interest in past hobbies. Considered as an early sign of the disease.
- Affective states. Absolute inadequacy of reactions to various situations. Laughing at someone else's grief or crying for no reason.
Positive symptoms of schizophrenia
- Hallucinosis
It can manifest itself verbally, visually or at the level of sensations.
The patient begins to see, hear or feel phenomena that do not exist in reality. For example, he may look around, listen to non-existent sounds, plug his ears, or talk to someone in an empty room. In the initial stages of the disorder, hallucinations do not appear so often, but as the disease progresses, the condition worsens.
- Obsessive thoughts and ideas
The patient is unable to separate the existing reality from his sick fantasy, which leads to the emergence of destructive thoughts that he is unable to cope with. For example, he may firmly believe that he has a meeting with Napoleon at 15.33. Moreover, he remains absolutely stubborn in his conviction and reacts very aggressively to attempts by those around him to dissuade him.
- Violations of logic and thinking functions
Neural imbalance leads to the inability to think logically and build connections between events, rules or phenomena. Thus, a schizophrenic ceases to understand why, for example, one should not go to a red traffic light or should not sleep on railroad tracks.
- Psychomotor agitation
It manifests itself in mixed, chaotic, sometimes destructive movements, inability to control one’s body, as well as speech function. A person with schizophrenia may break furniture, bang his head against the wall, shout incoherent phrases, and not notice or be aware of the strangeness of his behavior.
- Rave
Clusters of delusions include such conditions as delusions of persecution or delusions of hidden negative influence. In other words, a person believes that he is being affected by some device, waves, radiation or some kind of chemical agent that is sprayed into the air for a harmful purpose. There is also delusion of attitude, when a person thinks that everyone around him is conspiring against him, and he is in the center of some kind of conspiracy, and everyone around him treats him badly, thinks badly of him, his thoughts become known to others, as if broadcast like a radio. Often the patient thinks that he can read other people’s thoughts and knows the content of the selfish plans of others. The person expresses all this uncritically, and it is impossible to convince him otherwise. He is absolutely confident that he is right, which is negative.
How to communicate
One of the symptoms of schizophrenia is the desire for loneliness. Withdrawal becomes especially pronounced after psychosis or immediately before its development. For this reason, leaving the patient alone for a long time is not recommended. It is advisable to talk to him more. Conversations on abstract or interesting topics for the patient will prevent him from immersing himself in his inner world.
We can formulate several basic rules for communicating with a schizophrenic:
- Speak more slowly. Remember that the person may have impaired cognitive function. Perhaps he absorbs information worse. But at the same time, you should not treat him like a child, explaining everything in too much detail. He should not sense a patronizing or didactic tone in your voice.
- Don't criticize. Communicating without arguments is difficult even for healthy people. Often close friends quarrel over different religious or political beliefs. You should not get into verbal altercations with a schizophrenic. Also try not to criticize his judgments, even if they seem absurd to you.
- Don't raise your voice. Screaming and swearing cannot contribute to normal communication. The conversation should be productive. It is impossible for the patient to withdraw into himself after the conversation and begin to replay the quarrel in his head ad infinitum.
- Don't forget about the patient. Never talk in front of a patient as if he were not there. In most cases, he understands everything perfectly, since he is conscious. If you need to talk to someone about a patient, do it in their absence.
- Do not increase the patient's delirium. He may feel like he is being followed. Don't text other people in his presence. Don't laugh at megalomaniac delusions. Develop a behavior plan in case the patient has a panic attack. Let's say he believes that the intelligence services are watching him. Don't try to convince him of this. He will stop trusting you. Better listen and try to understand how to help him.
It is necessary to separate the person and his disease. He probably will not tolerate a condescending attitude. He also won't like being treated like a child. In a state of remission, a schizophrenic is often no different from ordinary people. He can work and even raise children.
Schizophrenia does not prevent some people from getting married, working, and getting doctorates.
An unusual attitude towards a patient will emphasize the “unusuality” of the patient himself. This will interfere with socialization. If you remind him in one way or another that he is sick and he can’t do something, he will never be able to feel like a full-fledged member of society.
Pathogenesis of schizophrenia
Pathogenesis, namely the process of initiation and development of the disease, is quite complex. As was clarified above, the main cause of the disease is due to a genetic factor, which also includes such circumstances as a complicated pregnancy, addictions of one or both parents, psychological or physical traumatic situations during fetal development and in the first months after childbirth. In the future, the development of the disease can be influenced by negative social factors (dysfunctional family, poor care, etc.).
In the case of increased neurotoxicosis (neuronal damage to the brain), degenerative changes in the brain may increase.
So, at the moment, classical psychiatry is studying both exogenous (external) and endogenous (internal) mechanisms that influence the occurrence and development of schizophrenic disorder. Of greatest interest are precisely those hypotheses and theories that consider the results of both clinical and experimental studies at the same time.
Diagnostics
According to statistics, the disease manifests itself most often in adolescence. If there are certain triggers, you can feel the disease at a fairly young age. The onset of schizophrenia is usually observed before the age of 30–35 years.
Prussian psychosis
As noted above, the first symptoms of the disease appear at a young age; schizophrenic disorder does not appear in the second half of life. Acute psychosis in elderly patients is classified in psychiatry as “cyanotic psychosis” rather than schizophrenia. However, its symptoms are quite similar to those of schizophrenia. Hallucinations and delusions may occur. But, most likely, they will be of a vascular nature: vascular dementia, brain destruction (Alzheimer’s, Parkinson’s or Pick’s disease). In any case, such organic brain lesions are not related to schizophrenia. Quite often, the differential diagnosis of schizophrenia causes significant difficulties. This is especially true for the initial stage of the disease or periods of deep remission, as well as when one person combines alcoholism and schizophrenia or has suffered psychotrauma against which pathology has developed. Thus, within the framework of the differential method, it is quite difficult to determine the disease on your own. As noted above, not every symptom characterizes this particular disorder. But a person cannot suspect schizophrenia in himself, since this is associated with a loss of criticism.
He may, for example, discover depression or neurosis and, in connection with them, go to a specialist, who, in turn, should conduct a more detailed study and prescribe medication. But, unfortunately, the disease is often noticed by the patient’s relatives at fairly late stages and they are hospitalized in an acute condition, because advanced symptoms are most often interpreted as coincidences or coincidences, or as a consequence of stress or neurosis. Thus, everyone expects that they will go away on their own, and if they take medications, they are more likely of homeopathic or herbal origin, which do not cure the disease, but simply help to prolong it. Thus, due to incorrect diagnosis and late diagnosis, schizophrenic psychosis most often debuts in the patient in an acute form.
Differential diagnosis of the disorder
An important stage of diagnosis is the differentiation of a schizophrenic attack from a neurotic or other mental disorder, as well as the rejection of diseases of an infectious nature that have a destructive effect on neural connections.
For example, an acute psychosis or manic episode, also identified as a polymorphonic psychotic disorder, can also unfold against the background of other diseases, for example, within the framework of schizoaffective or bipolar disorder, which can serve as precursors, but in general are not related to schizophrenia, since they are to another cluster of diseases, a cluster of mood disorders. Bipolar affective disorder, for example, has a more favorable prognosis for life and work. However, even an experienced specialist can sometimes confuse the state of acute psychosis in a neurotic or other disorder with a schizophrenic coat (schizophrenic psychosis). That is why it is very important to observe a person with a team of specialists and in dynamics. The patient’s condition after recovery from acute psychosis is of great importance, since only the stagnation phase makes it possible to more clearly differentiate schizophrenia from other mental disorders.
How to properly persuade a patient to undergo rehabilitation
- Gain the trust of the sick person and establish good contact with him (he should not be afraid or neglect you).
— Play along in some situations, confirm that you also see hallucinations and are “on the same wavelength” with him. Just don't overplay it, otherwise it will have the opposite effect.
— Determine what symptoms are bothering the person (for example, pain or dizziness, nausea, insomnia). It is these factors that should become a reasoned reason for contacting a psychiatrist.
Many people with mental disorders are most afraid of ending up in a “psychiatric hospital.” Therefore, one cannot focus on this, creating the most favorable conditions for a person. After the appointment, the specialist doctor will indicate exactly how to begin treatment.
Criteria for diagnosing schizophrenia according to ICD-10
ICD-10 - International Classification of Diseases.
Schizophrenia, as a disease, belongs to a cluster of endogenous (those caused by internal factors) disorders. According to ICD-10, it belongs to class V, which means mental and behavioral disorders; The diagnosis of schizophrenia is classified as f 20, namely schizotypal and delusional disorders. They are usually characterized by serious constitutional defects in thought processes and reflection of reality, as well as inadequate reactions. The ability for intellectual activity is usually preserved, but over time there may be a decrease in the ability to cognition and remember information.
The course of the disease can be long-term episodic, including periods of remission, stabilization or worsening of the condition. It is worth noting that in the intervals between attacks the person is practically healthy. Therefore, in the scientific community, the disease is not defined as schizophrenia, but as schizoaffective disorder.
We bring to your attention an interview with Sergei Ernstovich Medvedev. Sergey Ernstovich - psychiatrist-psychotherapist, candidate of medical sciences, doctor of the highest category, family therapist, member of the Society of Family Consultants and Psychotherapists, presenter of the seminar “Family psychotherapy for mental disorders (schizophrenia, autism, bipolar disorder).”
— Sergey Ernstovich, according to available information, laboratory diagnostics for this disease do not exist, so how do specialists manage to recognize schizophrenia?
— You are right, there are no laboratory diagnostic methods at the moment. The diagnosis is determined by a council of psychiatrists according to the criteria of the current International Classification of Diseases (ICD).
The emergence of the concept of “mental illness” and the emergence of a medical model in psychiatry were progressive. It allowed specialists to begin studying this phenomenon from a scientific point of view. This model also has a lot of disadvantages. Various variants of the course of schizophrenia are identified, the diagnostic framework is expanded and narrowed. Many people criticize modern psychiatry for this vagueness, often quite rightly. There are even experts who call for abandoning the term “schizophrenia” altogether. So in Japan, instead of the previous term “seishin-bunretsu-byo”, translated as “disease of the split mind”, since 2004 the term “tōgō-shitchō-shō” has been used, meaning “integration disorder”. Now in psychiatry there is a replacement of other terms that were widely used in the past. So in the modern current classification there are no longer such diagnoses as “moronism”, “imbitility”, “idiocy”, “hysteria” and so on, since these terms have turned into stigmas over time. I think this is the right approach, since psychiatry should be focused on the consumer of mental health services, and the consumer in this case is the mentally ill person and his family.
— But is the family a consumer in this case? Indeed, in our country, according to the law, the treatment of such patients should be carried out by the state, and not by relatives: mental illnesses are diseases that are subject to compulsory health insurance.
— Indeed, in Russia, state health care institutions provide assistance to mentally ill people by law, but the state fails to satisfy all the needs of such people: it provides psychiatric care, which may consist of hospitalization and the prescription of pharmacotherapy. Psychological assistance for this category of patients, and especially psychotherapy, is not included in the list of services subject to compulsory health insurance. Therefore, patients with mental illness receive psychological help, alas, much less often than they need.
Nevertheless, psychotherapists work with patients with schizophrenia and, often, very successfully. Here we touch upon a very important problem, which is worth talking about in more detail: the problem of interaction between two specialists - a psychotherapist (psychologist) and a psychiatrist - who work with the same patient. Modern assistance to a mentally ill person should be comprehensive. This means a combination of biological treatment methods, which are owned by a psychiatrist, and psychologically oriented methods, which are owned by a psychologist and psychotherapist. If I, being a psychotherapist with a medical education and knowing medications, interfere with the prescriptions of the attending psychiatrist, then I will enter into competition with him, and this will inevitably reduce the effectiveness of assistance to both the patient and his family. If a psychiatrist discusses and criticizes my psychotherapeutic interventions with a patient, then conflict is also inevitable. The effectiveness of work decreases if one of the specialists tries to take over everything and says, for example, that schizophrenia should be treated exclusively with psychotherapy or, conversely, says that psychotherapy is not needed for a patient with schizophrenia and is even contraindicated, only medications are sufficient. Psychopharmacotherapy has indeed achieved a high level of effectiveness and is safe when used in a qualified manner, but one cannot expect from drugs what they cannot do.
- What exactly can’t they do?
“Medicines will help improve the patient’s condition, but they cannot replace psychotherapy. Here we return again to the medical model of schizophrenia. It played a positive role: thanks to the emergence of this model, mentally ill people began to be treated more humanely, because if we consider schizophrenia a disease, then we must extend to it all other provisions that relate to diseases. And the modern bio-psycho-social approach in medicine implies that a person needs to be helped by biological means (for example, prescribe medications, if necessary), help solve psychological problems and help adapt socially. That is, the modern model includes a combination of different approaches. Psychological help can be useful not only to the person himself, but also to his family.
Psychological well-being is part of the concept of “health”; it is no less important than a person’s physical condition. And this applies not only to mental illness. The psychological state of the patient directly determines whether he will comply with the doctor’s orders. This is true for any field of medicine - traumatology or ophthalmology, for example. I deliberately do not mention such specialties as neurology, cardiology and gastroenterology. In these areas of medicine, the need for psychotherapeutic help is obvious to everyone.
I work at the Medical University General Hospital. There are 9 buildings in it, 7 of them are medical buildings and attending physicians from each building refer patients to me. Psychological assistance helps reduce treatment time, improves its results and, ultimately, improves the quality of work of doctors.
“And this is also beneficial for the state, since the length of a person’s stay in the hospital is reduced.
- This is extremely beneficial for the state! Under the guidance of Professor Edmond Georgievich Eidemiller (one of the founders of family psychotherapy in the USSR), I conducted a study called “Features of analytical-systemic family psychotherapy and the dynamics of psychopathological adaptation and family indicators in patients with paranoid schizophrenia.” The dissertation was defended at the NIPNI named after V. M. Bekhterev
This study proved that conducting, on average, about 20 sessions over six months (in the format of analytical-systemic family psychotherapy) leads to a reduction in the number of re-hospitalizations within a year by almost half. Maintaining a patient in a psychiatric hospital - with bed days, food and expensive medications, with salaries for qualified staff and various allowances for harmfulness - is very expensive for the state. Reducing re-hospitalizations leads to lower costs for the treasury. In addition, successful therapy helps to increase the social competence of mentally ill people; they completely or partially refuse government benefits and get a job. This study shows that psychotherapy can be used as an effective and cost-effective way for the state to rehabilitate mentally ill patients.
4 years have already passed since the start of the study and we had the opportunity to observe the patients’ condition over time. Those patients who maintain contact with a psychotherapist (no more than once a month) and take prescribed medications have never been hospitalized during this time. This is natural: walls don’t heal, drugs do. In some developed countries (for example, Germany), the 20 sessions required to rehabilitate the patient and restore his social competence can be covered by insurance. For neuroses and borderline disorders in the West, more than six sessions will not be paid for, but for severe mental illnesses, the patient and his family can receive up to 20 sessions through insurance.
In the West, mental health care is being deinstitutionalized. This means moving away from institutional psychiatry and minimizing hospital stays.
Public funds are used more effectively when modern drugs are used, which help achieve remission more quickly, often allowing the patient to return to pre-disease levels of functioning. Psychotherapy helps to increase the level of social competence of the patient and improves drug compliance. The patient does not refuse medications, but finds a place for them in his life and the medications do not interfere, but rather help him live. A person begins to treat his illness consciously: “I have some features of my psyche that force me to avoid certain things, adhere to certain rules and take medications.” This approach is applicable not only to mental, but also to somatic diseases. For example, there are diabetic patients who constantly take insulin. Many of them live active lives. Why shouldn't a mentally ill person who is properly informed about his or her health and receiving treatment also lead an active lifestyle? This is quite possible and psychotherapy can help increase the level of his adaptation.
— Why did you turn to systemic family psychotherapy when researching and treating schizophrenia?
- Because it's effective. There are many myths associated with a disease such as schizophrenia. For example, there is a myth that psychotherapy is unnecessary or even harmful for schizophrenia. I was faced with the fact that colleagues said with horror: “What will I do there? This is schizophrenia!” However, in a systematic approach, there is no fundamental difference between working with the family of a mentally ill person and a mentally healthy person. In all forms of schizophrenia, psychotherapeutic assistance to the family is not only possible, but also indicated. The fact that not everyone knows how to do this does not make the approach itself bad.
It is important to note that the word “systemic” is currently used unnecessarily widely. In this case, “systemic” means psychotherapy based on the principles of General Systems Theory. From the perspective of systemic family psychotherapy, the problem lies not in the specific symptoms of one of the family members, but in the functioning of the family system as a whole. This is the advantage of a systematic approach to schizophrenia. The psychotherapist will also take into account the impact of the narrative about mental illness on the new reality created for the family.
I will give a clinical example from my own practice, which is also described in the form of a situational task in the chapter “Family psychotherapy for schizophrenia” of the workshop edited by Professor E. G. Eidemiller “Systemic family psychotherapy”. It will be out of print soon.
Twenty-six-year-old schizophrenic patient Ignat was transferred from one psychiatric department to another because he kept getting into fights with patients. A young man of asthenic build chose the strongest and tallest man in the department as his opponent. When asked why he was doing this, he replied that he thought he had to fight because otherwise he would be considered a homosexual and his mother would be raped. Coming to the department, I met nurses, nannies and patients, vying with each other to talk about the strange things that Ignat told them about today.
At the reception, he told me about these and his other painful experiences, singling them out from all the others and, as it were, complaining about them. For example, he said: it seems to him that his mother is a cannibal and she ate his father. Each time I listened carefully to his story, I invariably praised him for the fact that, despite his painful condition, he found the strength to identify these thoughts as painful and tell me about them. That is, I focused specifically on the healthy part of his personality and resources.
In fact, in communicating with me, he reproduced his usual way of interacting with people significant to him. There was a lot of tension and contradiction in his relationship with his mother. On dates in the hospital, he told his mother about his painful thoughts, and she, in horror and anger, tried to forbid him to talk about it, scolded Ignat and tried to distract him, avoided coming to his meetings. However, at her next visit, Ignat again greeted her with a new portion of “thoughts.” Tension accumulated and was released through emotionally charged conflict explanations. By exploring their interaction and suggesting a positive connotation, and then prescribing a paradoxical ritual, I was able to reduce the emotional tension in this relationship.
At one of the meetings, he told me: “You know, Sergei Ernstovich, I think that you will now rape my mother, and she will like it.” I asked him why he was talking about rape. He tensed and, clenching his fists, approached me. “Now I want to hit you.” I thanked him from the bottom of my heart for telling me what I wanted, but not doing it. I told him that he was a young and strong man, and if he really hit me, I would feel very bad. I drew his attention to the fact that he found the strength to recognize his impulse and tell me about it.
At this moment, our roles were determined: he is a man, and I am another man, a representative of another generation, and I can be in the same world with him, I can even be close to his mother, and he and I can talk about it. An additional boost to his resources was that I recognized his masculinity and strength. Ignat calmed down and sat down in his original place. After sitting for a while, he got up and went to his room. After that, he canceled several meetings, notifying me by phone a day or two in advance. Psychotherapists working with mentally ill people will confirm that psychotics usually do not show initiative in communicating with a psychotherapist and can easily oversleep an appointment. And this patient called me every time the day before to reschedule the consultation! And we rescheduled four meetings (a month passed). Then the three of us met, together with his mother. He was very collected and serious. He told me: “I refuse further studies. You are not working with me correctly: you should have explained to me from the very beginning that no one is going to rape my mother, that she is already 60 years old, that I do not have to do anything to protect her. Why didn’t you tell me about this right away?” I replied, “Perhaps if you understand your situation so clearly, it doesn’t matter so much how I view it?”
Doctors began to note a gradual improvement in his mental state, calmness and orderliness of behavior. Some time after this he was discharged. I know he is currently taking medication and seeing a doctor as an outpatient.
Of course, in order to work with difficult cases, some preparation is needed. Knowledge of psychiatry and systemic psychotherapy is required, as well as supervision and personal therapy. The psychotherapist must be well aware of his own family history and deal with his “skeletons in the closets.” This allows, in particular, to understand the processes occurring in the family of a mentally ill person. It’s time to get rid of the misconception that schizophrenia is the only disease in the entire nosological classification that does not require psychotherapeutic help. It is a myth.
Interviewed by Yulia Smirnova
Interview with psychiatrist Natalya Yuryevna Korchagina “If a psychologist begins to suspect that a client’s problems are related not only to a traumatic situation, it is better to play it safe and send him for a consultation with a psychiatrist”
Pathologies of schizophrenia
Main psychopathic symptoms:
A feeling of “mirroring” thoughts (mental echo), detection of other people’s thoughts or loss of one’s own, replacement of thought processes, belief in the possibility of transmitting thoughts at a distance, delusions of various pathogenesis, asthenia, auditory, visual or verbal hallucinosis, affective suspicion, aggression and negativism. In some cases, a symptom of staging is very characteristic of the patient, for example, when a person says that some kind of performance is being played around him, all around people are hired actors, as if some action is taking place on stage, especially for him. A person experiences very vivid emotions: fear, anger, or, conversely, sexual disinhibition may be observed. Various bodily sensations may occur, such as a feeling of heat throughout the body or heat in the head.
Stages of schizophrenia
In the formation and progression of the disease, 4 main periods are defined, characterized by certain symptoms.
Basic periods of the disease:
- premorbid period;
- prodromal period;
- period of the first psychopathic episode;
- remission.
Premorbid period
At this stage, changes in the patient's character and personality traits may be observed. A person becomes overly tense, strange, hyper-emotional, overly suspicious, and others.
Prodromal period
Characterized by the destruction of connections with the outside world: Withdrawal, coldness, asociality, inability to concentrate, absent-mindedness, loss of interest in social life and family. Often, physiological changes in the brain begin in this phase.
Period of the first psychopathic episode
This stage is characterized by all the positive symptoms of the disease: such as delusions, obsessive thoughts and ideas, hallucinations of various types (visual, auditory, tactile or verbal).
Remission
In remission, the patient experiences a disappearance or weakening of characteristic symptoms for varying periods of time, sometimes long. However, aggravation cannot be avoided. Sooner or later, the patient is faced with the return of old or the appearance of new symptoms.
Defect concept
The defect in schizophrenia refers to mental, biological, social and emotional changes. There is a decline in any needs, apathy and indifference to everything appear, even to those things that previously aroused interest and satisfaction. By and large, the defect is defined as the terminal stage of a schizophrenic disorder. And the main goal of therapy is to delay its appearance. The state of the defect becomes clearly noticeable at the patient’s bodily level. There is a mask-like, emotionless, cold face, and immobility of facial expressions. The person seems to be detached, and those around him do not touch or touch him in any way, no matter what happens. Changes in motor functions appear. Most often, such violations are characteristic of the catonic form, which will be discussed below.
Special forms of schizophrenia
Special forms of the disease imply its intensive development. Most often, a patient comes to the hospital and first comes to the attention of a psychiatrist in the acute form of the disorder (acute psychosis). In such a situation, a person’s behavior changes, he behaves aggressively and can be dangerous to himself and others, he can express various delusional, paranoid ideas that are completely unrelated to reality, and also hallucinate profusely: these can be visual and auditory hallucinations that visible from the side with the naked eye. It’s impossible not to notice this anymore.
Special forms are classified as: hebephrenic, catonic, paranoid and febrile. Let's talk about them.
Hebephrenic form
This type is characterized by a state of passion and emotional disorder. The first symptoms usually appear during adolescence. The patient’s behavior becomes extremely strange, one might say feigned, inappropriate to the situation, and sometimes mannered. Positive signs of the disease (hallucinosis and forms of delirium) are not so noticeable, but negative symptoms (social isolation and problems and destruction of adaptation) quickly develop. The prognosis is most often unfavorable, as it is one of the most progressive forms.
Catonic form
Mostly, the clinical picture is characterized by various disturbances in the patient’s movements, differing in polarity, in other words, periods of exaltation (hyperactivity) can be replaced by numbness or catatonia (stupor). The patient may remain in stupor for quite a long time (up to several days), and then suddenly fall into exaltation. It is in this form that such a symptom as the “look of a schizophrenic” clearly manifests itself. The patient has a strange look, frightened, inadequate, sometimes glassy, staring at one point. However, the prognosis in this case is more favorable and depends on the combination of positive and negative symptoms.
Paranoid form
One of the constitutive signs of this form is paranoid delusion. There are a huge number of types of delusions: delusions of persecution, delusions of threat, delusions of grandeur, etc. Often, the concepts of delusion can be combined with each other, for example, the patient believes that he is under dangerous surveillance because he is a millionaire or a popular person. Most often, delirium is accompanied by hallucinosis.
Febrile form
In the history of febrile form, disturbances are observed at the body level, for example, an increase in temperature up to 39 degrees Celsius, the distinctive feature of which is the lack of response to antipyretic drugs. Also, it is worth paying attention to the patient’s appearance: the skin becomes dry, redness or general redness is noticeable, tearing or an unhealthy shine in the eyes, etc. In relation to psychopathy, affectivity, feverish movements, aggression, up to clouding of consciousness and toxicoderma (violation of the integrity of the skin) are manifested. This is the most dangerous form, the mortality rate of which can reach 50%.
Common misconceptions and “myths” about schizophrenia.
- A diagnosis of schizophrenia is an end to your future career, family life and relationships.
- Schizophrenia leads to dementia.
- Any psychosis with delusions and (or) hallucinations is a manifestation of schizophrenia.
- There is the best cure for schizophrenia.
- In hospitals, people with schizophrenia are turned into “vegetables.”
- Patients with schizophrenia are dangerous and should be isolated.
- Schizophrenia is “contagious” and can be passed on to others.
- You can diagnose yourself with schizophrenia.
Author: Filashikhin V.V. psychiatrist, Ph.D.
Types of schizophrenia
Species gradation is carried out according to the severity of symptoms and stage of development. The disorder usually begins with a simple (weak) sluggish form. A sluggish or poorly progressive form implies a stable course of the disease with mild symptoms. There are no acute sudden attacks. A diagnosis can only be made based on indirect clinical signs, which are sometimes quite difficult to distinguish from ordinary neurotic symptoms.
Progressive - includes two more types of disease: paroxysmal and continuous. The debut occurs after 25 years, but in certain cases the pathology can manifest itself earlier. In this subtype, the disease develops slowly and gradually, but the attacks themselves can be very acute, or the primary symptoms are pronounced.
Continuous flow
It is a complex concept that combines several forms. Moreover, the influence of environmental factors (endogenous) in this case is minimal. The destruction process itself begins extremely gradually, but remissions, as such, are practically absent. Sometimes the symptoms become less noticeable, but they never completely disappear.
Paroxysmal course
Or, as they also say, acute polymorphic disorder progresses over a couple of days, and then can last up to several weeks. Key symptoms: sleep disorder, anxiety, deconcentration, general extreme emotional lability, for example, causeless phobias (attacks of fear) are replaced by euphoric affect, joy and laughter alternate with crying and complaints. From time to time, patients with schizophrenia experience hallucinations and pseudohallucinations: voices sound in the patients’ heads, or they can sort through things, mutter something under their breath, and make secret notes.
Treatment and prevention of schizophrenia
Treatment of schizophrenia is a rather difficult task, since it can take years to destroy the structure of delusion in the patient’s brain, and moreover, complete healing is impossible to achieve. It’s good if a person becomes aware of his condition, but most often this also does not happen.
A diagnosis of schizophrenia in itself does not entail any consequences. At the initial stage, this is most likely only registration at a dispensary at the place of residence, and then only if the person is taken by ambulance to a city hospital of municipal subordination.
In general, a schizophrenic during periods of remission is not particularly different from an ordinary person, he behaves and speaks normally, he can work, for example, and communicate in deficit states (a period of remission, not acute psychosis).
Many people ask the question: Is hospital treatment necessary?
Each case of the disease is individual, but in general, with a favorable prognosis, it can be treated on an outpatient basis, that is, inpatient treatment is not required.
It is necessary to register with the dispensary and check in at certain intervals, but in the future the person has the right to withdraw from this registration. It all depends on the prognosis, which is different for everyone. The underlying factor depends on the specific course of the disease. As discussed above, the course can be continuous, paroxysmal, and even episodic. The episodic course is the mildest form, in which psychosis occurs very rarely, and in principle a person can suffer from schizophrenia, but continue to work and have a family. In such cases, drug therapy is used, which significantly reduces the possibility of developing an attack.
There are also modern treatment methods and drugs that do not cause serious side effects and give a good prognosis for the future. Unfortunately, the patient can take these medications for the rest of his life, which provide a reasonable quality of life.
Thus, the diagnosis of “schizophrenia” is not a death sentence, just like diabetes mellitus or bronchial asthma. Moreover, schizophrenia is not fatal. The lethal outcome is minimal, with the exception of possible suicide during psychosis.
Progressive form of schizophrenia and treatment
The progressive form implies the absence of a positive effect from treatment. In other words, a person is treated for a long time and unsuccessfully, since psychoses continue to recur. In this case, so-called anti-resistant methods are used, including both medicinal and non-medicinal methods of treatment.
Medicinal methods
This is taking certain medications in accordance with a regimen developed by a psychiatrist, which helps relieve resistance. Resistance is understood as a decrease in the pharmacological effect of a drug in a patient, which leads to a decrease in the effectiveness of treatment. Thus, if drug therapy does not produce results, then the next step is hardware methods.
Apparatus therapy
transcranial magnetic stimulation of the brain and electroconvulsive therapy. Impact on brain neurons using currents and magnetic fields. Previously, atropine comas and insulin comatose therapy were also used. very expensive material. Insulin treatment, by the way, is a very good method, but incredibly expensive to use. In the USA and Europe, electroconvulsive therapy is quite popular at this stage. It is worth noting that this particular method was stigmatized for many years, as it was recognized as inhumane, but now this type of treatment is carried out under general anesthesia. The patient does not experience any suffering, and the effect is positive due to the fact that there is a direct effect on the blood vessels of the brain, the permeability of the blood-brain barrier increases, and thus the drugs quickly and effectively reach the receptors. Also, this method is often used before prescribing medications if the patient is admitted in psychosis, allowing the psychotic state to be stopped independently.
Psychotherapy
Throughout life, when treating and stopping the disease, it is necessary to take into account all factors: biological, psychological and social. Implementation of biopsychosocial surveillance is possible only under the close supervision of a team of specialists, including a psychiatrist, psychotherapist, and clinical psychologist. Working with such patients must be done very carefully. In this aspect, positive psychotherapy is ideal within the framework of the Self - a concept where the patient works with and addresses his healthy part. Another important point in treatment is socialization, since the symptoms of the disease affect the everyday areas of the patient’s life. Literally speaking, an encounter with aliens or Napoleon should not interfere with brushing your teeth, washing clothes, maintaining a routine, and performing other everyday tasks.
Treatment of schizophrenia in Moscow
Treatment of schizophrenia in Moscow can be considered quite developed. In the capital of Russia, a considerable number of clinics are engaged in the treatment of this terrible disease, however, the specificity of this disease determines certain conditions necessary for truly effective treatment:
- Possibility of inpatient treatment, since schizophrenia requires long-term therapy. In addition, often the causes of the disease may be in the patient's family, so that his isolation often has a beneficial effect on the treatment of the disease;
- Availability of a rapid response team of psychiatrists ready to come to the rescue during an exacerbation of the disease;
- Availability of specialists in the field of psychiatry with solid experience in this field;
- The most modern and safe methods of treating schizophrenia.
All of the above conditions are available in the professional Moscow clinic Rehab Family, whose experienced specialists are always ready to help your loved one.