Periodic (transient) or permanent (increasing) circulatory disorders in cervical osteochondrosis are a common complication of degenerative dystrophic disease of the intervertebral discs. Due to the fact that the clinical picture develops very slowly, the patient does not pay attention to changes in his condition. Gradually, constant drowsiness, apathy, and headaches become “habitual” phenomena. The search for the cause begins in a completely different place. But in fact, this is a complication of long-term cervical osteochondrosis.
In this article, you can learn about how cerebral circulatory disorders develop in cervical osteochondrosis, what causes this pathology, which doctor you should contact for help, and what methods can be used to completely restore impaired blood flow. The first thing to remember is that no pharmacological drugs will help improve the process of blood supply to the cerebral cerebral structures if the normal patency of the blood vessels is not restored. Therefore, it will be impossible to do without treatment of osteochondrosis and its consequences.
So, osteochondrosis is a degenerative dystrophic change in the cartilage tissue of the intervertebral discs. Each of them consists of a dense fibrous ring and an internal gelatinous body - the nucleus pulposus. This structure can receive fluid and nutrition only during diffuse exchange with the surrounding soft tissues. If a person leads a sedentary lifestyle and spends a lot of time in a static position with tense muscles of the neck and collar area, then this process is disrupted.
At the same time, the stability of the position of the vertebral bodies is ensured precisely due to the normal height and degree of elasticity of the intervertebral discs. If protrusion (decrease in disc height) is observed, then adjacent vertebral bodies begin to shift relative to each other. It is worth knowing that the posterior vertebral arteries pass in a special canal formed by the hook-shaped (uncovertebral) processes of the vertebral bodies. Therefore, any, even slight, displacement of the vertebrae leads to a sharp decrease in the intensity of blood flow through the posterior vertebral arteries.
The carotid arteries and venous bed are pinched due to excessive static muscle strain. With protrusion or intervertebral hernia, reflex muscle tension occurs. In this way, the body compensates for the inability to provide full protection to the radicular nerves extending from the spinal cord. But a spasm of the cerebral blood vessels occurs.
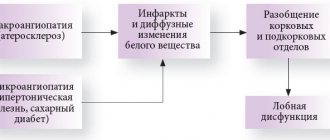
In severe cases, patients may develop a clinical picture of ischemic stroke followed by paralysis or paresis of certain parts of the body. With modern medical care, it is possible to transform this type of cerebrovascular accident into a transient one. If you consult a doctor in time, this attack will not have any health consequences.
If you develop cerebrovascular accident due to cervical osteochondrosis, we advise you to visit a neurologist or vertebrologist as soon as possible. If paralysis has already occurred, or a feeling of numbness has appeared in the body, then urgently call an ambulance. If you have pathology constantly and the severity of its manifestation is constantly increasing, then you need to make an appointment with a neurologist and undergo a full course of rehabilitation therapy.
In Moscow, you can make an appointment for a free appointment with a neurologist and vertebrologist at our manual therapy clinic. Experienced doctors work here. They will conduct a full examination, recommend additional examinations as necessary, make a diagnosis and tell you how to most effectively carry out treatment in your individual case.
Cervical osteochondrosis: symptoms and treatment
It’s rare that anyone today does not encounter manifestations of this widespread disease: according to statistics, about 60% of the population in developed countries suffer from manifestations of osteochondrosis to varying degrees.
The main reasons for such widespread prevalence are sedentary work and the lack of movement of modern people. Previously, cervical osteochondrosis in men usually manifested itself starting from 45-50 years, in women - a little later - 50-55 years. But now there is rapid rejuvenation: the typical picture is noticeable signs of the disease in 30-year-olds, and it is not uncommon for the first symptoms to appear at 20 years of age.
Osteochondrosis of the cervical spine: symptoms
In the early stages, the disease practically does not manifest itself with painful symptoms: you may feel discomfort in the neck after heavy physical activity or prolonged sitting in a tense position, after a sudden movement or tilting of the head.
The main symptoms are headache, dizziness and lack of coordination, a slight crunch when moving the head, general weakness; Less commonly observed are weakness of the arms, numbness of the tongue and speech impairment, problems with breathing, vision, hearing, increased sweating, and abnormally high blood pressure. The main areas are the back of the head, neck, collar area. In most cases, only a few of the listed signs of the disease are observed at the same time.
In general, the symptoms of osteochondrosis are not obvious; they are often masked by the use of painkillers. This is one of its dangers: most of the symptoms are also possible with other pathologies, which makes it difficult to diagnose cervical osteochondrosis.
The most important
Poor blood circulation in the brain with cervical osteochondrosis is a serious pathology that threatens with dangerous complications (stroke, ischemia, disability). To avoid dangerous consequences, you need to visit a neurologist when the first symptoms of pathology appear (headache, loss of coordination, tinnitus). The specialist will conduct a comprehensive diagnosis to distinguish between impaired cerebral blood flow associated with cervical osteochondrosis and other pathologies. With timely complex therapy, the patient will be able to get rid of unpleasant symptoms, slow down the development of pathology and prevent life-threatening complications.
Stages of development of osteochondrosis
In the development of cervical osteochondrosis, it is customary to distinguish 4 stages. But this is a rather arbitrary division, since most of the symptoms of the disease can also manifest themselves in other pathologies. In addition, the actual degree of tissue degradation of the cervical spine may not correspond to the externally manifested symptoms.
First stage (preclinical)
At the initial stage, symptoms are mild and are often attributed to stress or other diseases. You feel unpleasant stiffness in the neck, pain with sudden movements or bending. At this stage, it is quite possible to get rid of incipient osteochondrosis with the help of therapeutic exercises or simply move more and adjust your diet.
Second stage
The pain intensifies, becomes constant, and becomes severe with sharp turns or bends. Severe headaches appear, the patient begins to get tired quickly, becomes absent-minded, and areas of the face periodically become numb.
Third stage
The formation of disc herniation often causes dizziness, weakness of the arms, pain radiates to the back of the head and arms, and is constantly felt in the shoulders.
Fourth stage
Eventually, the intervertebral discs are destroyed and replaced by connective tissue. The nerves are pinched, which leads to difficulties in movement, acute pain, increased dizziness, and tinnitus.
Types of disease
Circulatory disturbances due to vascular compression can have varying degrees of severity. There are two main types of pathology - transient and acute cerebrovascular accident (PAI and ACVA).
PNMK
PNMC is a reversible condition characterized by cerebral ischemia. This condition is less dangerous than stroke, since all changes are reversible and not persistent. PNMK with cervical osteochondrosis develops gradually. Autonomic, vestibular or vascular changes may develop. The most common symptoms of PNMK in the vertebrobasilar region include:
| Group of clinical manifestations | Description |
| Vestibular ataxia | The main symptom is severe dizziness, which is accompanied by ataxia: · staggering; · instability when walking; · loss of balance. Often the symptoms are provoked by a sharp turn of the head, which leads to compression of the vertebral artery. |
| Vestibulocochlear syndrome | Dizziness in this case is accompanied by additional symptoms: · noise in ears; · hearing impairment. |
| Vegetative signs | Autonomic reactions often accompany PNMK in the vestibulo-basilar region: · shortness of breath, attacks of suffocation; · palpitations, fluctuations in blood pressure, pain in the heart; · hot flashes; · increased sweating; frequent urination; · nausea, vomiting; · diarrhea; · swallowing disorder. |
| Hemianopsia | Hemianopsia is the loss of halves of vision on both sides. That is, a person sees only half the picture with his left and right eyes. |
| Drop attacks | Drop attacks occur when the head is thrown back suddenly. The following manifestations develop: · severe muscle weakness; Loss of function of arms and legs; · a fall. The person does not lose consciousness. |
ONMK
ACVA (stroke) is an irreversible disruption of the blood supply to the brain. ACVA in osteochondrosis develops much less frequently than PNMK. This is usually facilitated by the presence of concomitant diseases - atherosclerosis, vascular abnormalities, arterial hypertension.
To suspect a person is having a stroke, you need to ask them to do three things:
- Smile. With a stroke, the smile is often asymmetrical - one corner of the mouth is downward.
- Speak. With a stroke, pronunciation is often impaired; a person will not be able to pronounce even a simple sentence.
- Raise your hands. When a person has a stroke, they often raise their arms to different heights.
If even 1 symptom out of 3 is detected, there is a high probability of a stroke, you should immediately call an ambulance.
What should the patient do?
If symptoms of stroke appear, you should immediately call an ambulance. While the ambulance is traveling, it is recommended to begin providing first aid:
- lay the victim on his back or side;
- unbutton tight clothes;
- provide access to fresh air;
- do not allow the patient to eat or drink;
- do not take medications without direct indications.
In the case of PNMK, medical assistance is also indicated, but you can consult a doctor as planned.
Causes and risk factors
Oddly enough, the possibility of developing osteochondrosis in humans is due to one of its evolutionary advantages - upright posture: the vertebrae press on each other, and with age, the connective tissue degrades. As a result, in older people this is an almost inevitable process. But there are many factors that contribute to the earlier and more intense development of cervical osteochondrosis:
- First of all, this is a sedentary and sedentary lifestyle, often observed in modern life (office workers, drivers and other “sedentary” professions, TV, long hours at the computer), lack of physical activity
- Tense, unnatural postures while working: for example, at a computer, a person often leans forward, taking a tense posture
- The opposite reason is that the load is too high and unusual for a given person; but even trained athletes, for example, weightlifters, are at risk;
- Any reasons that disrupt a person’s natural posture: uncomfortable shoes, especially high heels, poor sleeping position, flat feet, rheumatism, scoliosis;
- Excess weight, which is often caused by poor diet
- Frequent stress, severe nervous tension, constant overwork
- Local hypothermia
Osteochondrosis: how the disease affects the brain
Osteochondrosis can easily be called a disease of modern civilization. This disease is caused by stress on the spine, as well as intervertebral discs. Unfortunately, in the modern world, our sedentary lifestyle only contributes to the development of the disease. Perhaps every adult, in one way or another, experiences manifestations of this disease in a variety of forms. This is a disease in which the pathological process involves articular cartilage and bone tissue. The consequences of the process inevitably leave a mark on the work of the whole body, incl. in the functioning of the brain.
Factors provoking the disease
The primary cause of this disease is aging. It is most often observed in people over 30 years of age. Heavy loads also contribute to the destruction of bone tissue and slow down the regeneration of intervertebral joints. The specific causes of the disease have not yet been clearly established. However, there is a general set of factors that provoke this disease:
- Metabolic disorders in the body, and, as a result, excess weight, which, in turn, puts enormous stress on the intervertebral discs.
- Hereditary factors.
- poor posture. flat feet.
- spinal injuries due to fractures, bruises, injuries of various nature, as well as excessive loads.
- Poor nutrition. Lack of vitamins and microelements. Sedentary lifestyle.
- Uncomfortable posture during sleep.
- Uncomfortable shoes. Also the heels are too high.
- Using the same shoulder to carry a bag.
Cervical osteochondrosis often occurs during pregnancy or in women during menopause. The reason for this is hormonal levels. It transforms the connective tissue, causing it to become thinner.
Osteochondrosis of the cervical spine, symptoms
Osteochondrosis of the cervical spine manifests itself differently, in contrast to diseases of other parts of the spine. This is due to the fact that the cervical vertebrae are located closer to each other. They also have differences in structure. Our neck is characterized by extraordinary mobility and is located as close as possible to the head, supporting it. Therefore, often in the cervical spine, due to pinching in this section, the nerve nodes are blocked, and the artery that provides blood circulation to the brain is pinched. His nutrition is also disrupted due to lack of oxygen due to significantly impaired blood circulation. And the consequences of such a violation can be the most dire. Symptoms of cervical osteochondrosis may include:
- Pain when moving the head. Crunch in the neck.
- Loss of strength in the hands. “Cotton hands” effect.
- Decreased hearing and vision.
- Decreased tactile sensitivity in the palms.
Sure signs of osteochondrosis are:
- Pain in the shoulders, neck, and also shoulder blades.
- Frequent, seemingly causeless headaches. Pain in the temples and back of the head.
- Shifting pain that radiates to the shoulder or chest.
Several degrees of development of osteochondrosis
Osteochondrosis, regardless of its location on the spinal trunk, does not develop immediately, but in stages. There are several stages in this process:
- The fibrous tissue between the vertebrae is damaged, which is caused by a reduction in the height of the disc. This occurs due to dehydration of the nucleus pulposus. Simply put, micro-tears appear in the osteochondral tissue. Unfortunately, the symptoms in this case are hardly noticeable. And pain and fatigue are usually attributed to stress.
- Ligaments and muscles sag, which, in turn, inevitably leads to pathological mobility of the vertebrae and instability of their motor function. Displacement of the vertebrae appears.
- Stage of formation of prolapses and protrusions of joints. Arthrosis also begins to actively develop in the intervertebral discs. At this stage, hernias begin to form, and the cervical vessels and muscles are significantly damaged. Dizziness and pain in the back of the head are becoming more and more common.
- This stage is characterized by the proliferation of bone tissue. The same one that was once designed to protect the vertebrae from excessive stress. As a result, the mobility of the vertebrae is blocked. As a result, the nerve endings are pinched. The spine is no longer able to perform its previous functions, as its mobility is significantly impaired.
Treatment and prevention of osteochondrosis and its consequences
To identify all such pathologies of the musculoskeletal system, a complete diagnosis is necessary. Appropriate complex therapy can only be recommended on the basis of a medical examination and examination results. Regardless of the chosen method, throughout the entire period of treatment it is necessary to maintain a correct and balanced diet in order to provide maximum nutrition to the brain, which has already felt the influence of osteochondrosis in one way or another. Treatment includes medication, physical therapy, and massage. In the case of treating protrusion of the cervical spine, manual therapy, along with traditional methods, is considered especially effective.
Regularity and phasing are the most important conditions for treating the disease. Only in this way can you count on results. Gymnastics and yoga are good for sedentary people. Breathing practices are useful for balancing blood circulation, incl. and in the brain.
In addition to basic therapy, it is also necessary to change the lifestyle that once contributed to the development of the disease.
To reduce the load on your back, you need to wear comfortable shoes, leaving heels for special occasions, do not slouch, and swim. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Why is cervical osteochondrosis dangerous?
Many vital vessels, arteries, and capillaries are concentrated in the neck area, so any disturbance there can have unpleasant consequences, including oxygen starvation, hypertension, and vegetative-vascular dystonia.
Cervical osteochondrosis affects the segments of the spine that control the functioning of the shoulder and elbow joints, the thyroid gland, hands and other organs. With osteochondrosis, if left untreated, there is a high probability of pinched nerves and compression of blood vessels, which inevitably affects the functioning of other organs.
Which doctor should I contact?
Symptoms of cervical osteochondrosis are usually mild, especially at the initial stage, in addition, almost all of them are characteristic of other pathologies: in such conditions, it is best to consult a therapist who will analyze your complaints, conduct an examination and refer you for diagnosis and to a more highly specialized specialist - neurologist, orthopedist.
Who will carry out further treatment depends on the stage of the disease and the disorders detected during diagnosis. For example, the formation of a hernia or displacement of discs may require the help of a traumatologist. Massage and exercise therapy, physiotherapy are non-surgical methods of treatment; in severe cases, the patient is referred to a surgeon.
We diagnose the disease based on the main signs
During the initial diagnosis, seek the help of relatives or friends by discussing specific symptoms. Find on the Internet similar variants of the course of the disease as yours.
If you understand that osteochondrosis is not easy, but that there may be serious problems with blood circulation, then immediately seek medical help.
- Once again we remind you of the main symptoms of pathology in the bloodstream with osteochondrosis.
- Frequent attacks of dizziness.
- Severe and prolonged migraine attacks.
- Numbness of the arms and legs for short and long periods of time.
- Decreased visual acuity, pain in the eyes.
- Cramps.
- Nausea, vomiting.
- Fatigue and irritability.
Similar symptoms occur in different diseases, so only a doctor can make an accurate diagnosis. Do not self-medicate, it causes adverse reactions.
What types of examinations need to be completed?
Once again we emphasize the similar symptoms of the diseases. Osteochondrosis is easily diagnosed. And circulatory disorders during this pathology are not easy to determine, especially at the initial stage. It is important to identify this problem as early as possible. Therefore, do not be surprised if the doctor refers you to different types of diagnostics. The following options may include.
All diagnostics begin with an MRI and CT scan. During the examination, affected areas in the blood vessels are identified. The overall picture becomes clear - where and how serious the brain damage is.
An x-ray of the cervical spine is taken to determine the level of bone growth and closure of the main artery.
Dopplerography - diagnostics shows where the obstacle to the movement of blood flow is.
Antiography - diagnostics of blood vessels. Where are the problem areas in the vascular system and pressure on the vessels occurs.
The treatment package is prescribed by the doctor based on the diagnosis after analyzing all the diagnostic measures taken.
Diagnostics
Since the symptoms of osteochondrosis are mild and often overlap with other pathologies, it is better to conduct an initial examination with a therapist or other specialist - a neurologist, orthopedist. He will ask you about pain and other symptoms, check neck mobility, skin condition, balance, and reflexes.
If a primary diagnosis of “cervical osteochondrosis” is made, the doctor will then refer you for additional studies. The most effective of them is MRI, followed by computed tomography. X-ray studies are much less effective than the first two, especially with advanced disease. The condition of soft tissues is checked using ultrasound. If your doctor suspects blood vessel damage, you may be referred for a vascular duplex scan.
Since some symptoms overlap with signs of angina and coronary heart disease, you may need to consult a cardiologist who will refer you for an ECG and echocardiography.
How to treat cervical osteochondrosis
Real, sustainable success in the treatment of cervical osteochondrosis can be achieved only with an integrated approach, which includes medications, massage of the collar area, therapeutic exercises, and physiotherapy.
In particularly advanced cases, surgical intervention may be required. Naturally, the patient must eliminate or minimize factors contributing to the development of the disease: move more, eat better, etc. We strongly advise against resorting to self-medication, primarily because the symptoms of osteochondrosis can mean a completely different disease: not only will the drugs you choose not help in treatment, they can also cause harm. Even during painful exacerbations, do not rush to the pharmacy for painkillers - it is better to make an appointment with a doctor, and even better - do it in advance, at the first symptoms.
Relieving acute pain
Osteochondrosis, especially in the later stages, is accompanied by severe pain, so the first task of the attending physician is to alleviate your suffering. He will prescribe you painkillers, anti-inflammatory drugs, vitamins, chondroprotectors to restore cartilage tissue, medications to improve blood circulation and reduce muscle spasms.
In this article, we deliberately do not give the names of specific drugs - it is better to leave their choice to doctors who will take into account all possible consequences and evaluate contraindications.
Therapeutic exercises for cervical osteochondrosis
The simplest and most accessible method, including at home, is therapeutic exercises. At the same time, it is also quite effective, as it strengthens the neck muscles, restores blood circulation in damaged areas, and compensates for the lack of movement in everyday life. Physical therapy can be supplemented with swimming and aqua gymnastics.
There are many methods, including the use of simulators: most of them do not require special equipment or any special conditions, but we advise you to contact the exercise therapy office, where they will select the most effective sets of exercises for you and conduct classes under the guidance of an experienced specialist.
Physiotherapy
Correct and constant use of physiotherapeutic methods improves blood circulation in damaged areas, reduces inflammation and pain, and slows down the ossification process.
For osteochondrosis of the cervical spine, electrophoresis, magnetic therapy, laser therapy, shock wave therapy, therapeutic baths and showers, mud therapy and other methods are used.
Neck massage for osteochondrosis of the cervical spine
For osteochondrosis, massage can be very effective: it improves blood circulation, reduces the likelihood of spasms by reducing muscle tone, relieves pain symptoms and improves the general well-being of the patient.
But massage and manual therapy must be used extremely carefully, since inept and rough influence on diseased areas of the body can only cause harm. We strongly advise you to consult your doctor first.
Surgery
In particularly advanced cases, even surgical intervention cannot be ruled out: narrowing of the lumen of the spinal column, the formation of herniated intervertebral discs, or spondylolisthesis.
The decision on the need and method of surgical intervention is made by the surgeon, who also determines the preparatory operations, the duration of the postoperative period and rehabilitation.
Treatment of cerebral circulatory disorders in cervical osteochondrosis
It is possible to begin treating cerebral circulation disorders in cervical osteochondrosis only after the normal configuration of the spinal column has been restored. It is very important to restore the physiological height of the intervertebral spaces and the position of the vertebral bodies. This immediately relieves muscle fiber tension syndrome. Pressure is relieved from arteries and veins and blood flow is restored without the use of pharmacological drugs.
This effect can be achieved using the procedure of manual traction of the spinal column. During the procedure, the doctor releases all compressed soft tissue. The muscle fiber relaxes. To completely relieve pain in the neck area, 3–4 procedures are sufficient.
The treatment of impaired venous outflow in cervical osteochondrosis begins in a similar way - first, muscle fiber tension syndrome is relieved, then the normal position of the vertebral bodies is restored. After normalization of the patient’s condition, it is important to carry out a full course of restoration of the condition of the intervertebral cartilaginous discs. For this, it is very important to restore diffuse tissue nutrition. This can be achieved using the following influence methods:
- osteopathy is necessary so that the doctor has the opportunity to restore the disrupted process of microcirculation of fluids (blood, lymph) in the lesion and thereby accelerate the regeneration process by enhancing trophism at the cellular level;
- massage allows you to safely and effectively restore the normal tone of the muscle fiber, improves its functionality and ability to provide diffuse nutrition to the intervertebral cartilaginous discs;
- physiotherapy procedures trigger disrupted metabolic processes and help free tissues from cell decay products accumulated in them;
- laser exposure accelerates the restoration of the cartilaginous fibrous ring of the intervertebral disc;
- reflexology starts the process of tissue regeneration by using the hidden reserves of the human body;
- Therapeutic gymnastics and kinesiotherapy are needed in order to eliminate muscle blocks and ensure an even distribution of physical activity when performing a special set of exercises - thus increasing the intensity of diffuse nutrition of cartilage tissue.
The course of treatment is always developed individually for each patient. You can sign up for a free consultation with a vertebrologist or neurologist at our manual therapy clinic. After the examination, an experienced doctor will tell you about all the prospects and possibilities of treatment using our methods.
Possible complications and consequences
In the neck area there are many nerve endings and blood vessels that directly affect the functioning of other parts of the body: if cervical osteochondrosis is not treated, it can lead to an increase in many other diseases:
- Migraine – it is in the neck area that the vertebral artery delivers blood to the brain: narrowing also leads to severe headaches.
- Visual impairment - the carotid and vertebral arteries, which are responsible for supplying blood to the visual organs, pass through the neck: compression of the nerve roots and blood vessels leads to decreased vision.
Establishing a diagnosis
When the first suspicious symptoms appear, for example, frequent headaches, vertigo, hearing and vision disorders, you should contact a neurologist, reflexologist or vertebrologist.
Currently, the following instrumental methods are used to identify cerebral circulation disorders against the background of cervical osteochondrosis:
- Doppler ultrasound (Doppler ultrasound) of the neck vessels is used to assess the degree of vasoconstriction, as well as measure the speed of blood flow.
- Transcranial Doppler ultrasound is an ultrasound examination of the blood supply to the brain, which allows one to assess blood flow through intracranial vessels. This technique allows you to identify a violation of venous outflow, as well as arterial outflow, to identify spasm or local dilatation of blood vessels (aneurysm).
- X-rays of the spine are used to identify bone growths, as well as areas where the height of the vertebrae is reduced.
- Using magnetic resonance imaging, the doctor can assess the condition of the cartilage linings of the vertebrae, detect protrusions, hernias, and determine their size. In addition, this study is informative regarding blood vessels.
After confirming the diagnosis, the doctor draws up a treatment plan.
Prevention of cervical osteochondrosis
Osteochondrosis of the cervical spine is a disease whose negative impact can be minimized with proper and timely prevention. You need to think about its prevention in childhood: poor posture and flat feet in a child are a reason to consult a doctor for a diagnosis.
The basis for the prevention of osteochondrosis is a correct lifestyle: reasonable physical activity and periodic exercise during sedentary work, a healthy diet, body weight control.
Preventive measures
To prevent cerebrovascular accidents, a person must follow recommendations that will help him avoid diseases of the cervical spine and surrounding vessels:
- Eat right, watch your weight.
- Maintain a moderately active lifestyle, walk more often.
- When working sedentarily, get up every 2 hours and stretch your neck.
- Give up bad habits.
- Sign up for preventive massage courses.
- Get regular medical examinations to spot dangerous problems in time.
By adhering to these recommendations, a person will be able to maintain the health of the spine (including the cervical spine) for a long time.