Vascular diseases of the brain
The brain (cerebrum)
is an organ of the central nervous system, consisting of many interconnected nerve cells and their processes.
Vascular diseases of the brain are recognized in medicine as one of the most dangerous groups of diseases, as they have quite serious consequences for the body. Each cerebral vascular disease has characteristic features that depend on which specific vessels are affected by the pathological process. But in any case, doctors at OKB No. 1 warn that diseases in this group can provoke a hemorrhagic or ischemic stroke, after which the patient either becomes disabled or dies.
Clinical manifestations of vascular diseases of the brain can be divided into the following forms:
- chronic cerebral ischemia stage I-II;
- cerebral circulatory disorder of a transient nature;
- cerebral infarction (ischemic stroke);
- bleeding in the brain (hemorrhagic stroke).
Causes of cerebrovascular diseases:
The occurrence of cerebrovascular diseases occurs as follows: insufficient blood supply limits the access of oxygen and glucose, resulting in a cerebral infarction, the results of which are unpredictable. In adulthood, vascular atherosclerosis and hypertension can negatively affect blood supply.
Treatment of vascular diseases of the brain:
Among the many diseases of the cerebral vessels, coronary disease and discirculatory encephalopathy deserve special attention.
Treatment of ischemic disease involves:
- work on restoring impaired physiological and behavioral functions, for which restorative therapy, magnetic and electrophoresis, physical therapy, and massage are used;
- stabilization of blood pressure and prevention of strokes with the help of anticoagulant and vasodilator drugs;
- normalization of metabolism and proper blood circulation. The best results are ensured by taking medications according to medical prescriptions.
Vegetative vascular dystonia
Vegetative-vascular dystonia is a disturbance in the functioning of the body’s vascular system, leading to insufficient oxygen supply to tissues and organs. Otherwise, this disease is called neurocirculatory dystonia, or cardiac neurosis.
Causes of VSD:
- Exhaustion of the body due to acute or chronic infectious diseases or intoxications.
- Sleep disturbances such as insomnia, early awakening or difficulty falling asleep.
- Chronic fatigue, depressed mood, depression.
- Irregular unbalanced diet.
- Excessive physical activity or physical inactivity.
- Hormonal changes in the body during puberty in adolescents, pregnancy or menopause in women.
- Change of climate or time zone.
Types of vegetative vascular dystonia:
With a more accurate diagnosis, three types of vegetative-vascular dystonia are distinguished:
- if, with general signs of fatigue, you sometimes have a feeling of lack of air, you complain of irregular heartbeats, then this is vegetative-vascular dystonia of the cardiac type;
- The hypotensive form of vegetative vascular dystonia is characterized by low blood pressure, general weakness, headaches, coldness of the fingers and toes, and a tendency to faint;
- periodic surges in blood pressure indicate hypertensive vegetative-vascular dystonia.
Diagnosis of VSD:
The diagnosis of vegetative-vascular dystonia is made only after a comprehensive examination of the patient and the exclusion of other pathologies that have similar manifestations to VSD.
The list of diagnostic measures includes:
- Laboratory research of general blood test, biochemical composition of plasma, coagulation indicators, hormone levels. If necessary, urine tests are performed. Most often, the indicators of these studies do not go beyond normal values.
- Functional techniques, including ultrasound examination of internal organs and blood vessels of the head and neck, ECG, monitoring of blood pressure levels.
- X-ray of the spinal column, tomography of the brain and spinal cord.
- Consultations with specialists in related specialties.
Only after confirming the absence of other diseases can a diagnosis of vegetative-vascular dystonia be made.
Treatment of vegetative-vascular dystonia:
The majority of patients with VSD do not require drug therapy. The basis of treatment for them is methods aimed at changing the patient’s lifestyle and normalizing the functioning of the nervous system. Physiotherapeutic methods are mainly used to treat the disease. This could be hydromassage, physical therapy. If the symptoms of vegetative-vascular dystonia are serious, acupuncture, manual therapy, and herbal medicine give good results. Vegetative-vascular dystonia responds well to treatment. The main thing is not to self-medicate. The choice of methods by which to treat vegetative vascular dystonia should be determined only by a doctor after conducting the necessary research. Often, VSD “masks” another disease, so its treatment should be aimed primarily at eliminating the underlying disease. And, of course, first of all, don’t bring yourself to the point of needing to see a doctor: try to avoid stressful situations and emotional breakdowns, and, if possible, take a few days of rest and spend them as you would like for a long time. Thus, treatment of vegetative vascular dystonia should be based on both drug therapy and regulation of the mental state.
Causes of pathology
Vascular diseases of the brain can occur for a number of reasons. As a rule, several reasons lead to the appearance of pathology. The most common ones include:
● genetic predisposition;
● narrowing and hardening of intracerebral arteries (with hypertension);
● multiple focal and/or diffuse brain lesions;
● long-term somatic diseases of the expectant mother (and during pregnancy);
● atherosclerosis of cerebral vessels;
● rheumatic lesions;
● disturbances in the functioning of the respiratory system (for example, pulmonary edema);
● abuse of alcohol and tobacco products during pregnancy;
● disturbances in metabolic processes;
● increased blood viscosity;
● fractures of the skull bones;
● heart rhythm disturbance (with atrial fibrillation, blood hemodynamics are disrupted);
● serious abnormalities in the nervous system (increased anxiety, chronic stress);
● serious abnormalities of the endocrine system (diabetes mellitus, obesity);
● development of intrauterine infections;
● difficult long labor (with injuries);
● hypertension;
● hypercholesterolemia;
● various anomalies of the cardiovascular system (for example, hypoplasia of cerebral vessels, mitral valve prolapse).
Vascular diseases of the spinal cord
The spinal cord (Medulla spinalis)
is an organ of the central nervous system, consisting of nerve cells and fibers and located in the spinal canal. It starts from the brain and ends in the vertebrae of the lumbar spine and is a long cord, shaped like a cylinder.
It consists of gray matter, which is surrounded on all sides by white matter. The gray matter is predominantly nerve cells, and the white matter is the processes of nerve cells. Spinal cord damage can be caused by various factors. Diseases of the brain and spinal cord, as well as other lesions of its various parts can cause sensory, motor and autonomic disorders. The length of the adult spinal cord ranges from 41 to 45 cm. The spinal cord regulates the functions of the entire body by transmitting nerve impulses to all internal organs.
The human spinal cord can be divided into 5 sections:
-cervical, thoracic, lumbar, sacral, coccygeal. Syndromes of spinal cord lesions differ at different levels, and also depending on which substance is affected, gray or white.
Myelitis
Myelitis
is an inflammation of the spinal cord. The sooner we stop the inflammation, the less the loss of spinal cord substance, the faster the recovery.
Causes and symptoms of myelitis:
Inflammation and destruction of spinal cord tissue leads to a disconnection of communication between the brain and the body, and therefore to:
- sensitivity disorders;
- paresis (paralysis).
Myelitis usually responds well to treatment, you just need to clarify the cause of its occurrence. Therefore, we suggest you conduct research on the following:
- neuroinfections;
- multiple sclerosis;
- disseminated encephalomyelitis.
Diagnosis of myelitis:
- On MRI scans of the spinal cord, foci of inflammation and demyelination are clearly visible.
- Blood tests for antibodies to various infections and rheumatic indicators make it possible to differentiate between neuroinfection and autoimmune inflammation.
- Blood biochemistry data will help identify possible metabolic disorders, which will allow you to select medications correctly.
- A detailed immunogram will allow you to clearly assess the cause of what is happening and select the appropriate treatment for this situation.
- ENMG (electromyography, electroneuromyography, myography) is a set of studies to assess muscle function and the quality of transmission of nerve impulses along peripheral nerves and pathways of the brain and spinal cord. ENMG helps us pinpoint the location of the injury (brain, spinal cord, peripheral nerve or muscle)
Information for patients and their relatives
Rules for hospitalization
Services and prices of the department
About the symptoms of vascular diseases of the central nervous system
Patients experience a variety of symptoms. This is explained by the fact that certain areas of the brain are affected to a greater extent. But it’s still worth mentioning the main symptoms. So, tremors of the limbs and back pain, paresis and paralysis are the main factors indicating problems with the blood vessels of the brain. In addition, disturbances associated with the inability to sleep appear. There is a disorder of consciousness. But you can’t diagnose yourself. Only an experienced doctor, based on the results of a comprehensive examination, is able to accurately diagnose the disease. And based on the data obtained, it becomes possible to select the necessary methods and technologies. Don't worry, because there won't be any pain. This is facilitated by the professional approach of specialists and modern medical capabilities. Therefore, it is important to cast aside doubts by taking care of your health.
Having received data from the anamnesis and other studies, specialists from the neurosurgical department of the City Clinical Hospital named after. A.K. Yeramishantsev will be able to choose the most optimal and rational treatment methods. Particular attention is paid to the diagnosis and level of neglect of the disease. The characteristics of the body play an important role. The combination of these factors allows us to judge how successful the entire treatment will be. Intracranial and intravascular surgical interventions are performed by specialists with extensive practical experience. We have modern tools and high-quality equipment. All this helps to accurately diagnose and treat patients so that there are positive results.
The team of doctors also provides services that involve disease prevention. Everything is considered on an individual basis. Therefore, it is worth saying that in any situation it is better to contact the State Clinical Hospital named after. A.K. Yeramishantsev than to hope for a miracle. Only a professional approach and attentive attitude of doctors will give you a good chance of recovery. Also, the set of recovery measures is effective.
Clinical classification of vascular lesions of the brain
Classification of vascular lesions of the brain (E.V. Schmidt, 1985) I. Diseases and pathological conditions leading to circulatory disorders in the brain 1. Atherosclerosis 2. Hypertension (essential hypertension) 3. Diseases with symptomatic arterial hypertension 4. Combination of atherosclerosis with arterial hypertension 5. Vasomotor dystonia 5.0. Neurocirculatory dystonia 5.1 Vegetative-vascular dystonia 6. Arterial hypotension 7. Damages of the heart and disorders of its activity 8. Anomalies of the cardiovascular system 9. Damage to the lungs leading to pulmonary heart failure with impaired venous circulation in the brain 10. Infectious and allergic vasculitis 11. Toxic lesions of the brain vessels 12. Diseases of the endocrine system 13. Traumatic lesions of the brain vessels and its membranes 14. Compression of arteries and veins (with changes in the spine, tumors and DR-) 15. Blood diseases II. Disorders of cerebral circulation A. Initial manifestations of insufficiency of blood supply to the brain 1. Initial manifestations of insufficiency of blood supply to the brain B. Transient disturbances of cerebral circulation 1. Transient ischemic attacks 2. Hypertensive cerebral crises 2.0. General cerebral 2.1. With focal disorders B. Stroke 1. Subarachnoid non-traumatic hemorrhage 1.0. Non-traumatic hemorrhage under the membranes of the brain 2. Hemorrhagic stroke—non-traumatic hemorrhage 2.0. Cerebral hemorrhage 3. Other and unspecified intracranial hemorrhage 3.0. Non-traumatic extradural hemorrhage 3.1 Non-traumatic acute subdural hemorrhage 3.2 Unspecified intracranial hemorrhage 4. Ischemic stroke (infarction) 4.0. Cerebral ischemic stroke 4.0.0. In case of damage to the precerebral main arteries 4.0.1. In case of damage to the cerebral arteries 4.0.2. With cerebral artery embolism 5. Stroke with a recoverable neurological deficit - minor stroke 6. Insufficiently specified acute cerebrovascular accidents 7. Consequences of a previous stroke (more than 1 year) D. Progressive cerebral circulatory disorders 1. Chronic subdural hematoma 2. Dyscirculatory encephalopathy 2.0. Atherosclerotic 2.1. Hypertensive 2.2. Venous and other or unspecified vascular lesions D, Other and unspecified vascular lesions 1. Cerebral III. Localization of the lesion 1. Brain hemispheres 1.0. Cortex and immediate subcortex 1.1. White matter (indicating the affected lobe or lobes) 1.2. Inner capsule 1.3. Subcortical nodes 2. Brainstem 2.0. Midbrain (tegmentum, base) 2.1. Bridge (tire, base) 2.2. Medulla oblongata 2.3. Multiple foci 3. Cerebellum 4. Localization not established IV. Nature and localization of vascular changes A. Nature of vascular damage 1. Blockage of the lumen of the vessel 2. Narrowing of the lumen of the vessel (in%) 3. Kinks, looping of vessels 4. Aneurysms: a) saccular; b) arteriovenous; c) carotid-cavernous, arteriovenous anastomosis 5. Other lesions of the arteries 6. Other lesions of the veins and venous sinuses B. Localization of the lesion 1. Common lesion 2. Aorta 3. Innominate artery (brachiocephalic trunk) 4. Carotid artery (common, internal, external ) 5. Subclavian artery 6. Vertebral artery 7. Main artery 8.9.10. Anterior, middle, posterior cerebral arteries 11. Branches of the basilar artery 12. Inferior posterior cerebellar artery 13. Branches of the external carotid artery (meningeal artery) 14. Cerebral veins and sinuses 15. Jugular vein 17. Other vessels 18. Localization not established V. Characteristics of clinical syndromes Subjective symptoms (without objective neurological symptoms) 1. Organic microsymptoms without symptoms of loss of functions (anisoreflexia, slight deviation of the tongue, etc.) 2. Motor disorders (paresis - paralysis, extrapyramidal disorders, coordination disorders) 3. Sensitivity disorders (pain, decreased sensitivity) 4. Impaired function of the sensory organs 5. Focal disturbances of higher cortical functions (aphasia, agraphia, alexia, etc.) 6. Epileptiform seizures (general, focal) 7. Changes in intelligence, memory, emotional-volitional sphere 8 Psychopathological symptoms 10. Other VI. State of ability to work 1. Able to work 2. Temporarily disabled 3. Limited able to work 4. Incapacitated 5. Needs outside help 6. Needs observation, supervision
For more than 20 years, the classification proposed by A.V. Pokrovsky has been successfully used among angiosurgeons. It allows you to navigate quite accurately when determining the validity and timeliness of surgical measures for extracranial lesions of the cerebral arteries. Classification of chronic arterial insufficiency of the brain by A. V. Pokrovsky 1) etiology, 2) localization [all affected vessels and the degree of impairment of their patency (stenosis, occlusion) should be indicated in detail] 3) degree of cerebral circulatory impairment. According to the degree of cerebrovascular accident, we distinguish 4 groups: 1) asymptomatic, 2) transient disorders, 3) chronic vascular insufficiency, 4) stroke or its consequences.
Stage I cerebrovascular accident is characterized by the absence of symptoms of cerebral ischemia in the presence of proven damage to the brachycephalic arteries.
In grade II - transient disorders - transient ischemic attacks of varying severity and duration of no more than 24 hours are observed.
At stage III, general symptoms of slowly progressing vascular disease of the brain without ischemic attacks and strokes are revealed.
The fourth degree is progressively increasing dyscirculatory encephalopathy and severe consequences of stroke.
The clinical classification of chronic arterial insufficiency of the brain, proposed by B. A. Konstantinov and Yu. V. Belov (1996), reflects the functional state of the brain in this pathology. Classification of chronic arterial insufficiency of the brain by B. A. Konstantinov and Yu. V. Belov When assessing the state of cerebral circulation, division into 4 functional classes is used. 1 FC There is stenosis of the artery supplying the brain, but there are no symptoms of cerebral ischemia (so-called asymptomatic stenosis). 2 FC Characterized by transient ischemic attacks of varying severity, lasting no more than 24 hours. 3 FC Chronic cerebrovascular insufficiency, manifested by symptoms of slowly progressive vascular disease of the brain without or with transient ischemic attacks. In contrast to FC 2, there are permanent, and permanent, differently expressed and prone to change, symptoms of damage to certain parts of the brain. 4 FC A distinctive feature of this class is a progressive stroke or its consequences. All three of the above classifications do not contradict each other; by interacting, they allow choosing the most optimal diagnostic and treatment tactics.
In our opinion, the clinical classification of B. A. Konstantinov and Yu. V. Belov is preferable for screening examinations, the classification of A. V. Pokrovsky is preferable when determining treatment tactics, since additional examination methods are used in the assessment. Classification by E.V. Schmidt allows for a comprehensive assessment of all components of cerebrovascular insufficiency. The integrated approach of neurologists, therapists and angiosurgeons in a common understanding of classification characteristics allows tactical coordination to be carried out more productively and at an early stage, determining the optimal treatment and diagnostic algorithm.
Mental disorders in vascular diseases of the brain are a group of pathological conditions that develop as a result of cerebral circulatory disorders of various etiologies and pathogenesis.
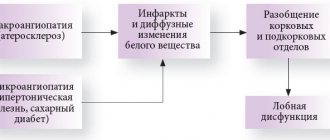
Atherosclerosis, hypertension, intracranial aneurysms, vasculitis and amyloidosis of cerebral vessels can cause both acute (strokes, transient disorders, crises) and chronic cerebral circulatory disorders, which is reflected in mental disorders of varying depth and nature. Vascular damage to the brain and mental disorders resulting from it can develop at any age, but they become significantly more frequent in the second half of life, reaching the peak of their prevalence in old age. Mental disorders of cerebrovascular origin account for 28.1% of all cases of mental pathology in people over 60 years of age attending a general clinic, and about 40% among people over 74 years of age [Mikhailova N. M., 1996].
In recent years, the ability to diagnose cerebrovascular diseases has improved dramatically. This happened due to the introduction into clinical practice of intravital imaging (CT, MRI, single-photon emission tomography, positron emission tomography, etc.) of brain structures, which makes it possible to observe and quantify structural, hemodynamic and metabolic changes in the brain. All this led, on the one hand, to the development of more stringent and clear criteria for diagnosing the vascular brain process, and on the other, to a significant revision of the approaches, principles of typology and classification of mental disorders in vascular pathology of the brain, especially persistent cognitive disorders (dementia).
Modern assessment and approaches to differentiation of mental disorders observed in vascular diseases of the brain are largely determined by new approaches to the classification of mental diseases (ICD-10) with their predominantly syndromic principle, as well as the use of quantitative assessment of psychopathological conditions. Because of this, various psychopathological phenomena (delusional, depressive, mnestic-intellectual), arising from the same vascular disease of the brain, often find themselves in different diagnostic categories. The most specific position in ICD-10 is occupied by vascular dementia. It is classified under the section “Organic, including symptomatic, mental disorders” (F.O), making up the general heading F01 (from F01.0 to F01.9).
The cause-and-effect relationships between vascular diseases of the brain and the mental disorders observed with them are very complex. Firstly, in the presence of undoubted signs of vascular damage to the brain, mental disorders do not always occur. Secondly, even in those cases where these disorders develop, their connection with vascular pathology can have quite different degrees of obviousness - from indisputable to very doubtful. This is largely due to both the nature of the vascular lesion of the brain (its severity, severity, localization), and the possibility of the simultaneous presence in patients (especially elderly and senile patients) of another somatoneurological pathology (multimorbidity) and, above all, such as arterial hypertension, coronary artery disease heart disease, diabetes mellitus, which are “vascular risk factors,” as well as degenerative brain diseases (Alzheimer’s disease, Parkinson’s disease, etc.). In addition, the constitutional and genetic characteristics of the patient are also important.
With vascular disease of the brain, as with any other organic pathology, one can observe, on the one hand, mental disorders of the exogenous-organic series (the concept of “exogenous” in this case relates not so much to the genesis, but to the characteristics of the symptoms of the disease; namely in in this sense, we use it in the text of this chapter), which are more directly related to it - “basic” (according to Yu. E. Rakhalsky, 1964) or “obligate” vascular mental disorders (according to J. Quind, 1975), and on the other - so-called endoform (endogenomophic) mental disorders - “conditional” (according to E. Ya. Sternberg, 1969), “accidental” (according to F. Stern, 1930), the connection of which with cerebrovascular pathology is more indirect and problematic.