Coronavirus without symptoms
Asymptomatic patients are considered patients whose smears show SARS-CoV-2, but there are no other signs of the disease.
- Even in the first wave in the UK, according to statistics, 78% of virus carriers had no symptoms or a mild form of infection.
- According to statistics from doctors in Italy, 50-70% of people with coronavirus infection are without symptoms. Research was also conducted in the spring of 2020.
- According to Australian scientists, the disease occurs without symptoms in more than 80% of cases.
- In Russia, at the beginning of the epidemic, it was believed that asymptomatic patients could make up up to a quarter of those infected, in July 2020 they began to talk about 40-50%, and at the beginning of the second wave, doctors say: 25% of those infected have symptoms of the virus, that is, they are asymptomatic 75% of people. Thus, the new Russian data are already close to the results that were obtained in the UK in the first wave.
The difference in data arises because different countries (and at different times) test different numbers of people for coronavirus. The more people are tested, the more asymptomatic carriers and vectors are identified.
Also, the “discrepancy” in the numbers is due to the fact that in some countries asymptomatic carriers of the virus are included in the statistics of COVID cases, in others they are not. And sometimes the approach to the state of things changes, and accordingly, the graph of COVID cases may begin to go in one direction or another.
Also, in some countries, for example, in Kazakhstan, double statistics existed for a long time: those who were directly ill and those who were carriers but had no signs of the disease were counted separately. Control over the first group was stricter; for the second group, sanitary and epidemiological measures were weaker. But then a number of such countries nevertheless came to the conclusion that both people with symptoms and those without them should be counted equally.
Another question is that the former require serious treatment, the latter only require fixation (approach as for persons in contact with carriers of the virus) and take appropriate measures (self-isolation). And it is impossible to say unequivocally whether carriers with and without symptoms pose the same or different danger to others. After all, transmission of coronavirus infection is possible not only through coughing and sneezing, but also through small droplets released from the mouth and nose when talking and breathing. Moreover, if a person who is a carrier of the virus but has no symptoms is in a close, poorly ventilated room with another, the chance of becoming infected is always higher. Transmission of the virus by objects cannot be ruled out. Although scientists have a lot of controversy about this.
What percentage of asymptomatic coronavirus carriers in Belarus is currently unknown. And it is becoming increasingly difficult to obtain this data, because if at the beginning of the epidemic PCR testing was carried out not only on people with symptoms, but also on all identified first-level contacts, then from mid-November 20, 1st-level contacts were subject to PCR testing sent only if respiratory signs are present. These signs are determined on the basis of an independent assessment of one’s condition, a survey of a doctor, and, if necessary, a measurement of the level of oxygen in the blood with a pulse meter (saturation), and an examination of the throat.
In Russia, by the way, the situation is similar. From the decree of the head of Rospotrebnadzor dated November 16, 2020, it follows that citizens who have been in contact with patients with coronavirus can now leave self-isolation after 14 days without undergoing a test for COVID-19.
True, data can also be obtained based on a study of a sample of individuals who have developed antibodies. But even here, not everything is clear. There is no exact data yet on how long they remain in the body.
Cough is the most common reason for visiting a doctor among respiratory manifestations; its feature is heterogeneity - development as a result of various factors. The scientific literature describes 53 possible causes of cough [1]. Establishing the etiology of cough is extremely important, since it is the elimination of its root cause that largely ensures the success of treatment. Acute cough is most often a symptom of a respiratory viral infection, lasts no more than 2 weeks, can be successfully treated and does not lead to serious complications. The cause of a persistent, difficult-to-treat cough is more difficult to determine, and in some patients there may be more than one factor causing the cough. Even in developed countries with a high level of healthcare, in more than 20% of cases the source of chronic cough remains unknown [1–8].
An intense dry cough as a result of a strong forced release of air from the respiratory tract significantly increases intrapulmonary and intrathoracic pressure, which reduces the flow of air into the alveoli, can contribute to the development of emphysema of the pulmonary tissue, the formation or enlargement of hernias, and has a negative impact on the functioning of the cardiovascular system. A tense cough often contributes to the development of heart rhythm disturbances; rare complications of cough are described as hemorrhages in the brain and retina in patients with vascular pathology. Against the background of increased intrathoracic pressure at the time of coughing, some patients develop bettolepsy - a short-term loss of consciousness or convulsions. In some cases, patients with intense long-term cough complain of fatigue, malaise, insomnia, voice changes, somatic pain, sweating, and urinary incontinence. Thus, persistent long-term cough significantly worsens the quality of life [1-3, 6, 7, 9].
One of the pathological varieties of cough is its reflex form, which is a symptom of a disease outside the pathology of the bronchopulmonary system. Reflex cough is a neurotic condition manifested by a dry paroxysmal cough during the day or night. Over time, a long-lasting cough almost always acquires a reflex character due to changes in the functional state of cough receptors and corresponding nerve centers [4, 5, 9, 10]. Coughing attacks may be accompanied by laryngospasm, a feeling of suffocation, and do not respond well to classical treatment methods. This condition can mimic bronchial asthma or be combined with it.
According to our clinic, in recent decades there has been an increase in patients with reflex cough, which corresponds to a general increase in the frequency of development of various neurotic conditions. A reflex cough can be of both central and peripheral origin, developing accordingly with pathological irritation of the cough center of the medulla oblongata or peripheral receptors of the vagus nerve. A number of researchers indicate that a reflex cough is formed against the background of neurogenic hyperventilation syndrome (HVS), while concomitant pathological processes are provoking factors for its manifestation. This point of view is confirmed by the results of our previous studies. This explains the long-term persistence of reflex cough even after the elimination of the factors that provoke it [4, 5, 9—11].
It is known that HVS is caused by psychogenic or organic (5% of cases) dysfunction of the central nervous system, manifests itself in various clinical disorders and leads to the formation of a stable pathological type of breathing, but to date the reasons for the development and maintenance of this syndrome remain unclear. Hyperventilation - an increase in the depth and frequency of breathing - disrupts gas exchange processes in the lungs, causes excessive release of carbon dioxide, the development of hypocapnia with a decrease in the partial pressure of carbon dioxide in the alveolar air and respiratory alkalosis. Unconscious, too deep and frequent breathing causes such patients to feel a lack of air. It is respiratory alkalosis, along with a decrease in the level of ionized calcium, that causes an increase in the level of neuromuscular excitability, including spasm of the laryngeal muscles, and provokes coughing attacks [9-12].
Signs of a reflex cough are its dry, hacking nature, gradual increase or sudden onset, inability to stop the attack, feeling of lack of air. It is characteristic that patients themselves localize the place of onset of reflex cough in the area of the anterior surface of the neck. Factors that trigger the onset of an attack include deep breathing, talking, stressful situations, smoke inhalation, and fatigue. In addition to coughing, patients are concerned about dryness and sore throat, a feeling of lack of air and a “lump in the throat.” Against the background of HVS, various pathological changes can develop not only in the respiratory tract, but also in the cardiovascular and digestive systems, psycho-emotional status, thermoregulation, as well as motor disorders, tetany [10, 11]. Paradoxical manifestations of hyperventilation syndrome are periodic sighs, arrhythmic breathing, unmotivated yawning, snoring, licking lips, and coughing. Such signs, in the absence of deep respiratory movements, often do not attract the attention of doctors and patients, but can support hypocapnia and respiratory alkalosis [8, 10-12].
A reflex cough can develop against the background of inflammatory diseases of the ENT organs, with unilateral paralysis and paresis of the larynx, prolapse of the membranous part of the trachea, pathology of the pleura, pericardium, thyroid gland, gastrointestinal tract, the presence of a diaphragmatic hernia, increased sensitivity of the body to any substance, including allergies due to taking angiotensin-converting enzyme inhibitors. We observed patients whose trigger for reflex cough was surgery under anesthesia, childbirth, or tracheostomy. A dry paroxysmal cough can persist for a long time in patients after infectious processes such as whooping cough, mycoplasma and chlamydial infections, influenza and others. Against the background of whooping cough (pathogen Bordetella pertus sis
) cough is caused by constant irritation of the receptors of the respiratory tract, which leads to the formation of a focus of excitation of the dominant type in the respiratory center and its preservation for several years. In addition, the neurotropic pertussis toxin affects the cough center in the medulla oblongata and contributes to the formation of a vicious circle. Attacks of spastic whooping cough and post-whooping cough can also be provoked by nonspecific irritants [1-3, 5, 9-12].
Assessing the characteristics and parameters of cough against the background of various diseases helps the doctor make the correct diagnosis for a particular patient. It is necessary to conduct a thorough differential diagnostic search, including with the participation of various specialists - pulmonologist, cardiologist, otolaryngologist, endocrinologist, neurologist, psychiatrist. Undoubtedly, it is difficult to diagnose a type of reflex cough - psychogenic, especially in the absence of any organic disorders and when the patient is confident in the presence of a causative disease of the respiratory tract.
When examining patients with reflex cough during medical history collection, it is extremely important to pay attention to the presence of a chronic psychotraumatic situation, the occurrence of coughing attacks against the background of stress, increased physical or prolonged vocal stress. An attack of reflex cough usually begins with a sharp dryness and soreness in the throat. When performing laryngoscopy, you should pay attention to such characteristic signs as an increased pharyngeal reflex, a wide glottis - 20 mm or more (usually up to 15 mm), spasm of the vocal folds during inspiration, sometimes convulsive closure of the vocal folds, the occurrence of a coughing attack at the time of examination . When studying the function of external respiration, moderate hyperventilation is detected in 1/3 of patients, while in the rest, the indicators remain within normal limits. Additional diagnostic criteria are a positive hyperventilation test and an electromyographic test for latent tetany, a low level of ionized calcium in the blood, and the lack of effect from the use of antitussive drugs [9–11].
The management tactics for such patients are largely determined by the etiotropic factor; if possible, it must be eliminated. It is also advisable to prescribe symptomatic (cough suppressant) and sedative medications. Doctors have at their disposal antitussive drugs of central, peripheral and combined action. Irrational use of antitussive, mucoactive, antibacterial and anti-inflammatory drugs, including hormonal drugs, and repeated diagnostic procedures can contribute to the development of side effects, lead to unsatisfactory results and adverse iatrogenic consequences. Treatment of such patients should be personalized, using pharmacotherapy, non-drug methods, and in some cases the possibility of surgical intervention is discussed [1, 9, 10, 12-15].
Our clinic has accumulated some experience in treating patients with laryngoneurosis in the form of reflex cough. Based on a fairly large volume of clinical data (more than 500 patients), we came to the conclusion that the management of such patients should include identification and elimination of the causative factor, breathing exercises to relieve hyperventilation, sedation and psychotherapy, reflexology - intradermal novocaine blockade of the Zakharyin-Ged zones for larynx and auricular reflexology, B vitamins, calcium supplements as indicated. The doctor needs to establish psychological contact with the patient, explain the mechanism of development of the disease and convince him of the effectiveness of treatment, as well as the absence of the risk of suffocation. The patient’s understanding that all pathological manifestations are caused by an excess, not a lack of air, and strict adherence to the doctor’s recommendations are extremely important for recovery. Breathing exercises involve switching to the diaphragmatic type of breathing, shortening the time of inhalation relative to exhalation by half, and reducing the breathing rate. The method of intradermal novocaine blockade of the Zakharyin-Ged zones for the larynx was developed and patented by an employee of our clinic, Prof. O.Yu. Karpova [16] and is based on the idea that internal organs and their corresponding dermatomes are associated with the same structures of the central nervous system. When exposed through novocaine blockades to skin receptors in the corresponding Zakharyin-Ged zones, inadequate impulses from the pharynx and larynx are reduced, the central pathological dominant is gradually eliminated and the normal function of the interested structures is restored, which is manifested by the cessation of reflex cough.
Currently, in the Clinic of Ear, Nose and Throat Diseases of the First Moscow State Medical University named after. THEM. Sechenov examined and successfully treated more than 500 patients with reflex cough. Clinical manifestations and anamnestic data, as well as a laryngoscopic picture (anatomically wide glottis, spasm of the vocal folds during inspiration, high pharyngeal reflex) confirmed the diagnosis. Considering that the psychogenic factor plays a significant role in the occurrence of reflex cough, 26 patients underwent a psychodiagnostic study using the SMOL-EXPERT computer system.
In 22 cases, a change in personality structure was revealed with a predominance of psychasthenic, hypochondriacal and depressive changes. Internal tension, decreased mood and anxiety, and increased sensitivity to stress were the leading personality traits. In 4 patients, hysterical-hypochondriacal radicals were determined; therefore, they were characterized by anxious and suspicious traits and a predisposition to anxious reactions to any events [17]. Also, before the start of treatment, patients were monitored the level of ionized fraction of calcium in the blood.
All patients underwent complex treatment, including 10 procedures of intradermal novocaine blockade of the Zakharyin-Ged zones for the larynx and auricular reflexology, breathing exercises aimed at relieving hyperventilation, sedatives, muscle relaxants to relieve pathologically increased tone of the laryngeal muscles, calcium supplements as indicated, as well as antitussive drugs.
In 2021, the use of the drug rengalin began as part of complex therapy for patients with reflex cough. Rengalin contains polyclonal, affinity-purified antibodies to bradykinin, histamine and morphine in the form of technologically processed (potentiated) ultra-high dilutions. The drug is release-active, i.e. it has a special modifying activity that is released during the technological processing of the original antibodies. Antibodies to bradykinin, histamine and morphine in a release-active form are capable of changing the activity of endogenous regulatory molecules, and therefore the processes associated with them. A special feature of the drug is its ability to influence the central and peripheral parts of the cough reflex, changing the interaction of endogenous regulators with the corresponding receptors involved in the formation of cough. The components of the drug modify the activity of the ligand-receptor interaction of endogenous regulators (opioids, histamine and bradykinin) with the corresponding receptors; in this case, the combined use of the components leads to an increase in the antitussive effect. In addition to the antitussive effect, the complex drug rengalin, due to its constituent components, has anti-inflammatory, decongestant, antiallergic, antispasmodic and analgesic effects. Unlike narcotic analgesics, it does not cause respiratory depression, drug dependence, and does not have a narcotic or hypnotic effect. Rengalin is indicated for adult patients and children over 3 years of age with acute and chronic respiratory tract diseases, accompanied by cough and bronchospasm, for any cough against the background of influenza and ARVI, acute pharyngitis, laryngotracheitis, acute obstructive laryngitis, chronic bronchitis and other infectious-inflammatory and allergic diseases upper and lower respiratory tract.
In the Clinic of Ear, Nose and Throat Diseases of the First Moscow State Medical University named after. THEM. Sechenov, 15 patients with reflex cough received the previously proposed complex conservative treatment in combination with the innovative drug rengalin. The age of the patients ranged from 28 to 76 years. The duration of the disease history ranged from several weeks to 6 years. 3 patients had concomitant unilateral recurrent laryngeal nerve palsy, 2 had a history of whooping cough. The main complaint of all patients was a prolonged unproductive paroxysmal cough, periodically interrupted by laryngospasms; they were also concerned about a feeling of lack of air and rapid voice fatigue. The severity of cough was assessed by patients on a scale from 0 to 10 during the day and at night, depending on the frequency and intensity of attacks (according to the “Cough Severity Scale”); the provoking factor was also taken into account.
The duration of the study was 10 days, during which patients received Rengalin 2 tablets 3 times a day and filled out a questionnaire, noting the frequency of coughing attacks, the impact of symptoms on daily activity/sleep, recording factors that provoke the development of a coughing attack, monitoring the presence or absence of sputum, as well as voice changes. The average cough severity score at the beginning of treatment was 6.2 points during the day and 3.5 points at night. The most common triggers for paroxysmal dry cough in patients were talking, laughing and physical activity.
All patients showed a significant improvement in their condition on average from the 3rd day of therapy, with the exception of one patient, who on the 8th day of treatment experienced the appearance of acute catarrhal symptoms, as well as stress, against the background of which the severity of the cough began to increase again. Complete recovery was observed in 6 patients on the 10th day of treatment. Our results demonstrate the effectiveness of the drug rengalin against cough of a reflex nature as part of complex therapy.
Thus, in our opinion, the treatment of patients with reflex cough and laryngoneurosis should be carried out by an otorhinolaryngologist who has the necessary skills in diagnosing and treating such a contingent of patients, including methods of reflexology, breathing exercises and psychotherapy. In cases where a reflex cough is only one of the manifestations of severe general neurosis, it is advisable to refer patients for treatment to a psychoneurologist. When a reflex cough is combined with another pathology, its relief is necessary, since the elimination of this pathological symptom facilitates the course of concomitant diseases and improves the quality of life.
The authors declare no conflict of interest.
*e-mail: [email protected] ; https://orcid.org/0000-0001-7414-1293
What is the incubation period for coronavirus infection?
The incubation period for coronavirus infection in most cases is up to 10 days. The first wave was considered to be up to 14 days . In some isolated cases, the incubation period lasts about 20 days.
The highest chance of becoming infected is from a person who is a carrier of coronavirus, but until the disease is recognized - 1-2 days, as well as from a person who has been sick with COVID-19 for 1-4 days. 95% of patients thus fall within the range of two to six days. During the incubation period, SARS-CoV-2 does not manifest itself in any way.
Another difficulty is that if coronavirus is without symptoms, it is difficult to give an objective assessment of which day of illness is the first.
By the way, if we compare the incubation period of coronavirus infection and influenza, then the latter has a shorter incubation period. In the latter case, in most cases it lasts a day or two.
More and less common symptoms
The most common symptoms with which the disease begins are respiratory (fever, cough, sore throat). At first, the disease is easy to confuse with the flu, sore throat, or acute respiratory infection.
Among the common symptoms is the loss of the ability to recognize smells (but it is important to understand that this is not an indicator, there are patients who have this symptom, but do not get sick with coronavirus, and there are people who have a moderate and severe form of the disease, but they have no taste differentiate).
If the disease progresses quickly, shortness of breath (feeling of lack of air, difficulty taking a deep breath), and chest pain are immediately added.
More rare are symptoms of a dermatological nature (rashes on the body, mucous membranes), nausea, vomiting, diarrhea, hemoptysis, unbearable headache.
Also not the most common symptoms in patients with coronavirus, but related to its symptoms, are swollen veins, cyanosis of the skin, and surges in blood pressure.
Let us consider which of these symptoms appear first, how symptoms change from day to day, whether there are differences in the manifestation of symptoms in adults and children, what you need to remember if your sense of smell has disappeared.
Symptoms
The clinical picture of bettolepsy is variable in severity not only in different patients, but also in one patient during different attacks.
Typically, an attack of coughing syncope is accompanied by the following symptoms:
- a coughing attack occurs while standing or sitting, while eating or immediately after eating;
- cough can be triggered by strong odors, cold air, excessive laughter, frequent sneezing, defecation, heavy lifting, or tobacco smoke;
- against the background of a cough, the patient’s face turns red and then turns blue, veins swell in the neck;
- sometimes a harbinger of an attack can be mild dizziness that occurs against a background of coughing;
- in the first minute of a cough attack, signs of fainting appear or loss of consciousness occurs, accompanied by a fall of the patient and cyanosis of the skin;
- after fainting, the skin becomes pale and the cough stops;
- the duration of fainting is several seconds or minutes;
- after this, the patient quickly returns to consciousness and recovers from the seizure (usually without medical assistance).
In some cases, an attack of coughing syncope is accompanied by convulsions, which are usually limited to one part of the body (for example, twitching in the limbs). Tongue biting is not observed during convulsions caused by bettolepsy. In rare cases, a seizure may lead to urinary or fecal incontinence.
During an episode of bettolepsy, the patient may sometimes experience the following symptoms:
- amnesia;
- headache;
- pain in the neck area.
Some experts identify the following variants of cough-brain syndrome:
- A seizure develops at the peak of coughing and is accompanied by sudden deep fainting and a fall of the patient.
- The seizure is accompanied by convulsions and, sometimes, involuntary bowel movements or urination.
- The seizures initially occur as in bettolepsy, and then are replaced by petit epileptic seizures, which can develop independently of the cough.
- Seizures of bettolepsy in patients with organic brain pathologies, accompanied by severe autonomic disorders.
- Seizures of bettolepsy in patients with a history of typical epilepsy.
What is the first symptom of coronavirus?
Various symptoms can be the first to make themselves felt. But, as a rule, these are respiratory manifestations.
- Fever. In some patients the temperature is immediately above 38 °C, in some patients it is low-grade: 37.1 – 37.3 °C.
- A sore throat. Moreover, as a rule, the back wall of the throat hurts more. At the same time, there is an unpleasant taste in the mouth.
- Dry cough. A person cannot “clear his throat.” His sputum does not come out.
- Fatigue. Malaise even after minimal physical exertion.
- A slight runny nose (at first it was believed that if you have a runny nose, then it’s not Covid), but later it turned out that everything was very ambiguous. A runny nose during COVID makes itself known less often than a dry cough, but its presence or, on the contrary, absence, cannot be a signal for an accurate diagnosis.
Among the first symptoms of coronavirus is anosmia – loss of smell. At the same time, like respiratory symptoms, loss of smell or taste cannot be called a direct “indicator” of COVID-19. The same symptoms are characteristic of neurological patients (for example, this symptom is common in those suffering from Alzheimer's disease). And in some cases, this is not a sign of pathology at all, but a sign of aging (more often in men). True, if before 2020 they did not pay much attention to it, then with the mass circulation of information that this is a symptom of coronavirus, many began to focus on it. Also, people who have suffered head injuries or nasal polyps often experience loss of smell.
However, some patients are only concerned about loss of smell and fatigue. This audience is classified as patients with mild symptoms of coronavirus.
Coronavirus symptoms without fever
Without fever, coronavirus is more common in children than in adults. In this case, against the background of the absence of temperature, the patient can experience the entire symptomatic spectrum, as in a patient with fever. Starting from a sore throat, and up to coughing, severe muscle pain, severe weakness (weakness).
Moreover, if adults have symptoms of coronavirus without fever, two radically opposite “scenarios” are possible.
- The disease occurs in a mild form.
- The functioning of the immune system is disrupted. After all, it is important to understand that behind the rise in temperature lies the body’s mechanism for fighting the disease, working to prevent complications (for example, in the form of pneumonia).
Often, frail elderly people have no fever during COVID. Their hypothermia is often caused by regular use of drugs to treat cardiovascular diseases.
Among people who suffer from viral infections without fever, there are also many who suffer from thyroid pathologies. And the reason for this is either the improper functioning of the thyroid gland itself, or the use of drugs aimed at correcting its function.
Hypothermia is also often observed in allergy sufferers who regularly have to take antihistamines, and in people who have recently suffered any bacterial infections and have been treated with antibiotics for a long time. Moreover, these could be both infections of the respiratory tract and, for example, the genitourinary system.
Despite the fact that in weakened elderly people the disease can occur without high fever, they often have difficulty breathing, many have movement and speech disorders (in this case, the symptoms of COVID-19 are close in symptoms to a stroke, and in some carriers of SARS-CoV-2 This strain is a stroke provocateur).
Remedial measures
If an abnormal condition occurs, surrounding observers should help the patient by placing him in a natural position on his back. The lower limbs should be elevated, thereby allowing arterial blood to flow to the head. The airways should be cleared and the buttons on the neck should be undone. If possible, the air around should be fresh.
Medical manipulations are reduced to reducing blood stagnation in the brain. Correct treatment of cardiovascular diseases is carried out. Cardiotonics, drugs aimed at narrowing vascular channels, and substances that improve the patency of the bronchial passages are prescribed individually. In case of prolonged bradycardia (decreased heart rate), an atropic drug is used. In case of a complex course of the underlying disease, hospitalization is required for subsequent treatment.
Symptoms of coronavirus in children
About 20% of children who are carriers of SARS-CoV-2 do not notice this disease in themselves.
In most children, Covid occurs in a mild form, like a cold: the temperature rises, but is not critical, or the disease goes away without it at all, there is fatigue, a slight cough, and there are no pathological changes in the lungs.
But there are children who have a hard time with COVID-19. Most of them are among babies under one year old (more than 10%). Risk group and age 1-5 years (over 7% of children at this age require serious treatment). But among children and adolescents aged 6 - 16 years, severe disease is typical for 3 - 5%.
With moderate severity, there is lung damage (pneumonia), but there is no shortness of breath. In severe cases of the disease, in almost all cases the temperature is above 35%, problems with the lungs are serious (difficulty breathing, coughing is painful), the skin begins to turn blue. Many people have problems with the stomach and intestines. They make themselves known by diarrhea and vomiting.
Symptoms of coronavirus in infants
The most difficult thing is with symptoms in infants. After all, they cannot say what bothers them, what hurts. Some of the symptoms can easily be attributed to teething, intestinal colic: increased tearfulness, anxiety, problems falling asleep.
At the same time, for example, the same intensity of intestinal colic is a characteristic sign of coronavirus in infancy.
Respiratory manifestations most often boil down to redness of the throat, nasal congestion, coughing, while most infants do not have breathing problems.
In a number of infants, especially if the disease has severe colic, severe fever and repeated vomiting.
Symptoms of coronavirus in preschoolers and schoolchildren
In children of preschool and school age, symptoms are often vague. Many symptoms, at first glance, look like a “typical cold.” But the coronavirus may be hiding behind it. Therefore, children who have even the first signs of a “cold” – a sore throat, runny nose – are advised not to go to school or kindergarten.
Observations also show two trends:
- Among schoolchildren, the highest transmission of the virus is from asymptomatic carriers.
- The spread of the pathogen among children in middle and high school is higher than among children in kindergarten and primary school.
Risk factors for developing symptoms and signs of PA
There are risk factors that precede the onset of panic attacks. These include the mental constitution of a person with an emphasis on general negative affectivity - with a tendency to “get stuck” on negative emotions, to give a negative assessment to almost everything that happens in life. Childhood, the nature of the relationship between parents, and parenting style play an important role in the formation of such an outlook on life.
“Genetic” factor and symptoms of PA
The occurrence of symptoms of panic attacks is influenced by growing up in an unfavorable family environment, where the child witnesses quarrels and violent conflicts between parents. Psychological and physical abuse in childhood, including sexual abuse, is also a risk factor for developing signs of panic attacks. This also includes such strong stress factors as parental abandonment of the child, deprivation of parental rights, and their premature death.
The emotional deprivation of a child with a significant person (son - mother, daughter - father), who provides a sense of security, is the cause of dissonance between sensory and emotional experience. A sure sign of such a situation in the family is overprotection, which cannot replace love for the child. Growing up in such a family creates the preconditions for the development of symptoms of panic attacks due, for example, to the repression of an anxious state, including the fear of being abandoned and, consequently, of dying, and the lack of understanding of its (fear) true causes (unconscious constant anxiety is the norm for such a person).
Clinical statistics also point to a “genetic” factor in the appearance of signs of panic attacks . For example, in children whose mothers suffered from PA, the risk of developing the disease increases significantly. It should be understood that the genetic factor here means not only the possibility of transmitting psychopathology by inheritance, but also its acquisition as a child copying an “anxious response”, or a combination of both. In particular, if parents suffer from mood disorders (eg, anxiety, depression, bipolar disorder), there is also a possibility of symptoms and signs of panic attacks in the child.
“Social” factor and signs of PA
Among the risk factors that provoke the development of symptoms of panic attacks in adulthood are lifestyle and traumatic events that negatively affect a person’s mental health:
- active smoking;
- alcohol abuse;
- drug use;
- side effects of medications;
- surgical intervention under general anesthesia;
- life in constant stress;
- interpersonal, family conflicts;
- divorce, other difficult life situations;
- chronic somatic diseases;
- stay in a military conflict zone;
- road accident;
- being in the zone of man-made and natural disasters;
- death of a loved one.
Among the somatic diseases, the presence of which potentiates the risk of symptoms of panic attacks, it should be noted bronchial asthma, chronic bronchitis, chronic obstructive pulmonary disease, arrhythmia, angina pectoris, hypertension, mitral valve prolapse, hypo- and hyperthyroidism, epilepsy, somatoform disorders, OCD, PTSD .
Covid on the skin
In addition to the characteristic symptoms, a number of SARS-CoV-2 carriers who have recovered from COVID also have dermatological symptoms. Most often these are red and purple bumps and redness on the skin.
- Visually, problem areas resemble areas after frostbite. As a rule, these are shapeless asymmetrical spots on the arms and legs. The formations may hurt and sometimes itch.
- Small blisters on the torso, arms and legs.
- Livedo is a red-blue network of vascular nature.
Dermatological problems can make themselves felt both at the first stage of the disease and when the disease has already developed. If we are talking only about redness and rashes, then they disappear within 2 weeks; if bumps have formed, then they can remain on the skin for several months.
In some COVID patients, the skin begins to peel off at the site of the bumps.
Spots are more typical for children, adolescents, young people, blisters - for middle-aged people, and livedo - for the elderly.
Dermatological manifestations of coronavirus infection are most often associated with overexpression of anti-inflammatory cytokines (peptide molecules), which are responsible for transmitting signals between cells. In fact, there is an “imbalance” in the body’s inflammatory response. But some rashes occur due to constant sweating at high temperatures. Infectious and allergic skin lesions are also possible.
Dental problems
Among the symptoms that were not paid attention to at first, but then noticed in a fairly wide number of patients with coronavirus, is exanthema, that is, a rash on the mucous membranes. Typically in the oral cavity.
Just by the presence of a rash in the mouth, one cannot judge that a patient has coronavirus. At the same time, if this sign is present, but there are no other symptoms, it cannot be ruled out that it is not Covid.
Although in many cases, classic enteroviral vesicular stomatitis may be behind the rash in the mouth. This is also an infectious disease, but it requires its own treatment.
A number of coronavirus patients develop ulcers and red bumps in their mouths, which can begin to bleed in spots.
Fainting causes, methods of diagnosis and treatment
Depending on the mechanism of development, the following types of fainting are distinguished:
Vascular syncope
Accompanied by a sudden decrease in vascular tone, a weak but rapid pulse. It mainly occurs in people with vegetative-vascular dystonia. In this condition, there is constantly low blood pressure and anemia. People of asthenic build, children and adolescents during puberty are susceptible to vascular syncope.
Vagal syncope
Loss of consciousness is characterized by a sharp drop in blood pressure, bradycardia, and asystole. A person's heart rate suddenly decreases, causing a decrease in the volume of blood flowing to the brain. Let it slow down, but not weaken. Vagal syncope occurs in people who have a heavy build or are overweight.
Emotional syncope
Such fainting causes severe stress, fear and other negative emotions. They can appear in a healthy person, but are more common in people with neurosis and vegetative-vascular dystonia. First, general tension arises, then there is concern about dryness in the mouth, general weakness, a pressing feeling in the heart area, paleness of the facial skin, difficulty breathing, trembling of the limbs, eyelids or lips.
Cardiogenic syncope
Cardiogenic or cardiac syncope provokes cardiovascular diseases. This type is considered the most dangerous. It is accompanied by a drop in cardiac output below the critical value required for effective blood supply to the vessels of the brain.
Simple fainting
A simple fainting state is characterized by gradual development. Loss of consciousness causes blurred vision, nausea and dizziness. At the same time, blood pressure decreases, the pulse weakens, the pupils become wider and react less well to light, and the skin turns pale. The duration of a simple faint is 25-45 seconds.
Convulsive fainting
Against the background of autonomic dysfunction and low muscle tone, tonic convulsions occur, provoking convulsive fainting. In addition to convulsions, a person may experience blue or redness of the face. Sometimes isolated muscle twitching may occur.
Orthostatic syncope
Occurs when the body rises sharply from a sitting or lying position. Accompanied by darkening of the eyes and loss of coordination. Primary autonomic failure, prolonged bed rest, and sympathectomy predispose to this type of syncope.
Fainting during pregnancy
Presyncope during pregnancy occurs due to three main reasons:
- decreased hemoglobin and the development of anemia;
- low blood pressure;
- lack of circulating blood for the woman and fetus.
Thromboembolism
Another common phenomenon that is important to consider when talking about symptoms is thromboembolism. It encounters many patients with moderate and severe forms of coronavirus.
Many people know about the serious consequences of thromboembolism. Not everything is about how she manifests herself.
Among the characteristic signs of thromboembolism:
- swelling of veins, often cervical
- blueness (cyanosis) of the face,
- drop in blood pressure.
However, again, these symptoms cannot be considered a direct signal of COVID-19. In addition to coronavirus, thromboembolism can be caused by injuries, varicose veins of the legs, the presence of a catheter, diseases associated with heart rhythm disturbances, malignant tumors, prolonged bed rest, and surgery with large blood loss. Also among the risk factors are old age, taking contraceptives and pregnancy.
In some patients, thromboembolism is not a symptom, but a complication. Most often, this again happens in older people and pregnant women. In addition, people with respiratory and heart failure are vulnerable, as well as those whose coronavirus has damaged the endothelium of blood vessels (a monolayer of vascular epithelial cells).
True causes and provoking factors
Hypoxia—oxygen starvation of tissues, in this particular case of the brain, is caused by any relatively long-term condition accompanied by:
- or a mechanical obstruction to breathing - the flow of oxygen;
- or caused by a lack of oxygen in the blood for another reason (defect of red blood cells in some anemias, for example).
In the variant of bettolepsy, these two factors in the development of hypoxia are combined. This is a mechanical obstruction of the airways damaged by acute or chronic pathology, and a prolonged period of circulation of oxygen-poor blood.
Time measured in minutes. Time that may be sufficient for the onset of irreversible changes in the brain.
Let us add to this basis what developed by the age of 40-50, but at an earlier age, coughing fainting does not develop - atherosclerotic degeneration of blood vessels, which in itself is the cause of chronic hypoxia. As well as associated episodes of excessive blood pressure. And also arrhythmia - momentary or permanent.
It is worth adding two more strokes to the canvas, adding the following to the causes of bettolepsy:
- endocrine pathology in the form of diabetes mellitus;
- chronic allergies to everything, which developed, among other things, as a result of excessive addiction to taking medications.
When there is excess glucose in the blood, as well as when aggressive substances appear in it, either released during an allergic reaction or necessary to extinguish it, the biochemical composition of the blood and its properties change in the same way as with mechanical suffocation due to respiratory tract pathology.
Anyone who has all these treasures of dubious value has an unusually high risk of developing cough epilepsy.
But... not everyone faints with a cough! And only 2% of adults experience various types of paroxysmal conditions! And children never suffer from this disease (with the exception of cases where whooping cough serves as a background).
Why?
For the development of cough fainting, one more condition is necessary - the presence of pathological impulses from reflexogenic zones:
- respiratory system;
- larynx (in particular, the areas of activity of the superior laryngeal nerve);
- carotid sinus, jugular veins, aorta;
- venous sinuses of the brain.
The reaction from the pressoreceptors located in these reflexogenic zones is a necessary link that closes the fatal chain - pathological impulses from them lead to an increase in the activity of the vagus nerve, contribute to the onset of bradycardia and the manifestation of a dangerous condition - Morgagni-Adams-Stokes syndrome.
The hand of fate, or who inevitably gets sick
Accordingly, the causes of the development of bettolepsy include conditions with phenomena of increased intrathoracic pressure, as well as cerebral hypoxia, leading to disorders in the activity of the nervous system. Other provoking disorders, diseases and conditions:
- diseases of the respiratory system in the form of bronchial asthma, chronic bronchitis with an asthmatic component and outcome in pulmonary emphysema, fibrous-cavernous form of pulmonary tuberculosis, laryngitis, whooping cough;
- status that occurs during aspiration of small objects into the larynx, trachea;
- neuralgia of the superior laryngeal nerve;
- pathology of the cerebral arteries and veins in the form of vascular anomalies, compression of the vertebral arteries by osteochondrosis or atherosclerotic deposits;
- household chronic poisoning – drug addiction and alcoholism.
Factors that provoke cough fainting should also include some habits and features of life in the form of:
- wearing tight-fitting clothing;
- habits of quickly changing posture (with sudden jumping up after prolonged sitting);
- "passive smoking";
- tendency to anxious and suspicious, “psychically suffocating” states.
Why you might lose consciousness:
Tunnel consciousness, panic attacks
Among the signs of coronavirus in people with severe forms of the disease is tunnel consciousness. A person cannot concentrate on anything. He focuses only on the disease and the fears around it. He does not focus on recovery, “here and now,” but obsessively searches for the reason why he got sick, suicidal thoughts are possible.
Among the mental manifestations of coronavirus are panic attacks . Women suffer from panic attacks twice as often as men.
A panic attack is not just a feeling of anxiety, but pronounced fear, which is accompanied by a number of physically unpleasant sensations. Among them are increased sweating, trembling of fingers (tremor), nausea, upset stool, and chest pain.
The most informative evidence that this is a symptom of Covid or a classic panic attack is obtained by a test (smear), but there are also a number of other signs. The role is played by whether such signs are observed for the first time and how long the panic attack lasts. If this is a true panic attack, and not a symptom of COVID, then 15 minutes after the onset of the attack the person begins to “let go,” especially if you take deep breaths.
With COVID, this exercise most often does not help. After all, the reason is a lack of air, depression of respiratory function, and in this case only saturation of the lungs with oxygen helps to cope with the attack.
Symptoms and signs of panic attacks
In the clinical picture of the disease, the leading symptoms and signs of panic attacks are strong fear that cannot be rationalized, disturbances in the functioning of the respiratory organs and cardiovascular system, and other phenomena of a vegetative nature. As a rule, the attack occurs instantly and lasts about 15–30 minutes.
The incidence of panic attacks varies from moderate (F41.00, ICD-10) to severe (F40.01, ICD-10). Moderate episodic paroxysmal anxiety corresponds to - from 4 attacks over a distance of 28 days; severe - at least 4 attacks in 7 days at a distance per month.
As a rule, the individual picture of an attack includes the following symptoms and signs of panic attacks:
- cardiopalmus;
- chest discomfort;
- tingling in the heart area;
- rise in blood pressure;
- feeling of lack of air;
- labored breathing;
- dizziness;
- sweating;
- “waves” of heat and cold;
- nausea;
- diarrhea (sometimes).
Objectively, during an attack, those around you can record a change in the color of the skin, sweating, a rise in blood pressure, a high pulse rate, difficulties with coordination of movements, and tremors. However, both the person himself and the people around him usually mistake the symptoms of panic attacks for signs of a heart attack or stroke (especially at the onset - the first attack of PA).
In some cases, with a weak mental constitution (low threshold of resistance to stress factors), a severe panic attack can lead to loss of consciousness. With repeated attacks of PA, anticipatory anxiety develops quite quickly, expanding the range of negative experiences with the fear of expecting an attack. In addition, agoraphobia and restrictive behavior may appear in the clinical picture.
Rice. 1. The mechanism of a panic attack.
Symptoms of panic attacks in women
Clinical practice shows that women are more susceptible to episodic paroxysmal anxiety than men. The symptoms of panic attacks in women are not much different from the signs of the “male” version of the disease. However, they still affect the health and adjust the life of an adult woman.
The main symptoms of panic attacks in women include:
- menstrual irregularities;
- other endocrine disorders affecting reproductive function;
- increased risk of developing neurotic and depressive disorders;
- alcoholism according to the female type.
In addition, the development of the disease can cause disruption in a woman’s functioning in the family, even leading to the risk of divorce proceedings. Indirectly, the disease inevitably affects both men and children, becoming the cause of “secondary” psychopathology, including developmental disorders of the mental apparatus in children.
Symptoms of panic attacks in men
Symptoms of panic attacks in men can radically change a person’s life, masking the disease under character traits, lifestyle, or unusual creeds. Outside of marriage, it is quite difficult for such a person to maintain a relationship; in marriage - to preserve the family or relationships in it, to create favorable conditions for raising children, the healthy development of their mental apparatus.
Typical symptoms of panic attacks in men that affect quality of life include:
- problems with potency;
- risk of developing severe depression with suicidal tendencies;
- rapid alcoholization, interest in surfactants.
If the picture of the disease is dominated by depressive tendencies, alcoholism or addiction to psychoactive substances quickly develops, and there is a high risk of suicidal tendencies. Most successful attempts to commit suicide during the course of the disease are observed in men.
Symptoms of panic attacks in teenagers and children
As a rule, severe symptoms of panic attacks in adolescents can be detected between the ages of 7-10 years. First of all, they manifest themselves in an unusual deterioration in the well-being of children, a decrease in mood and activity. Within an educational institution, such a child may become a victim of bullying or violence from classmates, fall behind in academic performance, and withdraw into himself.
Symptoms of panic attacks in adolescents that occur against a background of increased anxiety or fear attacks include:
- decreased tone;
- fast fatiguability;
- frequent headaches;
- gastrointestinal disorders;
- increased sweating;
- cardiopalmus;
- pain in the heart area;
- dyspnea.
Unfortunately, symptoms of panic attacks in children are not detected in a timely manner. Parents can search for a long time for the true reason for the deterioration of their child’s well-being, visiting doctors of various specializations year after year, ignoring treatment for panic attacks by a child psychiatrist or neuropsychiatrist. However, having learned to cope with attacks of PA, such a child becomes “adapted” only externally, maintaining psychopathology in potency. Having entered adulthood, such children have a high probability of relapse of the disease and, consequently, its development.
Rice. 2. Types of reaction to stress and panic attack.
Headache
8% of COVID-19 patients have headaches. Their intensity is quite strong even if there is no high temperature at the same time.
As a rule, ordinary antispasmodics, painkillers such as nemisulide, analgin for pain arising from COVID do not help much.
With such pain there are no other typical signs for other pathologies (for example, dizziness, as with hypertension, vegetative-vascular dystonia). However, the nature of headaches with Covid is also of a vascular nature. The virus negatively affects vascular endothelial cells. There are problems with blood flow. The lumen of blood vessels narrows significantly. A headache in this case is a signal of a lack of oxygen. And if this deficiency is replenished, then the headache problem is solved.
By the way, when pathologists autopsy the bodies of those who died from coronavirus and micrograph the brain, sharply narrowed blood vessels and signs of inflammation are visible. The vessel becomes unable to properly supply the brain with blood.
And also, as practice shows, about 1% of headaches during a pandemic are completely false. Suspicious people experience headaches when reading news about coronavirus, hearing news that one of their friends has contracted coronavirus (even if there was no contact with him).
Causes
Cough syncope occurs due to disorders of the internal organs:
- Pulmonary diseases: bronchial asthma, cor pulmonale, tuberculosis and emphysema. With pulmonary diseases, blood stagnates in the pulmonary circulation, which causes cardiopulmonary failure.
- Diseases and pathological conditions of the upper respiratory tract: whooping cough, foreign bodies entering the bronchi. During attacks, oxygen does not reach the lungs. Hypoxia of the brain occurs, the person loses consciousness.
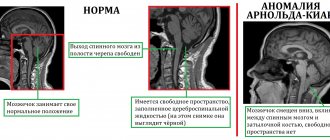
- Brain pathologies: dyscirculatory encephalopathy, arteriovenous malformations, previous traumatic brain injuries, increased intracranial pressure.
- Peripheral nervous system disorders. When the laryngeal nerve is inflamed, the vagus nerve is activated due to the generation of a large number of electrical impulses. The number of heart contractions decreases and cardiac output decreases. The brain receives less blood and the person loses consciousness.
These risk factors increase the likelihood of developing betolepsy:
- smoking;
- sedentary lifestyle;
- diet without vegetables and fruits;
- alcoholism, drug addiction.
The exact pathophysiological mechanisms are unknown. However, the hemodynamic theory has the most supporters. To understand the mechanism of development of cough syncope, you need to understand the mechanism of cough. It consists of three acts:
The first act is inspiratory. Characterized by closure of the larynx. The second act is compression: the muscles of the chest and abdomen contract, the diaphragm is fixed in a static position. The third act is expiratory: high pressure is created, which pushes air out at high speed with the larynx open.
In the second and third phases, intrathoracic pressure increases. With a normal cough, the pressure increases from 40 to 100 mm Hg. During syncopal cough, the pressure tends to 200-300 mmHg. Due to such indicators, intra-abdominal pressure increases. This results in decreased blood flow to the heart. As a result, the amount of blood ejected by the heart decreases and systolic blood pressure decreases. Blood flow to the brain decreases. In neurons – hypoxia and ischemia. Due to lack of oxygen to the cortex, a person loses consciousness.
There are continuous and intermittent coughs. In the first option, a coughing attack occurs that lasts several seconds. Between acts of coughing, a person cannot inhale air. Because of this, the number of impulses to baroreceptors decreases, and the resistance of peripheral vessels reflexively increases.
With an intermittent cough, a person inhales air before each coughing act. This irritates the baroreceptors and decreases peripheral resistance.
These mechanisms lead to difficulty in venous outflow from the brain. Intracranial pressure increases. The minute volume of blood circulation in the cerebral arteries decreases. The bleeding may stop completely. Due to hypoxia, syncope occurs.
Conjunctivitis with COVID
Some patients with COVID have pronounced conjunctivitis, while others do not have any traces of it.
Most often, signs of conjunctivitis are present in those individuals in whom the virus entered the body through the eyes. This is why not only masks are so useful, but also safety glasses and shields.
All types of conjunctivitis are visually similar. It is especially difficult to distinguish between different types of viral conjunctivitis (viral conjunctivitis - not necessarily caused by a strain of coronavirus). But viral conjunctivitis can be distinguished from bacterial conjunctivitis even without tests.
In the field of attention is what is separated from the eyes. If it is bacterial, it is dense, white, yellow, and if it is viral, it is watery.
It is also worth paying attention to the parotid lymph nodes. With viral conjunctivitis, the lymph nodes in most cases are painful when palpated.
Speech and movement disorders
Speech and movement disorders due to coronavirus can be observed in severe forms of the disease and direct entry of the virus into the brain.
The diagnosis in this case is COVID-19-associated necrotizing hemorrhagic encephalopathy.
Her symptoms are similar to hemorrhagic encephalopathy caused by strains of the Coxsackie A virus and H1N1 influenza.
The frequency of words in speech changes, perseverations arise - repetitions of individual words and even phrases, some phrases begin to be “swallowed”, errors in cases and word order in a sentence begin, problems arise with muscle articulation (it becomes difficult for a person to repeat a simple tongue twister even at a slow pace. Coordination of movements is also impaired.
Coronavirus symptoms by day
If the disease has symptoms, then it proceeds through certain phases. And each phase is characterized by its own symptoms.
Days 1-4 – phase 1 . In this phase, the following signs most often manifest themselves: fever, muscle pain, sore throat, dry cough. If the body is amenable to treatment, then improvement may begin after the 1st phase. Either the person recovers, or for another week or a week and a half there is a sluggish cold - often without a high fever, but with a “stuffed” throat, a slight cough, and fatigue.
5-10 days – 2nd phase . If the body cannot cope with the disease, then on the 5-6th day a new phase begins, which is characterized by a lack of air and the development of pneumonia. If timely measures are taken, including providing the patient with oxygen support, respiratory failure can be overcome by the 10th day of illness. As a rule, oxygen support is prescribed when saturation changes and oxygen levels are below 94-90%. In hospitals in Belarus, oxygen is supplied into the nose through a cannula, as a rule, when the oxygen level is less than 93%.
The unpleasant thing is that on the 4th day, some patients begin to believe that they are getting better (the criterion is that the cough has become wet, not dry). But a wet cough does not always mean a healthy cough. In some cases, the appearance of sputum is the result of fluid accumulation in the alveoli, and this is precisely followed by a violation of oxygen metabolism. That is why temporary relief on the 5th day may be followed by deterioration, and the 2nd phase is then inevitable.
If the patient's water-electrolyte balance is disturbed, then on days 5-10 convulsions, spasms in the gastrointestinal tract, and insomnia may also appear.
Day 10-12 – phase 3 . On the 10-12th day, in most patients the temperature returns to normal, but muscle pain and a feeling of lack of air may remain. In this case, the respiratory function is restored in some patients, while in others shortness of breath remains the main companion.
Days 13-20 – phase 4 . In this phase, symptoms remain, as a rule, in patients with severe disease. At this moment, there is a high risk that complications from the heart, kidneys, or heart may occur.
On the part of the kidneys, this is, for example, a drop in diuresis (urine volume), inhibition of consciousness; on the part of the heart, inflammation of the heart muscle. If a patient has a weak liver or has chronic diseases of this organ, then the risks of their exacerbation are high.
It is important to understand that different patients may have different “scenarios” for the development of the disease. There are cases when a coronavirus infection is asymptomatic, but then, after a person has formed antibodies, pneumonia develops. This is not a typical option, but it also occurs.
The course of the disease can be relatively mild, moderate or severe.
- Light form . Symptoms last 4-14 days. Limited to phase 1 (see above). For a number of patients, a mild form of coronavirus ends with a complete recovery, while a number have difficulties with the respiratory system (there is still a cough), liver (ALT levels increase), and kidneys. But there is no exact data on whether the coronavirus or intensive care is to blame for most problems. After all, the same level of ALT can be increased by paracetamol, antibiotics, aspirin - drugs that are important for treating COVID-19 itself, relieving symptoms, stopping the development of the disease, and they cannot be canceled, this is a greater risk for the body. But after a person has had COVID-19, it is important to monitor these indicators and support the liver and kidneys. If there are no serious chronic diseases of these organs, the body recovers over time. For example, the liver is supported with drugs based on essential phospholipids.
- The disease is of moderate severity . The patient “goes through” 2 phases of disease development. It all starts close to the flu, then pneumonia develops, which usually develops in the alveoral space (directly in the alveoli there is an exchange between air and blood). Hypoxia with moderate severity of COVID-19 is not uncommon, especially if a large area of the lungs is affected, but patients usually do not require mechanical ventilation. It is possible to increase the oxygen level by supplying oxygen into the nose using a cannula, through breathing exercises, and prone position (lying on the stomach).
- Severe form of COVID-19 . Affects all phases of disease development. At the first stage there is a pronounced fever. Possible loss of consciousness. Acute respiratory distress syndrome and extensive pneumonia develop rapidly. Moreover, not only in the alveoral space, but also in the interstitial space, i.e. between partitions. In this case, pulmonary edema increases very quickly. CT scan shows a ground glass pattern. Blood clots may form in the arteries. Also, it is with pneumonia in the interstitial space that a person is more often oxygen-dependent: the natural oxygen level is low, oxygen deficiency occurs. Such patients often require mechanical ventilation, very high doses of drugs that reduce blood clotting activity.
What is fainting and should you be afraid of it?
In works of art you can often see a scene of young, languid, unmarried young ladies of noble origin fainting from shocking news. Loss of consciousness was a certain obligatory attribute of refined natures in the highest aristocratic society. But in fact, anyone can experience fainting, regardless of gender and age. Let's figure out what causes fainting, when it can be dangerous and whether it is really possible to lose consciousness from sudden news.
Fainting
- a short-term loss of consciousness and muscle control caused by low blood flow to the brain. In most cases, this condition is not dangerous, but sometimes fainting can be a symptom of the disease.
There are several types of fainting, which are divided depending on the cause of the condition. Let's list some types (don't be alarmed, there will be complex terms later).
Neurally mediated syncope. It is also called neurocardiogenic, vasovagal, or vasodepressor syncope. This is the most common type of fainting. It is more common in children and young adults, although it can occur at any age.
Vasovagal syncope is caused by stimulating the vagus nerve, which can briefly reduce heart rate and blood pressure, which causes a drop in blood flow to the brain, causing the person to lose consciousness. This type of fainting can occur when you strain during a bowel movement or when you experience sudden, intense stress. Yes, that same shocking news may well trigger it.
Telemedicine
Online consultation with doctors. Faster than a trip to the clinic Cheaper than an in-person appointment
- Situational syncope is a type of vasovagal syncope. It is associated with certain situations that affect the nervous system. For example, such fainting can be caused by:
- dehydration;
- severe emotional stress, anxiety, fear;
- pain;
- hunger;
- alcohol or drug use;
- hyperventilation (inhaling too much oxygen and quickly expelling too much carbon dioxide);
- severe coughing, sneezing or laughing;
- urination.
- The cause of fainting may be postural hypotension, that is, a sharp decrease in pressure that provokes fainting. This can happen when you quickly change position, for example from lying down to standing. Certain medications and dehydration can lead to this condition.
- Cardiac or cardiovascular syncope is associated with cardiovascular disease and may be a symptom of it. Such fainting may be associated with conditions such as bradycardia (severely slow heart rate), tachycardia (severely increased heart rate), or certain types of hypotension (low blood pressure).
- Unknown reason. In some cases, the cause of fainting may remain unclear.
We'll help you choose the program that's right for you
Fainting may be preceded by the following conditions:
- dizziness;
- nausea;
- darkening of the eyes;
- feeling of warmth;
- feeling drowsy or weak.
If you feel like you're about to faint, you can try:
- lie on your back and raise your legs. If this cannot be done, then sit down and lower your head between your knees;
- drink some water;
- eat something;
- take a few deep breaths.
If someone nearby has fainted, it is important to remain calm and not give in to panic. Place the person on their back and elevate their legs if possible. Usually a person regains consciousness after about 20 seconds.
Call an ambulance if:
- it is impossible to wake a person 1 minute after losing consciousness;
- he was seriously injured in the fall;
- the person shakes or twitches due to a seizure.
When loss of consciousness is not a problem
Vasovagal syncope (including situational syncope) is usually not a sign of any problem. Such fainting can occur due to prolonged standing, dehydration, the sight of blood, emotional trauma, stress, or fear of bodily harm.
If such fainting occurs quite often and causes concern, seek advice from a specialist.
A serious cause of loss of consciousness may be indicated by:
- age over 60 years;
- presence of known cardiovascular diseases;
- fainting during or after physical activity;
- fainting while lying on your back;
- atypical cardiac examination;
- family history of hereditary diseases;
- loss of consciousness as a side effect of medications.
In this case, you should consult a doctor as soon as possible. You can prepare for your visit to the clinic by answering the following questions:
- Do you feel nauseous or dizzy before passing out?
- Do you have shortness of breath?
- Have you taken a new medicine?
- Are you eating and sleeping well?
- How often have you fainted?
Examination in a hospital setting
More details
At the appointment, the doctor may ask other questions; this is necessary to collect a complete history so that the doctor can see the whole picture. Your doctor may also order additional tests to determine the cause of fainting:
- blood test to check for anemia or metabolic changes;
- electrocardiogram (ECG) - a test that records the electrical signals the heart produces. It can detect irregular heart rhythm and other heart problems. The test may be performed using a portable monitor that will have to be worn for a period of time;
- Exercise ECG is a test in which an ECG records the electrical activity of the heart while a person is physically active, such as running on a treadmill;
- echocardiogram - a test that uses high-frequency sound waves to create an image of the heart's structures;
- tilt table - the analysis is carried out on a special table that tilts at different angles, at which point blood pressure and heart rate are recorded. The test may show abnormal cardiovascular reflexes that cause fainting.
In what cases should you consult a doctor?
- If you have symptoms such as fever and dry cough, you should consult a doctor immediately.
- If the symptoms are atypical (for example, dermatological + loss of taste), but there is a suspicion that there has been contact with a carrier of the coronavirus, you should not delay visiting a doctor either.
- If you have difficulty breathing (severe shortness of breath), there is a feeling that there is no oxygen, you should immediately call an ambulance.
- The situation when a loss of smell occurred was not previously considered a reason to immediately go to the doctor, but in the current epidemic situation, with loss of smell (and especially at the same time with loss of taste), it is important to undergo laboratory diagnostics and exclude infection with coronavirus.
- If there are any manifestations of colds, a sore throat, or a runny nose, then in a pandemic, this is also a signal to see a doctor.
In a special risk group:
- Elderly people, the risk of complications is especially high in patients over 70 years of age.
- Persons with somatic diseases of the endocrine and cardiovascular systems: especially arterial hypertension, diabetes, atrial fibrillation.
- Taking hormonal medications.
- Persons with chronic respiratory diseases (COPD, asthma, pulmonary hypertension, idiopathic pulmonary hemosiderosis).
- Cancer patients.
- Persons with excess body weight and metabolic disorders.
Treatment
The main goal of treatment for bettolepsy is always aimed at treating the underlying disease that caused the development of cough syncope. An action plan is drawn up individually after all necessary examinations have been carried out.
During and after an attack of coughing syncope, symptomatic therapy is carried out, aimed at alleviating the patient’s condition. It may involve the use of the following means:
- ammonia;
- oxygen therapy;
- improving bronchial patency and antitussives;
- cardiotonic drugs;
- vasoconstrictors: Ephedrine, Mezaton;
- administration of Atropine sulfate (for bradycardia).
Cough fainting often frightens the patient and those around him. Their appearance should always be a reason to consult a doctor and conduct a comprehensive examination and treatment of the underlying disease that triggered the development of bettolepsy.
Be careful about your health and don’t put off visiting a specialist! Even a fall that accompanies loss of consciousness can cause serious injuries, and in some diseases, coughing fainting causes structural damage to brain tissue and irreversible complications. Remember this and be healthy!
How to influence COVID symptoms with breathing exercises?
Exercises that are aimed at optimizing air exchange in the alveoli of the lungs also help to reduce a number of symptoms (if the disease is not severe) or increase the speed of treatment in severe forms of the disease.
Exercises based on quick short breaths of air through the nose and passive exhalation give good results.
In addition to the fact that exercise saturates the body with oxygen, blood circulation improves and lymphatic drainage is put in order. Breathing exercises are also useful for combating inflammatory processes. The optimal option is about 30-40 breaths, 3-6 seconds of rest and cyclic repetition of the exercises 3-4 times. It is best to do exercises in a well-ventilated area on an empty stomach, or if you feel very weak, 1.5-2 hours after eating.
Hypertension is a contraindication for performing breathing exercises. Exercise can further raise your blood pressure.
Coronavirus prevention measures
- Wear masks, medical respirators, disposable gloves, and eye shields.
- Wash your hands regularly and treat them with antiseptics that contain 70% alcohol. Also treat handles, window sills, and tables with disinfectant solutions.
- Ventilate the room often.
- Maintain a sufficient level of humidity in the room (40-60%), use humidifiers if necessary.
- Rinse mucous membranes with saline solutions. They can be purchased at the pharmacy or prepared from table sea salt.
- Take vitamins, including vitamin D and B vitamins.
- Do breathing exercises and strengthen your lungs. They will not help avoid infection, but will help the body avoid severe disease.
Diagnostic criteria and research methods
Since it is possible for a bettolepsy seizure to smoothly flow into a petit mal seizure, the treating neurologist needs to know exactly what pathology he is dealing with.
Therefore, important diagnostic criteria are the onset of cough syncope:
- without warning signs;
- during a coughing attack - in the first minute;
- absence of biting the tongue and secretion of foamy saliva from the mouth, as well as subsequent falling asleep characteristic of epilepsy.
To establish a true diagnosis, the previous actions of the person suffering from attacks are important - in the form of eating, defecation, excessive laughter-gelolepsy, as well as the influence of cold air and tobacco smoke on him.
His age (mature or even older), as well as the presence of respiratory and vascular disorders, is important. In addition to performing the Valsalva maneuver, the effect of using instrumental methods for studying the state of the nervous system and the body as a whole should be noted:
- EEG;
- ECG, EchoCG and Holter monitoring;
- blood pressure monitoring;
- X-ray and other methods for detecting respiratory pathology.
If necessary, an inpatient examination is carried out, including in cases of difficulty, in an epileptology center.
conclusions
- The most common symptoms of coronavirus are fever, weakness (weakness), dry cough, loss of smell; in complicated and severe forms of COVID there are serious difficulties with breathing.
- Both adults and children can get sick, with or without severe symptoms. But there are more asymptomatic patients among children than among adults.
- Much depends on how the virus entered the body. If through the eyes, inflammation of the eyeball is pronounced. If the virus is transmitted by airborne droplets, the first symptoms include a sore throat and cough.
- A number of patients have dermatological signs in addition to the characteristic respiratory signs.
- Loss of smell is a common, but not essential, symptom of coronavirus. At the same time, it is also not worth considering the loss of charm as the presence of coronavirus. Often this is a signal of other pathologies.
- To reduce symptoms, it is important to start timely treatment, monitor nutrition, and do breathing exercises.
- At increased risk are the elderly, people with impaired metabolism, blood clotting problems, and a weakened immune system. The course of the disease in them is more difficult, and the symptoms are more pronounced.
- If coromavirus is in a mild form, then there is no difficulty breathing, but if it is severe, this is one of the common difficulties in treating the disease.
- The most complex symptoms are in patients with respiratory distress syndrome. With it, the attack begins on healthy tissues of the body.
Follow sanitary and hygienic rules; if symptoms appear, consult a doctor immediately, do not panic.
Symptoms and clinic
A typical picture that precedes coughing fainting is purple discoloration of the skin of the face and visible parts of the upper half of the victim’s body at the peak of a coughing attack, with swelling of the veins overflowing with stagnant blood due to strain, followed by cyanosis.
Then fainting occurs - the body, without any “preliminary explanation,” falls to the floor.
The further fate of a person depends on the duration of fainting. But in any case, the victim’s skin turns pale, and in an unconscious state, suffocation stops along with coughing.
Depending on the depth of cerebral hypoxia that has developed, the following may occur:
- rapid return to consciousness (with the duration of fainting from seconds to a minute);
- the return to consciousness is longer, with the development of short-term tonic convulsions in the form of twitching of the limbs and a drop in the tone of the pelvic organs with incontinence of feces and urine.
It is possible to have epileptiform convulsions in one of the areas of the body, as well as short-term “twilight” of consciousness during coughing suffocation without falling to the ground (on the floor), while maintaining the original position of the body.
The consequences of cough syncope depend on the severity of the somatic pathology predisposing to the development of bettolepsy - with deep-seated changes, damage to thin brain structures that are especially sensitive to hypoxia and fluctuations in the level of blood pressure and cerebrospinal fluid in the corresponding systems is possible.