The perinatal period is the period from the 28th week of pregnancy to the 7th day after birth, inclusive. If during this period, as a result of exposure to various unfavorable factors, damage to the child’s brain occurs, accompanied by neurological symptoms, then such damage is called perinatal damage to the central nervous system or perinatal encephalopathy.
The concept of perinatal damage to the central nervous system combines several pathologies resulting from damage to brain cells in the perinatal period and leading to dysfunction. Damage to the central nervous system in the perinatal period can lead to the development of serious diseases later (cerebral palsy, delayed psychomotor and psycho-speech development, etc.).
Perinatal encephalopathy manifests itself as various disorders in motor development, impaired speech formation, and mental disorders.
Perinatal encephalopathy is a syndromic diagnosis and requires mandatory clarification. That is, it is necessary to examine the child in order to find out which specific departments are damaged and to what extent, and what functions this damage affects. A detailed examination will allow the doctor to prescribe adequate treatment and minimize the consequences of the damage.
Risk factors
The development of perinatal encephalopathy in the fetus and child can lead to
- chronic maternal intoxication and chronic diseases
- infectious diseases during pregnancy
- disorders of uteroplacental blood flow, placental abruption, fetoplacental insufficiency
- Umbilical cord entanglement
- maternal diseases associated with metabolic disorders (diabetes mellitus, phenylketonuria, etc.)
- severe toxicosis;
- pathological course of labor, use of obstetric aid, weakness of labor, rapid labor
- prematurity;
- Fetal malformations
What is PPCNS?
The very phrase perinatal period suggests that perinatal damage to the central nervous system develops in an unborn or newly born child. Perinatal damage to the central nervous system (PPCNS) is not one, but several diagnoses that imply dysfunction in the brain of a newborn child and can lead to persistent neurological consequences at an older age (for example, cerebral palsy, cerebral palsy).
The entire perinatal period is divided into three stages:
– from the 28th week until the moment of birth, the antenatal period ;
– the process of childbirth itself is called the intrapartum period ;
– the neonatal period is the period of time from the moment of birth to the 7th day of life inclusive.
In modern medicine there is no exact name for the disease when the central nervous system of the fetus is affected, there is only a collective one, it is called PPCNS or perinatal encephalopathy . Perinatal damage to the central nervous system in newborns is manifested by disturbances in the functioning of the musculoskeletal system, speech and mental disorders.
With the development of medicine, this diagnosis has ceased to be used for children older than one month. After a month, the doctor must make an accurate diagnosis of the child. It is during this period that the neurologist accurately determines how badly the nervous system is damaged. Prescribes treatment and ensures that it is chosen correctly.
What are the causes and risk factors for PPCNSL?
The reasons why perinatal damage to the central nervous system may develop are quite varied, among the most popular:
– somatic disease of the mother, which is accompanied by chronic intoxication;
– the presence of acute infectious diseases or chronic foci of infection while the expectant mother was carrying the child;
– if a woman’s nutritional process is disrupted, or she is not ripe for pregnancy and childbirth;
– disruption of uteroplacental blood flow during pregnancy;
– changes in metabolism also entail a disorder of the nervous system in the unborn child (increased bilirubin levels, neonatal jaundice);
– in case of severe toxicosis, both at an early stage and at a late stage, or the appearance of other problems with bearing a child;
– the environment is an important factor in the development of the disease;
– the appearance of pathology during childbirth - this may be weak labor, accelerated labor;
– if a child is born prematurely, then his body is not fully developed, therefore, against this background, a disturbance in the functioning of the central nervous system may appear;
– Children who have a hereditary factor are at greatest risk of developing central nervous system lesions.
All other causes of PPCNS are situational and, to a greater extent, their occurrence is simply impossible to predict. There are several ways of development of perinatal damage to the central nervous system in newborns, depending on the cause and subsequent symptoms, the analysis of which allows us to make an initial diagnosis:
– If a lack of oxygen is clearly detected while the baby is inside the mother’s body (hypoxia), then hypoxic damage to the central nervous system is diagnosed.
– During childbirth, the baby’s tissue structure may be damaged (this can be either the brain or the spinal cord). In this case, we are already talking about a traumatic lesion of the central nervous system, resulting in changes in the functioning of the brain.
– In case of metabolic disorders, metabolic and toxic-metabolic lesions may appear. This may be due to the use of alcohol, medications, or nicotine during pregnancy.
– Changes in the central nervous system in the presence of infectious diseases of the perinatal period.
Symptoms, how PCNSL manifests itself
Perinatal encephalopathy is a very multifaceted disease. The following main clinical syndromes of PPCNSL are distinguished:
- Muscular dystonia is a pathological increase or decrease in muscle tone. Normally, all newborns have increased muscle tone of the flexors; in the process of growth and motor development, the flexor tone decreases, becoming normal. This transformation allows a newborn child to have the necessary set of protective reflexes, and during the process of growth, a decrease in flexor tone makes it possible to develop movements. In cases where muscle tone has not decreased in a timely manner or does not change symmetrically, this significantly interferes with the normal development of the child’s motor sphere, the formation of postural control and normal movements.
- Neuro-reflex excitability syndrome is a disorder of sleep and wakefulness, an overly active reaction to sounds and touches.
- CNS depression. Lethargy, apathy, decreased tone and reflexes, drowsiness.
- Intracranial hypertension. This syndrome occurs when intracranial pressure increases. Increased excitability, obsessive screaming, regurgitation, bulging fontanel and Graefe's symptom are most characteristic of this syndrome. Intracranial hypertension can lead to the development of hydrocephalus—a decrease in the volume of brain tissue and its replacement with fluid.
- Convulsions (convulsive syndrome) are involuntary contractions of the muscles of the entire body, accompanied by loss of consciousness or simply “freezing” for several seconds. Convulsive syndrome is dangerous because, if left untreated, it significantly disrupts the normal development of the brain and its function.
Outcomes and consequences of CNS PP
The consequences of PP CNS can be determined by 1 year of life. Below are their main manifestations:
- Impaired motor development: delay in acquiring the skills of holding the head, rolling over, sitting, crawling, standing up, and walking independently relative to the physical age of the child.
- The formation of paresis and paralysis of both one and several limbs (monoplegia, diplegia, hemiparesis, tetraparesis), which belong to various forms of cerebral palsy.
- Violation of psycho-speech development: delay in acquiring the skill of humming, babbling, the first words and phrases, the quality of pronounced sounds, the timing of the formation of pincer grip and pointing gestures, understanding of addressed speech, interest in surrounding objects and using them for their intended purpose, the nature of the game, memorizing new information , concentration of attention with the formation of attention deficit hyperactivity disorder.
- Disorders of behavior and emotions: timing of the formation of the revitalization complex, differentiation of relatives and strangers, emotional resonance, degree of expression of emotions, communication with peers and adults, the possibility of playing together, the formation of neatness skills, possibly leading to autism spectrum disorders.
- Hydrocephalus: excessive increase in head circumference, head deformation, pronounced saphenous veins in the temporal areas, signs of hypertension and hydrocephalic syndromes.
- Paroxysmal conditions of non-epileptic origin: affective-respiratory seizures, benign myoclonus of infancy (Fijerman's syndrome), benign neonatal sleep myoclonus, Sandiffer's syndrome, infantile torticollis, restless sleep, night terrors, rhythmic movements in sleep (rocking, head shaking, thumb sucking, grinding teeth).
- Age-dependent epileptic syndromes: early infantile epileptic encephalopathy (Ohtahara syndrome), early myoclonic encephalopathy, Dravet syndrome, West syndrome, benign neonatal epileptic syndromes, benign myoclonic epilepsy of infancy, benign partial epilepsy of infancy.
Treatment and rehabilitation for PCNSL
Treatment of PPCNS begins with measures to prevent it.
Before birth, mandatory monitoring of the fetal condition is carried out and, if any abnormalities are present, treatment is immediately prescribed. In severe cases, surgical delivery may be required.
During the perinatal period, children with suspected PPCNS are observed by a neonatologist. At this stage, intensive therapy is carried out, the child is in a specialized department.
After stabilization of the condition, in the absence of a threat to life, the recovery process begins - rehabilitation. The goal of this stage is to minimize the effects of brain damage.
At this stage, medications are used that improve trophic processes in brain tissue, massage to normalize tone and stimulate tactile and proprioceptors, exercise therapy and kinesiotherapy (Bobat, Vojta, etc.) to develop motor skills and prevent the development of contractures, it may also be necessary the use of special orthopedic devices to prevent or correct limb deformities. Botulinum therapy can be used to reduce tone.
The most important thing is to remember that all rehabilitation activities are carried out for one purpose - to provide an opportunity for the child to develop skills and make him as independent as possible in adulthood. Each child’s body is unique and the result of recovery in each specific case is very difficult to predict, however, the correct and consistent use of rehabilitation methods and techniques allows you to achieve maximum results. Cases of partial or complete restoration of central nervous system functions after PCNSL are far from uncommon.
Causes
As you know, no disease occurs on its own; the development of pathology of the nervous system in the fetus in the womb or in a newly born baby is associated with reasons such as:
- viral infection (syphilis, herpes);
- oxygen starvation;
- negligent attitude of obstetricians towards a woman in labor and her child during childbirth;
- the influence of toxic substances on the body of a pregnant woman (alcohol, tobacco, drugs, fumes of gases of natural and chemical origin);
- genetic predisposition.
A child diagnosed with depression syndrome should be taken to see a speech therapist or psychologist from time to time, provided with proper and balanced nutrition, and also create an environment that is as comfortable as possible for the child (it is recommended to exclude the influence of loud sounds and, if possible, refuse to visit guests).
Our rehabilitation programs for PCNSL
We provide comprehensive treatment for the consequences of perinatal CNS damage.
Typically, a rehabilitation program includes:
- Observation by a neurologist. The participation of this doctor is necessary, since the child’s condition must be monitored during the process of rehabilitation measures
- Observation by a physical therapy doctor (rehabilitation specialist). The basis of any rehabilitation is the development and restoration of motor skills. A physical therapy doctor will examine a small patient and plan the rehabilitation process, helping to prioritize physical treatment.
- Observation by a neuropsychologist and sessions with a neuropsychologist. The participation of a neuropsychologist in rehabilitation after PCNSL is necessary starting from 2 years of age. The tasks of a neuropsychologist include diagnosing disorders of higher nervous activity in a child, planning and implementing measures to correct them. Neuropsychologists conduct group and developmental classes with children to develop memory, attention, motivation, and thinking. The neuropsychologist also provides family counseling.
- Exercise therapy and kinesitherapy. We are proficient in various exercise therapy techniques. It is impractical to single out just one among them. Exercise therapy techniques are tools in the hands of a doctor and instructor. We try to select the appropriate instrument for each of our patients. The most commonly used methods in children are Bobath therapy and Vojta therapy. We also use PNF, Neurac, manual therapy techniques and many others in our work.
- Massage. Massage plays an important role in the rehabilitation of children. Naturally, it is not an independent procedure, but its reasonable use allows the child to become more aware of his body and helps him learn to control it. In addition, massage in rehabilitation solves many auxiliary problems - eliminating swelling, improving muscle nutrition, temporary decrease in tone, etc.
- Physiotherapy. We widely use physiotherapeutic treatment in rehabilitation after PCNSL. The objectives of physiotherapy are very diverse and depend on the characteristics of the disease. The most commonly used are medicinal electrophoresis, IR dipole, phototherapy, and magnetic therapy.
- If necessary, a speech therapist may be included in the rehabilitation team. Typically, the need to involve this specialist arises when there is a delay in speech development or alalia.
If you have any questions or want to sign up for a rehabilitation program, call us at: +7 (812) 309-67-26 or leave a request through the contact form on the website.
Oncology and damage to the nervous system
Many malignant tumors contribute to the formation in the body of a large number of toxins and immune factors that are aggressive to the body’s own tissues, incl. to the brain and spinal cord, to peripheral nerves, muscles. Paraneoplastic disease of the nervous system is damage to the nervous system not by a tumor, but by the immune system under the influence of a tumor. We have specialists and modern laboratory tests to diagnose paraneoplastic diseases of the nervous system and experience in their treatment.
Read more about laboratory tests for suspected paraneoplastic diseases of the nervous system.
Intoxication and autoimmune aggression can cause paraneoplastic syndromes and damage:
- muscles,
- peripheral nerves,
- brain and spinal cord.
Symptoms of paraneoplastic processes can be very diverse:
- paralysis and paresis,
- sensitivity disorders,
- hearing and vision impairments,
- imbalance,
- mental disorders.
What tissues of the nervous system can be affected by paraneoplastic syndromes?
- Peripheral nerves – polyneuropathy and polyneuritis.
- Muscles – myopathy and polymyositis.
- Brain – encephalopathy, encephalitis.
- Spinal cord – myelopathy.
Discirculatory encephalopathy, circulatory disorders
The human nervous system consumes a huge amount of energy and is therefore very dependent on nutrition. The delivery of oxygen, glucose and other necessary substances is provided by arterial blood. Metabolic products to be disposed of are evacuated with venous blood . With a lack of blood supply, the brain matter either gradually atrophies (encephalopathy) or dies within a few hours (stroke).
Poor cerebral circulation can be associated with narrowing and blockage of blood vessels for various reasons:
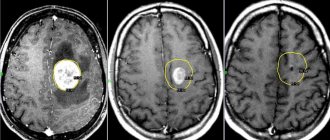
- Vasculitis (inflammation of blood vessels due to immune attack or infection). This rather dangerous disease usually leads to gradual, small-focal death of brain matter. With MRI, vasculitis is often confused with various types of encephalopathies and multiple sclerosis. More details here
- Atherosclerosis is the deposition of fat (cholesterol) between the layers of the inner walls of blood vessels. Deposition occurs in the form of plaques. Plaques bulge into the arteries and obstruct blood flow, causing chronic circulatory deficiency, with gradual atrophy of the medulla. The greatest danger is posed by ruptured plaques, fatty masses from which enter the blood and clog smaller arteries (stroke, acute cerebrovascular accident, cerebral infarction).
- An increase in blood coagulability and viscosity prevents blood from flowing through the smallest blood vessels (capillaries) and causes a chronic lack of blood supply to the brain. In addition, intravascular coagulation with blockage of the vessel is possible (stroke, acute cerebrovascular accident, cerebral infarction).
- Compression or tortuosity of a blood vessel. The arteries passing through the cervical vertebrae (vertebral arteries) are usually affected, causing dizziness, loss of balance, and visual and hearing disturbances.
Treatment of cerebrovascular accidents in our clinic begins with accurate detection of its cause. This is how we select a treatment method that is truly effective in this particular case. For diagnostics we use:
- Blood test for fats, vasculitis markers and coagulation;
- Doppler ultrasound and/or MR angiography to clarify the location of the narrowing of the blood vessel;
- X-ray, CT or MR tomography to look for deformations of the cervical vertebrae that are dangerous for blood vessels.