Causes of cortical dysarthria in children
The defect develops as a result of damage to those areas of the cerebral cortex that regulate the tone and contractions of the muscles of the cheek, pharynx, jaw, soft palate, lips and tongue.
The cause of the disorder may be:
- perinatal pathology is the main cause of brain damage in childhood. Hypoxia, intrauterine infection, and asphyxia of the newborn are important. The likelihood of these conditions is increased by a complicated obstetric history, oligohydramnios, gestosis, and rapid labor;
- traumatic brain injuries - in children, birth injuries play an important role, which occur due to inadequately chosen labor management tactics. Injuries at an early age are dangerous due to falls and impacts. Brain damage in older children and adolescents can also cause speech disorders;
- space-occupying formations lead to compression of the cerebral cortex, sometimes to germination and destruction, that is, destruction;
- neuroinfections - consequences of ARVI, rubella, herpes, measles, sinusitis, sinusitis, otitis, abscess, syphilis, tuberculosis.
The mechanism of development of the cortical form of dysarthria is associated with damage to the anterior central gyrus or the area behind it. In the first case, central paresis of the articulatory muscles develops. In the second, the processing of information about the state of the organs of articulation is disrupted, which is why there is no correction of the movements of the muscles involved in speech. This is how apraxia occurs - a failure in the sequence of muscle contractions.
Analysis of electroencephalogram features in children with attention disorder and hyperactivity disorder
M.I. Lokhov, Yu.A. Fesenko, L.P. Rubina, Research Institute of Experimental Medicine of the Russian Academy of Medical Sciences, Center for Rehabilitation Treatment “Child Psychiatry”, St. Petersburg.
The basis for the formation of attention deficit hyperactivity disorder (ADHD) is minimal brain dysfunction (MBD). The concept of MDM arose in neurological pediatric practice to characterize perinatal brain lesions that do not lead to significant impairments in motor skills and intelligence, but cause clear neurological and psychopathological disorders [1, 2]. Most researchers include the most common neurological symptoms in MDM as a violation of associative movements, twitching of various muscle groups, tremor of the fingers, disorders of tendon reflexes and coordination of movements, and psychopathological disorders include impaired attention, hyperactivity, emotional lability, increased fatigue, impaired perception and formation of concepts. Due to the fact that “attention disturbance with hyperactivity” occurs in 80-93% of MDM, they were identified as a separate syndrome, replacing (although not entirely fairly) the concept of MDM at present.
Over the past decades, in pediatric neurological practice there has been an increase in the number of children with ADHD. In St. Petersburg, according to epidemiological surveys, ADHD is found in 17.5% of children aged 4 to 11 years [3]. The 1994 American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) divides this syndrome into 3 types: predominant inattention, predominant hyperactivity-impulsivity, and mixed.
From a neurophysiological point of view, it has been suggested that the etiology of ADHD is based on a disruption in the interaction of the caudate nucleus and the frontal cortex, apparently caused by an imbalance of dopamine and norepinephrine [4]. To compensate for this imbalance, the body is forced to resort to a kind of stimulation of the cerebral cortex through the motor centers, which leads to hyperactivity syndrome. Thus, increased motor activity serves as a kind of protective mechanism that supports a certain functional interaction between the brain structures responsible for its normal development.
The use of computer cross-correlation analysis of the electroencephalogram (EEG) in ADHD provides fundamentally new opportunities for determining the interaction of the structures of the cerebral cortex, which can occur not only directly between the cortical areas themselves, but also through subcortical formations. Calculation of the cross-correlation function allows us to reveal the mechanisms and ways of forming functional connections between the activity of different parts of the brain.
The degree of similarity or connection between two EEGs in cross-correlation analysis is determined by the value of the cross-correlation coefficient (Ccr), which can range from +1 to -1. If two EEGs are exact copies, then the Ccr of these EEGs will be equal to the maximum value, i.e. +1. In cases where the two processes under study contain, in addition to common components, other elements characteristic of each of them separately, the magnitude of the connection, determined by Ccr, will have a value less than unity, and the less, the more independent elements or frequencies there are in two studied EEG.
When analyzing cross-correlation, the following quantities are usually quantified:
- The degree of correlation based on the value of Ccr—the ratio of the maximum value of the cross-correlation function to the maximum value of the autocorrelation function of each of the processes under study at t=0 (taken as 1).
- The time shift of the maximum of the cross-correlation function - BC or t, characterizing the time relationships of two processes.
In this case, by the value of Ccr one can judge the degree of correlation between the two processes: with a Ccr value of up to 0.2, the connection is very weak; from 0.2 to 0.5 - moderate; from 0.5 and above - significant; from 0.7 to 0.9 - tight or high.
At t=0, the process is characterized by in-phase oscillations in two EEG leads. When comparing leads 1 and 2, t with a + sign characterizes the advance of the process in lead 1 compared to lead 2, and t with a minus sign characterizes the advance in lead 2 compared to lead 1.
In our long-term studies of cross-correlation activity in the EEG in children under normal conditions and with the development of borderline disorders [5-7], we used monopolar recording with an averaged ear electrode on a computer encephalographic console “Telepath” with recording on a computer hard drive and subsequent processing using special analysis programs, developed at LETI named after. A. S. Popova. To present the results obtained in a visual form, the well-known graph projection method was used [8], reflecting the dynamics of movement of the foci of maximum activity and associated inhibition of various areas of the left and right hemispheres of the brain. In the language of graph theory, such areas are designated as source and drain points, respectively. We studied the presence of sources and drainages in the parieto-occipital or inferior parietal zone (cytoarchitectonic areas 39 and 40, according to Brodmann) of the right hemisphere of the brain. This area of the cerebral cortex, according to many studies [9–11], plays a leading role in the development of the child’s psyche and intelligence, and is also of no small importance in many mental disorders in adulthood [12, 13]. Suffice it to say that the characteristic profiles of psychotropic pharmacological drugs are built specifically in relation to the right parieto-occipital region of the cerebral cortex [14].
In our practice, out of 658 children, in most cases (70%) it was the mixed type of ADHD, often (in 30-40%) complicated by other borderline mental disorders of childhood (tics, stuttering, enuresis) [5, 6].
Rice. 1. Average data of cross-correlation analysis of EEG of healthy children tested 3-11 years old. Thin arrows in the graphs indicate cross-correlations between 0.3 and 0.5, and thicker ones above 0.5. The direction of the arrows characterizes the advance in the work of the structure from which the arrow comes (the so-called source).
Rice. 2. Average data from cross-correlation analysis of EEG of children aged 3–11 years suffering from severe forms of stuttering (explanations in the text).
Rice. 3, a. Fragment of computer cross-correlation analysis of background EEG recording of patient O., 6 years old, with ADHD.
Rice. 3, b. A fragment of a computer EEG of the same patient against the background of hyperventilation. Preliminary diagnosis: stuttering, ADHD.
Rice. 3, c. Fragment of computer cross-correlation analysis of EEG against the background of hyperventilation in the same patient.
The following research results show the dynamics of changes in the nature of cross-correlation activity characterizing the relationship between different areas of the cerebral cortex in normal conditions and with ADHD in children 3-11 years old, with a strictly selected periodicity and epoch of analysis (8 s) of the background EEG recording and during hyperventilation . Hyperventilation was carried out for 3 minutes, with a maximum depth of inhalation and exhalation, and a frequency of 20 respiratory movements per minute.
As can be seen from the presented data (Fig. 1), averaged over more than 200 healthy subjects (children 3-11 years old), the right parieto-occipital region is normal (3-minute background recording), starting from 3-4 years of age, was the area of origins, which is confirmed by the results of other studies [9-11]. As a rule, the frequency range 4–12 Hz was used in the analysis. With the dynamics of cross-correlations in the case of a sequential analysis of the background EEG recording in one healthy child, it turned out that the relationships between the structures were not homogeneous. They seem to “breathe” and compete with each other for leadership in the average recording. In some cases, it was discovered that EEG segments changed their relationships with each other to those directly opposite to those that were revealed by statistical averaging of the recording as a whole. Such a dynamic pattern of cross-correlations was typical for most children aged 3-11 years. It is also worth noting that normally most connections had a correlation coefficient above 0.5.
A completely different picture was observed when analyzing the EEG in sick children of the same age with borderline mental disorders, in particular with ADHD (Fig. 2).
In Fig. 3a shows the results of a computer EEG of patient O., 6 years old, with ADHD and stuttering. The results of processing a background recording, i.e., an EEG recording in a state of quiet wakefulness with eyes closed, are presented. The background recording differed from that characteristic of the norm only in the direction of interaction between brain structures that was changed in some fragments. However, during hyperventilation - increased respiratory activity, which under normal conditions is equivalent to increased breathing during vigorous motor activity of a child - there was a noticeable change in this relationship. In response to hyperventilation in the EEG after the first minute, generalized bursts of q-rhythmic activity appeared in the frequency range of 4 Hz (Fig. 3, b), which was accompanied by a temporary restoration of full cross-correlation connections of the parietal-occipital zone of the right hemisphere with other areas of the brain (Fig. 3, b). 3, c).
Thus, it can be assumed that hyperactivity is a kind of protective mechanism that temporarily restores normal connections in the cerebral cortex and thereby preserves the normal intellectual development of the child.
Our study found that the observed changes are not typical for other monosymptomatic borderline disorders of childhood.
So, the EEG in children with ADHD has a number of features that distinguish it from that characteristic of the norm or children with other monosymptomatic borderline mental disorders.
Firstly, although in terms of external manifestations in most cases the background EEG recording in children with ADHD differs slightly from the age norm (the presence of dominant a-activity, its distribution, the absence of clearly defined pathological signs, etc.), according to the results of cross-correlation analysis in in the range of the leading recorded rhythms (4-12 Hz), a clearly defined deviation from the norm is observed, consisting in the almost complete absence of connections between the frontal and other structures of the brain.
Secondly, during hyperventilation (under standard conditions), slow-wave activity (3-5 Hz) in children with ADHD appears in most cases already in the first minute and is of a generalized cyclic nature (cycle duration is 10-15 s) throughout the entire test with a slight aftereffect (20-30 s) after its completion.
Thirdly, during the occurrence of slow-wave activity, connections are restored (according to the results of cross-correlation analysis) between the frontal and other structures of the brain, which is not observed under similar conditions in patients with other monosymptomatic borderline mental disorders.
The data obtained suggest weaker control by the reticular formation of the brainstem over nonspecific thalamic structures and the leading role of these structures in synchronizing the interaction between various brain formations involved in memory processes and ensuring the intellectual safety of the patient with ADHD.
Literature:
- (Trjesoglava Z.) Trjesoglava Z. Mild brain dysfunction in childhood. M.: Medicine, 1986.
- Yaremenko B. R., Yaremenko A. B., Goryainova T. B. Minimal brain dysfunction in children. SPb.: SALIT-DEAN, 1999.
- Modern aspects of diagnosis and treatment of attention disorder with hyperactivity disorder in children. Ed. T. A. Lazebnik, L. S. Chutko, Yu. D. Kropotova and others.
- (Lubar JF) Lubar J. F. Biofeedback, attention deficit and hyperactivity. Biofeedback-3. Theory and practice. Novosibirsk, 1998; 142-62.
- Lokhov M.I., Fesenko Yu.A. Stuttering and logoneurosis. Diagnosis and treatment. SPb.: SOTIS, 2000.
- Lokhov M.I., Fesenko Yu.A., Rubin M.Yu. Bad good child. St. Petersburg: ELBI-SPb, 2003.
- Lokhov M.I. Psychophysiological mechanisms of speech correction in stuttering. St. Petersburg: Nauka, 1994.
- Pavlova L. P., Romanenko A. F. Systematic approach to the psychophysiological study of the human brain. L.: Nauka, 1988.
- Khrizman T. P. Development of child brain functions. L.: Nauka, 1978.
- Shepovalnikov A. N. Activity of the sleeping brain. L.: Nauka, 1971.
- Shepovalnikov A. N. et al. Functional asymmetry of the brain in disorders of speech and auditory development. M.: Nauka, 1992.
- Aleksandrovsky Yu. A. Borderline mental disorders. M.: Medicine, 2000.
- Flor-Henry P. Cerebral basis of psychopathology. Wright, Boston etc., 1983.
- Itil TM The significance of quantitative pharmacy EEG in discovery and classification of psychotropic drugs. EEG Drug Res. NY, 1982; 131—50
Journal “Review of Psychiatry and Medical Psychology named after. V.M. Bekhterev", t. 02, N2, 2005
Classification of cortical dysarthria in children
Depending on the location of the pathological focus and the mechanism of development, two types of pathology are distinguished:
- Cortical kinetic dysarthria (efferent) is associated with damage to the central zone of the anterior cortex. Due to the proximity of the area that controls hand movements, hemiparesis may occur. Characterized by slowness of speech and lack of rhythm. Some children speak in syllables;
- Kinesthetic (afferent) dysarthria is associated with damage to the postcentral zones. It is characterized by discoordinated work of the organs of articulation and movements of the muscles of the hand on the opposite side.
Based on severity, there are 4 forms of the defect. In the first degree there is no clear clinical picture, then their severity increases. Grade 4 may be accompanied by complete anarthria, that is, lack of speech.
Mixed variants of the disease are possible, for example, cortical-subcortical dysarthria, when in addition to the cortical part, the subcortical parts of the brain are also affected.
What is the research?
To conduct an EEG of the brain in children, use a room that, if possible, does not allow light and sound to pass through. Before the examination, a special cap with sensors is put on the patient’s head, which transmit signals to a device (electroencelograph).
The session duration ranges from 30 minutes as part of a routine examination to multi-day video-EEG monitoring as part of the presurgical diagnosis of epilepsy. The examination of children from one year onwards takes place in several stages:
- Taking an encephalogram at rest. In this case, the child should be in a sitting or lying position.
- Carrying out the test with eyes open and closed. This is done to determine the basic rhythm.
- In the future, the examination technique will differ depending on the purpose of the study.
- The hyperventilation test involves deep exhalations and inhalations in order to provoke pathological brain activity.
- During a photostimulation test, the light bulb flashes at certain intervals. The child at this moment is with his eyes closed.
- Additionally, sound stimulation, clenching and unclenching of fists, and a psychological assessment can be performed.
- An EEG of sleep (daytime, nighttime) is also recorded.
The next step is to decipher the results in order to identify deviations from the norm and determine pathological processes.
Symptoms of cortical dysarthria in children
Characteristic symptoms of cortical dysarthria are disturbances in the tempo-rhythmic component of speech: there is a slow pace of expressive speech, lack of fluency and automatism. From the outside it seems that it is difficult for the child to move his tongue and lips.
The most difficult sounds are the anterior lingual sounds. The baby replaces or skips problematic sounds. Because of this, speech is blurred and slurred. But there are no problems with the semantic part, that is, the vocabulary is sufficient, children correctly use words in sentences and correctly express their thoughts.
Cortical-subcortical dysarthria is characterized by violent involuntary movements at rest and during conversation.
Afferent cortical dysarthria
Signs of this variant of cortical dysarthria are the search for the correct articulatory structure when pronouncing sounds, which causes pauses. The voice, due to stress during conversation, is loud with a decrease in voiced consonants. Due to the slowness of speech, intercalary sounds appear.
The baby pronounces affricates (consonants made of two sounds) separately or pronounces only a separate part. For example, “t” or “s” or the prolonged “ts” from instead of the sound “ts”. It also replaces some sounds with others: fricative consonants with stop consonants. The child cannot name the place on the face that the speech therapist touches.
Efferent cortical dysarthria
Cortical kinetic dysarthria is characterized by slowness of speech due to problematic transitions between sounds. Stressed vowels are lengthened, and consonants, if they are at the beginning and end of a word, too. The pronunciation of “l”, “sh”, “r”, “zh” suffers: this requires the participation of the tongue, and the child’s tongue movements are difficult. He can replace them with “d” or “t”.
It is difficult for a child to fix the desired articulatory position, so there are unnecessary insertions and omissions of sounds. Children may wrinkle their forehead, stick out their tongue, close their eyes, and lick their lips when talking.
Complications in children
Speech defects affect the development of speech in general, the state of the nervous system and cognitive functions. Children do not develop their vocabulary well, and they have a general underdevelopment of speech. Attention and memory deteriorate. A pronunciation defect causes a deterioration in the perception of phonemes. Such violations are fraught with learning problems: written speech and reading suffer.
At older ages, the likelihood of psychological problems is high. School-age children have a hard time with speech disorders, become withdrawn, and may show aggression and irritability. Depression may develop. The situation becomes more complicated if there is a lack of understanding and help from parents.
Diagnosis of cortical dysarthria in children
The diagnosis is made based on an examination by a neurologist, speech therapist and the results of instrumental research methods:
- A neurological examination can reveal paresis of facial and articulatory muscles, facial asymmetry, and deviation of the tongue to one side. Difficulties in performing sequential actions at the request of a doctor are also identified;
- The speech therapist identifies not only the symptoms of cortical dysarthria, but also its characteristics and causes. Determines the degree of disturbance, the presence of its components: replacement of sounds, slowness and unevenness of speech;
- Hardware research methods make it possible to evaluate the structure of the brain and identify pathological foci: space-occupying formations, hematomas, consequences of traumatic brain injuries. Depending on the situation, an MRI or CT scan may be prescribed;
- Lumbar puncture is performed if a neuroinfection is suspected. This method allows you to evaluate the properties and amount of cerebrospinal fluid and identify the pathogen.
If necessary, the patient can be examined by other specialists. For example, in case of extensive education - an oncologist and neurosurgeon, in case of neuroinfection - an infectious disease specialist, a phthisiatrician.
Types of EEG changes
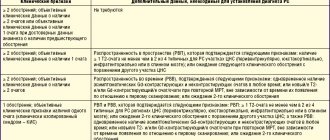
According to the severity of EEG changes over time, there are:
- Periodic (paroxysms)
- Continued
According to localization, EEG changes can be:1
- Focal (focal, local) – limited area (up to 3 leads);
- Regional – zone of the brain lobe (3 or more leads)
- Lateralized - pathological activity detected above the hemisphere;
- Generalized - general pathological activity, affecting the entire brain, recorded in all leads according to the mechanisms of primary and secondary generalization;
- Diffuse (unspecified) – cannot be classified into the above groups. Depending on the severity, diffuse EEG changes can be mild (moderate) or pronounced.
Specific EEG changes that are interrelated with various psychoneurological conditions are considered as EEG correlates.
Diffuse EEG changes
➥ Main article: Diffuse EEG changes
The term diffuse EEG changes reflects pathological processes that occur without a clearly localized focus and are “scattered” in nature, therefore they can be recorded throughout the brain, but quite often it is combined with generalized EEG changes, which are also observed in all areas of the brain.
Diffuse EEG changes may be normal, provided there are no other abnormalities. Thus, if in the conclusion it is written only about diffuse mild changes in the EEG, without paroxysms, foci of pathological activity, or without a decrease in the threshold of convulsive activity, then this is a variant of the norm.
Moderate and pronounced diffuse EEG changes are usually used to indicate the presence of pathology, but are nosologically nonspecific, i.e. These EEG patterns can be recorded both in patients with severe neurological diseases and with functional disorders of the nervous system. The information content of such conclusions is low. But at the same time, it was revealed that moderate and pronounced diffuse EEG changes in the midline structures are usually recorded in severe neurological patients.
If we are talking about focal (focal, local) changes in the EEG, then the presence of some space-occupying brain formations (cysts, tumors, etc.) is usually assumed.
Slowdown
➥ Main article: Diffuse slowing of bioelectrical activity
Fig.1. BEAGM deceleration formation scheme
A - the process causing the slowdown is localized in the cortex, B - the process is localized in the mid-stem structures), C - failure (damage) of the pacemaker zone
The slowdown in bioelectrical activity occurs due to a decrease in the functional activity of some nerve cells, which may be due to various etiological reasons, but pathogenetically represents the switching off of some “microswitches” (A). As a result, the main rhythm of the pacemaker zone spreads across the damaged area with minimal changes in the EEG, which is recorded as slow oscillations and rhythms.
Periodic diffuse slowing occurs in the initial stages of neurological diseases with a predominance of cerebral syndromes in the clinical picture, for example, encephalopathies of various origins, etc., when the functional activity of neurons can be restored after the load is stopped. Continued slowdown indicates a more severe defect, in which some of the nerve cells have completely changed their functional characteristics.
Diffuse slowing due to both a decrease in the overall frequency of the background rhythm and/or an increase in the index of slow-wave forms of activity is typical for patients of early childhood and older age groups, and does not indicate the development of any pathological process in such cases. Also, a slight diffuse slowing of the basic rhythm (up to 8 Hz) may be present in healthy young people, which can also be considered a pathology.
However, pronounced EEG changes are usually pathological in nature and are most often associated with a decrease in the functional activity of cortical structures (B). Particularly pronounced changes associated with disruption of the functional activity of all structural formations of the brain are observed in coma.
Periodic focal and regional slowing of the bioelectrical activity of the brain, especially detected during functional stress tests, most often indicates a disruption in the processes of regulation of a particular zone of cortical structures, which can still be restored at rest. Such EEG changes are most often observed with the development of stenotic processes in the main arteries of the head and large segments of the cerebral arteries. Continued focal and regional slowing, as opposed to intermittent slowing, indicates more pronounced (usually structural) changes in neural tissue. Continued deceleration is most often detected in large intracranial processes, such as space-occupying lesions, stroke, local edema (in case of head injury), and atrophic process.
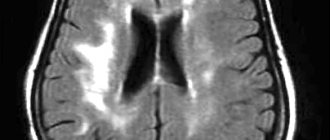
Fig.2. Continued diffuse slowing on the EEG in dyscirculatory encephalopathy2
Signs of a decrease in the functional activity of cortical structures are recorded in the form of erasing zonal differences, as well as a slowdown of the rhythm to the theta range
Fig.3. Periodic slowdown in EEG in atherosclerotic lesions MAG3
Periodic occurrence of focal slow-wave activity of the theta range during functional exercise with hyperventilation (provocation of hypoxia of brain structures)
Fig.4. Continued deceleration due to intracranial space-occupying process (stroke)4
Focal slow-wave rhythm of high-amplitude waves of the delta range corresponding in localization to the affected area.
Fig.5. EEG Diffuse delta activity in a patient in a coma (delta coma)5
Diffuse continuous slow-wave activity of the delta range is recorded - a relatively unfavorable sign.
Fig.6. EEG rigid activity of the alpha range in a patient in a comatose state (alpha coma)6
Slowing is recorded in the form of diffuse, continuous and rigid activity of the lower alpha range, an unfavorable sign
Low amplitude EEG
An electroencephalogram with a characteristic decrease in amplitude is also called a “flat EEG” and is most often considered as a normal variant with a predominance of desynchronizing activity. Read more: EEG norms in children and adults.
Paroxysmal activity of non-epileptiform type
Paroxysmal activity on the EEG is understood as a rapid (sudden) deviation or disturbance in the nature of the recording with the registration of graph elements significantly different from the background activity. The appearance of paroxysmal activity does not always indicate the development of the disease, and can occur in healthy people.
Most often, the occurrence of such activity is observed in childhood and young adults, and is associated with the functional immaturity of the mid-stem structures (B). According to the classification of X. Lueders 2000, these phenomena are designated FIRDA. Their occurrence is associated with the development of acidosis that occurs during stress tests with hyperventilation, which leads to general hypoxia. Functionally immature mid-stem structures under these conditions lose the ability to integrate and regulate bioelectrical activity, and begin to freely transmit bioelectrical impulses to various parts of the cortex. In turn, this change in the EEG is reflected in the appearance of high-amplitude bilateral synchronous waves in the theta and delta ranges, predominant in amplitude in the fronto-central leads.
In children and young people, this condition is not pathological, but reflects only the instability of physiological processes in a young body.
Differential diagnosis of “respiratory waves”
➥ Main article: Respiratory waves on EEG
Respiratory waves should be differentiated from paroxysmal bilateral synchronous slow waves that occur in patients with hemolytic fluid dynamics disorders due to the development of occlusive processes in the cerebrospinal fluid conducting system of the brain. In such patients, changes in the EEG are also detected during functional stress tests, especially during hyperventilation.
Increased excitability of neural structures (epileptiform patterns)
Fig.7.
Scheme of the formation of an epileptic focus in cortical structures ➥Main article: Epileptiform EEG patterns
In general, epileptiform EEG changes are traditionally considered as a subtype of general paroxysmal changes in BEAGM. But since they have a specific mechanism of occurrence, due to the development of increased excitation of nerve cells, with the formation of rhythmic and synchronous discharges. As well as the specificity of this type of changes for epilepsy, it is necessary to consider them within the framework of a separate syndrome.
The formation of epileptiform patterns occurs in cortical structures and is associated with an increase in the functional activity of their neurons. It is based on a pathological hypersynchronous discharge of neurons (microswitches), which is recorded as an acute pattern in the form of a spike or a sharp wave. The depletion of the mechanisms for the formation of axonal APs and the inclusion of the mechanism for the formation of soma APs characterizes the appearance on the EEG of the subsequent acute component of the slow wave. With repeated epileptiform discharges, a general depletion of nerve cells begins to be registered, which is characterized by an increasing slowdown in the frequency of epileptiform patterns with the subsequent cessation of epileptiform activity.
Epileptiform patterns on EEG
Fig.8. Benign epileptic discharges of childhood (BEDC, Rolandic complexes)7
Fig.9. Spike-wave complexes8
Fig. 10. 3-Hz spike-wave complexes9
Fig. 11. Polyspikes10
Rice. 12. Hypsarrhythmia11
Fig. 13.
Photoparoxysmal response12 In contrast to rhythm acquisition, it is characterized by provocation of epileptiform activity during a test with rhythmic FS
Fig. 14. Subclinical seizure pattern13
Generalized epileptiform activity lasts less than 3 seconds, forming an outbreak that does not turn into a paroxysm. The patient's consciousness is preserved
Fig. 15 EEG pattern of attack14
A paroxysm (more than 3 seconds) of generalized epileptiform activity in the form of acute-slow wave complexes is recorded. The patient's consciousness is lost.
Fig. 16. Status pattern15
A long-lasting paroxysm of high-amplitude generalized epileptiform activity is recorded.
Treatment of cortical dysarthria in children
Correction of cortical dysarthria begins with pathogenetic treatment of the disease that led to a speech defect. Without this step, no amount of speech therapy help will help restore speech.
Complex treatment includes:
- drug therapy aimed at stimulating metabolism in the brain and restoring its functions. Prescribe nootropic drugs, vitamins, metabolites. In difficult cases, sedatives, tranquilizers, and antidepressants may be needed;
- speech therapy correction of cortical dysarthria - speech therapy massage, articulation gymnastics, development of fine motor skills of the hands, production of sounds. If necessary, a psychologist is involved in the treatment process;
- physiotherapeutic procedures, reflexology, massage, physical therapy help eliminate muscle paresis and improve blood flow throughout the body;
- Relaxation techniques - art therapy, aromatherapy, music therapy help relieve stress and improve the emotional background.
Conventional treatment is long-term. Specialists prescribe several courses of therapy, during which they can adjust the program taking into account the body’s response to therapeutic measures.
Prognosis and prevention
Timely initiation of therapy using a comprehensive individual approach and the absence of complex neurological pathology are the main conditions for complete speech restoration. The child overcomes his speech impediment and in the future leads a normal life typical for his age. He can study in a regular school and successfully master the school curriculum.
If cerebral palsy or another neurological disease is present, or there is a space-occupying lesion, the prognosis is difficult. In any case, with a competent approach, it is possible to improve speech and reduce the severity of the defect.
Prevention of the cortical form of dysarthria consists of planning pregnancy, giving up bad habits during pregnancy, timely treatment of emerging problems, and preventing complications of pregnancy and childbirth. It is important to choose a method of delivery in advance to prevent birth injuries.
Preparing a child for an EEG
Before the EEG, it is important to tell your neurologist if your child is taking any medications. For example, sedatives, hypnotics, muscle relaxants and anticonvulsants distort the results of the electroencephalogram. It is important to avoid food and drinks containing any form of caffeine for 8 hours before your procedure. Hair should be clean, without applying oils, sprays, creams or lotions, or conditioners. Sometimes they ask you not to sleep for 4-5 hours before the test (for the most accurate result).
A child with autism must be prepared for the procedure in advance due to their behavioral and mental characteristics.