Diffuse brain stem tumor (DSBT) is a neoplasm that represents about 6-8% of cases of known cancers. OSGM accounts for a quarter of a percent of total brain oncology. Unfortunately, the younger generation is also susceptible to this pathology. The real cause of the disease has not been fully determined, and therefore the only chance not to worsen the disease is to recognize the signs that have appeared and begin timely therapy.
What is a brain stem tumor
The structure of the brain stem includes: the base, where the head trunk itself is located, consisting of two substances: gray and white. The trunk itself is small - only 7 centimeters in length. The spinal cord is on one side, and the diencephalon is on the other. Its components: medulla oblongata, pons, midbrain. All nerve nuclei are located in it. There are also centers responsible for: breathing, cardiac function, nerve endings, swallowing, coughing, chewing, salivation, gag reflex. The pons is responsible for the functioning of the eyes, facial muscles, tongue, neck, limbs and torso. Thanks to the work of the nerve nuclei of the medulla oblongata, the work of the muscles of the larynx and pharynx, gastrointestinal tract, hearing and speech of a person is regulated.
Given the importance of the brain stem, any damage or formation entails symptoms that affect health and sometimes life.
Single cavernous malformations of the cerebral hemispheres of cortical and subcortical localization
The vast majority of operations for cavernous malformations of the central nervous system are performed for cavernomas located in the cortex and white matter of the cerebral hemispheres, since they are the most common. This group includes patients with cavernomas located in functionally significant (eloquent) areas, that is, in areas of the brain, damage to which is associated with a high risk of developing severe neurological deficits. High-risk cortical areas include the sensorimotor cortex, speech centers, visual cortex, and insula. Many neurosurgeons believe that for cavernomas of this localization, the possibility of surgery should be considered only in cases of drug-resistant epilepsy, repeated hemorrhages, or increasing neurological deterioration.
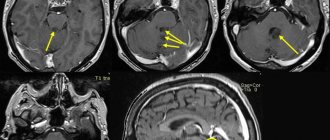
Detection of subcortical cavernoma by changes in the superficial cortex and membranes
Removal of cortical and subcortical cavernomas is usually not difficult. Craniotomy is performed according to standard techniques in the projection of the cavernoma onto the cranial vault. In patients with superficially located cavernomas, in half of the cases more or less pronounced changes in the soft and arachnoid membranes, as well as in the superficial parts of the cortex, can be observed in the form of their yellow color. In some cases, the cavernoma tissue is directly visible.
Encephalotomy is performed at the site of maximum changes in the medulla and meninges, or in the depth of the sulcus closest to the cavernoma. Access planning should be especially careful for cavernomas that are located in the white matter of the hemispheres and are small in size. In such cases, there are usually no landmarks in the form of changes in the surface of the brain. In these cases, it is necessary to use ultrasound scanning and, if necessary, neuronavigation. If it is impossible to detect a cavernoma after 1-2 encephalotomies, it is better to stop the operation, since additional brain injury can lead to the development of neurological defects. Cavernoma removal can be performed as a second step after the location of the formation has been clarified.
If the cavernoma is localized outside functionally significant zones, identifying the formation in the zone of perifocal changes and removing it in one block significantly simplifies and speeds up the operation. Operations to remove cavernomas located in functionally significant cortical and subcortical parts of the brain have a number of features. In case of hemorrhage from a cavernoma of this localization, the patient should be monitored for 2 to 3 weeks. The absence of regression of focal symptoms during this period serves as an additional basis for surgical intervention. When making a decision about surgery, you should not wait for the hematoma to resolve, since due to the processes of organization and gliosis, the operation becomes more traumatic. Access is planned based on minimal impact on a functionally important area. For this purpose, preoperative fMRI, intraoperative stimulation of motor areas, awakening the patient with assessment of speech function, and intraoperative navigation are used. Internal decompression of the cavernoma by evacuation of the hematoma is a necessary step, as it allows to reduce surgical trauma.
It is preferable to perform a control MRI no earlier than 3 months after surgery in order to exclude erroneous interpretation of data due to the presence of fresh postoperative changes. When evaluating postoperative MRIs, the use of intraoperative hemostatic materials must also be considered.
Removal of insular cavernoma with good outcome
The main criteria for the effectiveness of operations for cavernomas of cortical and subcortical localization should be considered complete excision of the malformation and, as a consequence, the absence of repeated hemorrhages, as well as the cessation or significant reduction in the frequency and severity of epileptic seizures, in the absence of deterioration of neurological functions. Considering the absence of neurological symptoms before surgery in the vast majority of patients, as well as the benign nature of the disease, the appearance or worsening of a neurological defect should be regarded as an undesirable outcome. According to generalized data, a neurological deficit after removal of cavernomas from functionally significant areas of the cortex and subcortical parts of the cerebral hemispheres develops in approximately a third of patients.
Complete excision of the cavernoma guarantees the cessation of hemorrhages. Efficacy regarding the postoperative course of epilepsy is not so obvious. Meanwhile, getting rid of seizures is one of the main tasks in the treatment of patients with cortical cavernous malformations. Data obtained in different years and on different clinical material generally indicate a positive effect of surgery on the course of the epileptic syndrome. 60% of patients are completely freed from seizures, and another 20% of patients experience improvement in the course of the disease in the form of a decrease in the frequency and severity of epileptic seizures. Almost all researchers note the best effect when the operation is performed in the immediate period after the onset of seizures, as well as in patients with fewer seizures. Other prognostic factors for a good outcome of surgical treatment of epileptic syndrome also include age over 30 years, medial temporal localization of the cavernoma, its size less than 1.5 cm, and the absence of secondary generalization of seizures.
Cavernoma excision supplemented with amygdalohippocampectomy
Currently, the method of choice for the surgical treatment of patients with cavernous malformations manifested by epileptic seizures is the operation of cavernoma removal, which can be supplemented by resection of the altered medulla if the cavernoma is localized in a functionally insignificant area of the brain. During extended operations, intraoperative use of ECoG is advisable to assess the need and extent of excision of the perifocal zone and/or distant foci of epileptiform activity. Given the existence of known limitations, the method is the only possible way of intraoperative functional assessment of the state of the brain and, in certain situations, can affect the course of the operation. The validity of amygdalohippocampectomy in patients with cavernomas requires further consideration. The AMGE operation can be performed in cases of drug-resistant epilepsy with frequent seizures in patients with temporal lobe cavernoma. Preoperative examination of such patients should be carried out according to the rules for treating patients with “classical” epilepsy. It should include pre- and postoperative neuropsychological examinations, various methods to clarify the ictal focus (EEG monitoring or video-EEG monitoring to record the seizure pattern, if necessary, examination with implantation of invasive electrodes, high-resolution MRI, MEG and PET), use of ECoG for intraoperative clarification of the resection zone. In severe forms of epilepsy, two-stage operations are also justified. They consist of removing the cavernoma, and if this operation is ineffective, examination and surgical treatment in accordance with the standards of treatment for “classical” epilepsy.
Types of tumors
There are two types of tumors: primary and secondary. Disruptions in brain activity caused by harmful factors will ultimately lead to the chaotic division of damaged cells until they are completely replaced by healthy ones. This is how a primary tumor of the brain stem appears in children and older people. It is based on glial cells. Brain stem cancer can start and develop in one part of the organ. A common place for oncology to appear is the bridge (about 60%). Slightly less - in the midbrain and medulla oblongata. Brain stem tumors occur in the plural.
Secondary are those that appear in one place and continue to grow on the brain stem. Moreover, in only 5% of cases, metastases occur in the trunk, penetrating from other organs. A brain stem tumor is a parastem formation (para – about).
Common types of tumors are gliomas, which develop from glial cells.
- Astrocytomas account for about 60% of diseases. There are multiforme, pilocytic, anaplastic and fibrillary. Benign ones include pilocytic and fibrillary. Pilocytic forms occur in children. Glioblastoma (multiforme) is considered aggressive, which occurs most often in men under 50 years of age.
- Ependymomas account for 5% of all tumors. Most often it is benign.
- Oligodendrogliomas occur in 8% of diseases. Large tumor sizes. There are 4 degrees of malignancy.
Stages of brain cancer
Brain cancer is characterized by 4 stages of development. Let's look at each of them:
- First stage. The tumor has already formed, but its size is still small. Symptoms indicating the onset of the disease do not appear or are completely insignificant. At this stage, only the appearance of a headache is possible, which intensifies in the evening. The tissues that surround the tumor are not yet affected.
- Second stage. The brain tumor gradually increases in size and begins to put pressure on neighboring organs. As a result of this exposure, some important body functions are disrupted. It is already possible to identify focal symptoms. At this stage, surgery for a brain tumor is expected. If the cancerous tumor does not exceed 3 cm in size, then it is removed using radiosurgery (Cyber legs and others). This method of treatment is the most gentle and effective for the patient - there is no need to perform craniotomy and additional incisions. To exclude the occurrence of relapse and eliminate the remaining single cancer cells, chemotherapy is carried out.
- Third stage. The brain tumor has already grown quite strongly and metastases have appeared. In addition to focal symptoms, there are also general cerebral symptoms. The growth of cancer cells accelerates. Radical treatment methods are still possible, but achieving a positive effect will be quite difficult.
- Fourth stage (final). A cancerous tumor manifests itself as clearly and aggressively as possible. Metastases are found in the organs most distant from the source of the disease, in bone tissue. Since radical treatment methods did not have a positive effect, it is time to use palliative methods. This means that it is no longer possible to completely eliminate the disease. Therefore, palliative therapy is aimed only at improving the patient’s quality of life, pain relief and relief of painful symptoms, regardless of how long he has left to live.
Symptoms
When gliomas appear, the destruction of brain stem tissue begins. Depending on the affected area, focal symptoms of the disease appear. Unfortunately, with the appearance of a tumor, other organs also suffer - the tumor, increasing in size, impairs blood circulation and increases intracranial pressure.
Brain stem tumor symptoms to look out for include:
- Headache. 90% of patients complain about it. The tumor puts pressure on the nerve endings, membranes, and blood vessels of the brain. It can appear both locally and be felt throughout the head. The intensity varies - from strong to dull. It occurs suddenly, most often in the morning.
- Nausea, sometimes with vomiting. Appears in the morning.
- Incorrect position. The patient prefers to hold the head in a manner that does not irritate the nerves in the neck and skull.
- Mental disorders. This symptom can be observed both locally and generally. Such disorders include deafness, irritability, and changes in consciousness. The patient feels lethargic, apathetic, does not want to talk, and does not react to anything.
- Epilepsy.
- Decreased visual acuity, which appears due to intracranial pressure. The fundus of the eye changes - the discs swell, their color changes.
- Bulbar syndrome.
- The structure of the skull changes - the seams diverge, its walls become thinner.
Focal symptoms include:
- Damage to motor functions, loss of orientation, tactile and visual perception disappears, gait changes.
- Hearing and sensitivity decrease.
- Paresis and tremors appear.
- Blood pressure surges.
- A facial disorder (distorted smile) appears.
- The clinical picture of brainstem tumors includes delayed onset of intracranial pressure and accumulation of cerebrospinal fluid in the brain (hydrocephalus).
There are many structures in the brain stem that can be affected. When central paresis is affected, tremor appears, dizziness occurs, problems with hearing and vision appear, strabismus may develop, and difficulty swallowing appears. Paresis in the limbs may occur. With the progression of tumor growth, these symptoms increase, and new ones appear - nausea, headache, vomiting. The patient dies due to malfunctions of the cardiac, vascular centers and respiratory organs.
Surgery to remove glioma
A neurosurgeon will provide professional assistance to patients. Contact neurosurgery-msk.ru. He provides effective treatment for brain glioma mainly using surgical methods. The specialist first performs an examination, evaluates the patient’s complaints, and prescribes a comprehensive examination. Diagnosis includes echoencephalography and electroneurography. Additionally, an ophthalmological examination, MRI, and CT scan of the brain are prescribed.
Brain glioma is differentiated from abscess, epilepsy, and other neoplasms of the central nervous system. The rate of tumor growth can be judged from the results of PET-CT.
The main treatment method is surgery to remove the glioma. Additional techniques, including chemotherapy, are used for inoperable tumors or as an adjunct to surgical tactics.
Many patients prefer to undergo brain glioma removal at the Medsi Clinic. This ensures that you receive qualified neurosurgical care throughout your hospitalization and recovery.
Localization in the frontal lobe
With glioma in the frontal lobe of the brain, the main clinical manifestations do not appear for a long time. First of all, patients notice general cerebral symptoms, which are often associated with prolonged exposure to stress, problems at work and in their personal lives. As the tumor grows, additional symptoms appear, including seizures and visual disturbances.
Localization in the brain stem
Such a tumor is called diffuse. It has characteristic manifestations. On one side of the head, the patient experiences disturbances in the functioning of the cranial nerves, and in addition, decreased sensitivity in the limbs and problems with coordination of movements, but on the other side of the body. Without timely treatment, brain stem glioma causes life-threatening complications, including hydrocephalus, speech and thinking disorders.
Localization in the parietal lobe
A tumor of this type provokes sensory impairment in the extremities. Parietal lobe glioma causes characteristic clumsy movements. Patients cannot move normally and note a noticeable decrease in quality of life. Possible impairment of habitual skills, including loss of the ability to pronounce certain complex words, count, write and read.
Localization in the temporal lobe
The main clinical symptom is hallucinations. With glioma of the temporal region, visual disturbances may occur. Many patients lose half of their visual fields. In most cases, temporal lobe glioma causes memory loss and the inability to perceive human speech. At an advanced stage of the disease, convulsive seizures appear.
Optic nerve glioma
There are no symptoms of the disease for a long time. Optic nerve gliomas occur at a young age. The disease causes myopia and even complete blindness. At a late stage of development, exophthalmos occurs. The tumor grows predominantly from astrocytes.
Localization in the cerebellar vermis
The disease is accompanied by focal and cerebral symptoms. Due to increased intracranial pressure with cerebellar vermis glioma, patients complain of headaches, nausea and vomiting, and dizziness. Long-term symptoms include signs of facial asymmetry, strabismus, and blurred speech.
Localization in the quadrigeminal region
This type of tumor is quite rare. It is classified as a neoplasm of the brain stem. A typical symptom is impaired pupil reaction up to complete lack of sensitivity. Quadrigeminal glioma causes swelling of the meninges, which begin to swell, increasing cerebral symptoms.
Localization in the corpus callosum
The tumor consists of astrocytes. Glioma of the left frontal lobe most often grows into the corpus callosum. It is detected mainly in men after 40 years of age. Glioma of the corpus callosum is characterized by a high degree of malignancy and has an unfavorable prognosis.
Pontine glioma
Tumors of the pons can occur without obvious symptoms. The disease leads to cranial nerve palsy. Pontine glioma affects the neural structures of the face. Accompanied by dizziness. The absence of cerebral symptoms causes certain difficulties in diagnosis. Patients often adopt a forced head position, which reduces dizziness. It is worth paying close attention to this sign, as it often accompanies the growth of brain tumors.
Glioma of the 4th ventricle of the brain
Such tumors are localized in the posterior cranial fossa. They cause increased intracranial pressure and swelling of brain tissue. Closure of the lumen of the 4th ventricle causes severe headache, nausea and vomiting. Such tumors are characterized by Bruns syndrome. It occurs due to a violation of the normal outflow of cerebrospinal fluid.
Stages of the disease
In medicine, there is a classification of oncological diseases. It is expressed in degrees:
- The first degree is benign. They grow slowly, up to ten years.
- The second degree is borderline.
- The third and fourth are the highest, having an indicator of malignancy. The growth of tumors is rapid - a person with similar degrees can live from a couple of months to several years.
Unfortunately, benign tumors can eventually develop into malignant tumors.
Radiation dose for brain stem tumors
Some researchers believe that only 20-30% of patients who have brainstem glioma have a positive prognosis with 55 Gy of radiation. The low percentage of achieving local tumor destruction forced scientists to look for new ways to temporarily administer the dose. Thus, hyperfractionation began to be used. By irradiating a brainstem tumor with 1 Gy twice a day to a total dose of 72 Gy, we noticed that 30% of patients lived for 2 years, and the survival rate among patients with a diffuse tumor averaged 1 year. High-dose radiation through hyperfractionation increases the effectiveness of treatment.
Causes of pathology
Oncology can occur for various reasons. Doctors call the most common heredity, genetic predisposition, exposure to chemicals, and radiation.
Deviations in genetics include the following syndromes: Turco, Li-Fraumeni, Gorlin, tuberous sclerosis, Von Recklinghausen's disease, Burkitt's tumor.
Unfortunately, medicine has not yet found the exact causes of cancer in humans. Therefore, to date, no remedy has yet been found to help prevent cancer.
Diagnosis of a brain tumor
In order for the doctor to make a diagnosis, he must first collect an anamnesis. It is very important to answer all questions about symptoms as accurately as possible. If neurological abnormalities are observed, the patient must be sent to a neurologist.
At his appointment, he undergoes an examination and various tests that reveal motor dysfunctions. The doctor will definitely check whether all reflexes are present and whether there is tactile and pain sensitivity. An examination by an ophthalmologist is required, where the patient's fundus is measured. If necessary, the patient is referred to an otoneurologist for a hearing test. After collecting anamnesis, the neurologist will be able to make a diagnosis. If necessary, a neurologist can prescribe CT and MRI, which help detect tumors of minimal size, determine the location of the tumor, and the type.
Additional studies include craniography (x-ray of the skull), which can show whether there is a change in the bones of the skull, encephalography (determining changes in the brain), echoencephaloscopy (ultrasound diagnostics), radioisotope scanning, angiography.
A biopsy is not performed for brain stem cancer. Histology is carried out solely on the basis of data on location, symptoms, and the age of the patient.
Meningioma: symptoms, risk factors and treatment
Neurosurgery Jan 30, 2020
What is Meningioma?
Meningiomas are tumors of the meninges, the membranes that surround the brain and spinal cord. Even if they are not brain tumors, they are included in this category because they can affect the brain, nerves and adjacent vessels, compressing them.
Most meningiomas grow very slowly over several years without causing any symptoms or discomfort. But in some cases, serious changes occur in the brain tissue, nerves or nearby vessels, so it is important to monitor the tumor's development.
In terms of the incidence of brain tumors in adults, meningioma ranks second and in most cases affects women over 50 years of age, but this disease can occur at any age in both men and women.
Symptoms
Often meningioma can develop asymptomatically or with minor symptoms, especially at an early stage. Depending on the area of the brain where it is located, symptoms may include:
- Headaches that get worse over time
- Behavioral changes
- Weakness or numbness in one part of the body, limbs
- Changes in vision, such as doubling or blurring of the image
- Difficulty concentrating
- Hearing loss
- Memory loss
- Loss of smell
- Convulsions
When is it necessary to see a doctor?
Most signs and symptoms of meningioma progress slowly, but sometimes meningioma requires treatment as quickly as possible.
You should immediately consult a doctor if:
- Sudden onset of convulsions
- Sudden changes in vision or memory
- The occurrence of paresis or paralysis of the limbs
It is necessary to consult a neurosurgeon or neurologist if you have persistent symptoms such as headaches that get worse over time.
Often, because meningiomas are not clinically apparent, they are only discovered by X-ray examinations performed for reasons not directly related to the tumor (head injury, stroke, or headache).
Causes
The exact cause of meningioma has not been determined. It is known that some meningeal cells undergo changes that lead to loss of control over their proliferation, which leads to the appearance of meningeal tumors (meningiomas).
This may be due to genetic predisposition, hormones (which may explain the higher incidence in women), radiation exposure, or other largely unknown factors. There is no evidence to support the idea that meningiomas are caused by mobile phone use.
Risk factors
There are a number of factors that can trigger the appearance of meningioma:
Radiation therapy. Radiation therapy, which includes radiation to the head, may increase the risk of meningioma.
Female hormones. Meningiomas are more common in women, leading doctors to believe that female hormones may play a role. Some studies have also found a link between breast cancer and the risk of meningioma associated with hormone exposure.
Genetic diseases of the nervous system . Neurofibromatosis type II is a rare disease that contributes to the development of meningioma and other brain tumors.
Obesity. A high body mass index is an established risk factor for many types of cancer. We mostly see meningiomas in obese people; several studies have been conducted in this direction, but they have not been scientifically confirmed.
Diagnostics
Meningioma can be difficult to diagnose because the tumor often grows slowly. Symptoms of meningioma may not be accurate and may be confused with symptoms of other diseases or considered normal signs of aging. If your doctor suspects meningioma, you should contact a specialist in diseases of the central nervous system (neurosurgeon).
To diagnose a tumor, the neurosurgeon will perform a complete neurological examination followed by tests such as:
Computed tomography (CT) . CT scans are performed using X-rays, which create complete images of the brain. Sometimes an iodine-based contrast agent is used to improve the image.
Magnetic resonance imaging (MRI). This research uses a magnetic field and radio waves to create images of brain structures. MRI provides a more detailed picture of the brain and meningiomas in particular.
In some cases, a small piece of the tumor may need to be examined (biopsy) to rule out other types of tumors and confirm the diagnosis of meningioma.
Treatment
Treatment for meningioma depends on many factors, including:
- Size and location of the tumor
- Percentage of tumor growth and aggressiveness
- Patient's age and health status
Wait and see tactics
Not all patients diagnosed with meningioma require urgent treatment. A small, benign meningioma may not require treatment. If a decision is made that does not include treatment, it is necessary to carry out periodic examinations to monitor and keep the tumor under control.
If the doctor concludes that the meningioma is in the growth phase and needs treatment, there are several options.
Surgical intervention
If the tumor causes symptoms or shows signs of growth, surgery is recommended.
The goal of neurosurgery is to completely remove the meningioma. However, if the tumor develops near structures that are responsible for important functions of the brain or spinal cord, it is not always possible to remove all of it. In these cases, as much of the tumor as possible is removed.
Postoperative treatment tactics depend on several factors:
- If the tumor has been completely removed, no further treatment is required. However, periodic examinations are mandatory.
- If the tumor is benign and only a small part of it remains after surgery, the neurosurgeon can only recommend periodic examinations (CT, MRI). In some situations, small parts of the remaining tumor may be removed using stereotactic radiosurgery (SRS), a very precise form of radiation therapy.
- If the tumor is atypical or malignant, radiation therapy will be required to reduce the risk of recurrence.
Like any surgery, meningioma removal may carry some risks, including infection and bleeding. The risks vary from case to case and largely depend on the location and size of the tumor. The experience of the surgical team and the equipment used play an important role in this type of operation.
Radiation therapy
If the meningioma cannot be completely removed by surgery, radiation therapy is recommended after surgery. The goal of radiation therapy is to kill remaining cells and reduce the chance of tumor recurrence. Radiation therapy is carried out using a machine that emits high-energy rays at tumor cells. Recent technological advances in radiation therapy have made it possible to increase the radiation dose for meningioma, reducing the radiation exposure to healthy tissue. There are several options for radiation therapy for meningiomas, such as stereotactic radiosurgery, proton radiation therapy.
Chemotherapy is rarely used to treat meningiomas, but may be used in cases where the patient does not respond to surgery and radiation therapy.
Medical observation after brain surgery
Immediately after surgery, the patient is closely monitored in the intensive care unit.
Recovery from brain surgery depends on the type and extent of surgery performed. Hospitalization for brain surgery can last up to a week or more, depending on many factors, including the general condition of the body, the age of the patient, and the complexity of the surgery.
Before discharge, the neurosurgeon will explain the next steps in the recovery process. This will include instructions on how to care for the surgical wound, advice on what activities are permitted, and clarification on when to return to the doctor.
Author: Dr. Adrian Danu, neurosurgeon, highest category
For registration and questions, contact us by phone. +373 (22) 40 00 40 (available 24/24).
Treatment
The most effective methods include operations that are aimed at removing tumors.
During the operation, the doctor cuts off the largest part of the formation. To perform the operation, the patient needs to open the skull. In some cases, surgery is not performed on the brain stem, since there is a high probability that vital centers may be affected. The decision on the need for surgery is made based on the size of the tumor and location. The tumor is cut off using endoscopic or laser removal. The laser option cauterizes the edges of the tissue and stops bleeding. The operation is performed using a robotic system, minimizing all kinds of complications.
Radiosurgery is radiation therapy that is based on the use of a single exposure to a high dose of radiation. Used for relapses and metastases.
HIFU therapy, which uses high-intensity ultrasound.
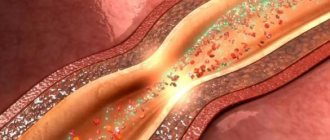
Cryodestruction – freezing with liquid nitrogen. To perform this you need a cryoprobe. The photo below describes the mechanism of action of cryotherapy. The mechanism in the brain is similar.
Treatment and removal of brain cancer
To treat brain cancer, radical therapy is mainly used - surgery. If the diagnosis was carried out on time and efficiently, then removal of brain cancer is successful in most cases. Relapses occur in rare cases. If metastasis growth is detected, repeat surgery is possible.
During surgical treatment, a laser and other special instruments are used. Cryocoagulation has shown the greatest effectiveness in the treatment of benign neoplasms on bone and soft tissues. During the procedure, the tumor is exposed to liquid nitrogen, argon or helium. Low temperatures instantly destroy cancer cells. The advantage of this treatment is the absence of side effects such as vomiting and nausea.
If the tumor is small, hormone replacement therapy is prescribed. This treatment of a brain tumor does not entail disruption of the patient’s hormonal levels and is quite easily tolerated. This method has proven itself to be especially effective in the treatment of pituitary adenomas. The drugs used during therapy are aimed at stabilizing the level of prolactin in the patient's body, which leads to a decrease in tumor size.
Many severe cases of brain disease require a comprehensive approach. However, it is not always possible to undergo surgery. It all depends on what part of the brain the tumor occurs in. In this case, the removal of the cancerous tumor is carried out using modern ultrasound and laser methods.
Chemotherapy is indicated to reduce the size of the tumor. It can also be used to stop the growth of metastases. Taking into account the severity of the disease, stage of development and general condition of the patient, an individual course of treatment is drawn up.
Conservative (palliative) therapy is of an auxiliary nature. The goal of this method is to alleviate the patient’s general condition as much as possible. The patient is prescribed a course of pain medication (narcotic analgesics), antiemetics, sedatives and anti-inflammatory drugs, and glucocorticosteroids.
Radiation and chemotherapy
After the operation, radiation therapy is prescribed 14-21 days later. Doctors use radiotherapy (external beam radiation). The course ranges from ten to thirty procedures. Radiation dose – up to 70 Gy. If there are many metastases and malignant astrocytomas, it is necessary to irradiate the head. Radiation dose – up to 50 Gy. This treatment is suitable for inoperable patients who have a diffuse type of oncology.
Chemotherapy is carried out along with education. Treatment for diffuse brainstem tumor is a course of several drugs. The duration of treatment with chemotherapy should be from 1 to 3 weeks. After a break, repeat. During treatment, tests are taken that will show whether chemotherapy needs to be continued or whether it will be cancelled.
Method of implementing radiation therapy
Pontine gliomas are characterized by infiltrating growth, often involving the midbrain (quadrigeminal) and cerebellum in the tumor process. It is important to take such information into account when choosing the volume of tissue for irradiation. That is why the brain stem is included from the quadrigeminal region to the level of the first cervical vertebra (C1). The use of opposing fields and high-energy radiation is useful.
For midbrain tumors, local irradiation can be performed. In this case, the irradiation area includes the primary tumor and 1-2 cm of adjacent tissue. In 16-20% of patients with brainstem gliomas, subarachnoid metastasis is present. Such tumors are characterized by local progression.
Forecast
Unfortunately, the prognosis is disappointing. Even after a complex of treatment, the survival rate is 60%. If a patient is contraindicated for surgical intervention or has an advanced disease, he or she is less likely to live 5 years (the patient is one of 30-40% of people).
People with the most aggressive forms of cancer live no more than one year. Unfortunately, some survive only a few months. Children, due to their growing bodies, have a better chance of surviving than adults or older people.
People with certain diseases: non-Hodgkin's lymphoma, brain stem cavernoma, sarcoma tumor, HPV, lymphoma tumor, unfortunately, will not be able to live long.
Symptoms
The brain stem contains nerve centers that regulate breathing and heart function. Therefore, it takes part in regulating the movement of the eyes, facial muscles, speech, hearing, and swallowing. Nerve fibers run through it, innervating the muscles of the limbs and body. Based on this, in the case of damage to the brain stem by a tumor process, many symptoms develop, reflecting a violation of the above functions.
Signs of the onset of the disease depend on where the tumor forms. Strabismus, twitching of the eyeballs, facial asymmetry, hearing loss, dizziness, and weakness in the limbs or half of the body may occur. A shaky gait and hand tremors may appear. In the case of a prolonged course of the disease, the symptoms intensify; headache and vomiting may occur, which is explained by an increase in intracranial pressure as a result of an increase in tumor size, and most often due to the formation of cerebral hydrocele. If the complaints or signs described above occur, then you need to contact a neurosurgeon, neurologist and be examined.