Neuritis of the facial nerve is a partial or complete dysfunction of the facial nerve. The facial nerve is the nerve that is responsible for the facial muscles of the face. With facial neuritis, symptoms appear suddenly or develop within 48 hours. Often this is first noticed by the patient's family members (deviation of the nasolabial fold or slurred speech). Patients often noted that they noticed these symptoms in the morning. Other common symptoms of neuritis are numbness or burning in half the face, facial asymmetry or drooping corner of the mouth on one side, increased sensitivity to loud sounds, watery or dry eyes, difficulty eating, headache, pain behind the ear, changes in taste.
This disease affects 1 in 5,000 people in the United States each year. Facial neuritis can occur at any age. Neuritis of the facial nerve occurs more often in pregnant women, patients with diabetes, after influenza or acute respiratory infections, or simply hypothermia.
Cause of facial neuritis
The cause of Bell's palsy is unknown. However, the most common theory is about the viral etiology of the disease. According to this theory, under certain circumstances, a virus like HSV-1, which usually lives within nerve cells, is activated. The virus begins to actively multiply and produce toxic substances. As a result, inflammation of the nerve occurs and disruption of the conduction of electrical impulses along the nerve fiber. Most patients with sudden loss of facial nerve function on one side are diagnosed with Bell's palsy.
However, this diagnosis must be made by a doctor, such as a neurologist. There are many other causes of facial paralysis. The doctor will look at how quickly the symptoms began, whether there are other symptoms such as fever, headache, hearing loss, dizziness, weakness or numbness in the arms and legs, difficulty swallowing, and hoarseness. The doctor will also need to find out about pre-existing medical conditions, medications, and family history. In addition, a full inspection is required.
Other causes of facial neuritis are: ear infections and tumors, trauma, Lyme disease, brain tumors, stroke, etc.
If the symptoms progressed slowly over 3-6 months, the presence of constant headaches was noted, or there was a transient nature of the symptoms, then this is not Bell's palsy.
The prognosis for neuritis of the facial nerve is quite good. If the dysfunction was incomplete (a certain range of muscle movements was preserved), then the likelihood of a complete recovery is very high. In this case, 95% of patients will have complete recovery of nerve function. In a small number of patients, minor disturbances (asymmetry when smiling or twitching) may persist.
With complete paralysis, it is possible to achieve up to 80% recovery, that is, practical restoration of functions in full. Approximately 17 percent of patients experience persistence of some dysfunction. This may be some weakness of the facial muscles, twitching of the lip or eyelid. A small percentage of patients (4 percent) may have more significant dysfunction, such as persistent facial muscle weakness or twitching.
Typically, most patients begin to regain function within 3 weeks. The earlier recovery begins, the better the final result. If paralysis does not recover within 3 months, then another pathology is likely.
Paralysis
Polio
Encephalitis
Tick-borne encephalitis
Syphilis
Stroke
18340 September 17
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Paralysis: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition _
Paralysis is a complete loss of movement in one or more parts of the body, loss of muscle strength in a muscle or group of muscles, and inability to perform movements. In some cases, the term is used to describe muscle contractility disorders. Paralysis is not an independent disease, but only one of the symptoms of many organic pathologies of the nervous system.
A condition in which voluntary movements are not completely lost is called paresis.
Types of paralysis
Any damage to the nervous system can lead to impaired motor function. There are organic, functional and reflex paralysis.
Organic paralysis is formed due to the fact that the nervous system (at any level) is affected by tumors, injuries, infections or any other factors.
Functional paralysis in most cases occurs as a result of the formation of a so-called stagnant region of inhibition in the brain, which prevents the muscles from receiving the command to contract. During the development of the disease, no pathological changes occur, reflexes remain normal, muscle tone is maintained at the proper level. Reflex paralysis is caused by damage to the peripheral motor neuron and can be caused by damage to any part of the nerve pathway. From an anatomical point of view, a distinction is made between paralysis caused by damage to the central nervous system (brain or spinal cord) and paralysis associated with damage to the peripheral nerves.
The variety of causes of paralysis is reflected in pathomorphological changes, which can have a very different nature and location.
Paralysis is divided according to severity, persistence and prevalence. It can be complete or partial, irreversible or transient, localized or widespread.
None of these clinical types is an independent pathology, however, there are certain types of paralysis that represent independent diseases. These include Parkinson's disease (shaking palsy), polio (infantile paralysis), Bell's palsy, bulbar palsy, pseudobulbar palsy, familial periodic paralysis, brachial plexus palsy, cerebral palsy and others.
Destruction, degeneration, inflammation, formation of foci (plaques), sclerosis, demyelination are the most typical types of pathological changes in nervous tissue that are detected during paralysis. According to their development, acute and flaccid paralysis are distinguished. In the first case, the symptoms increase very quickly, in the second, immobilization develops gradually.
The following classification of paralysis is distinguished, based on the prevalence of the process:
- monoplegia - paralysis of one limb on one side of the body;
- paraplegia - paralysis of two limbs of the same type, for example, both arms;
- hemiplegia – paralysis develops in the limbs on one side;
- tetraplegia – all four limbs are affected simultaneously;
- Ophthalmoplegia is paralysis of the muscles that provide motor activity to the eyes.
With central paralysis, motor function as a whole usually suffers, but not individual muscles.
Paralyzed muscles are spastic (convulsively tense), but do not undergo atrophy (it can only be a consequence of inactivity), and there are no electrophysiological signs of degeneration. In paralyzed limbs, deep tendon reflexes are preserved or enhanced. When peripheral motor neurons are damaged, instead of increasing muscle tone, it decreases. Individual muscles are affected, in which atrophy and an electrophysiological reaction of degeneration are detected. In a paralyzed limb, deep reflexes are reduced or completely disappear, and clonus are absent.
Psychogenic paralysis, which is not based on organic damage, can imitate one of these options or combine features of both. Central paralysis can appear in its pure form or be combined with features of peripheral paralysis. As a rule, it is accompanied by sensory and trophic disorders, as well as changes in vascular tone.
Peripheral paralysis is often accompanied by sensory impairment.
Possible Causes of Paralysis
There are different causes of paralysis, but they all boil down to damage to the nervous system caused by injury, tumor, abscess or inflammation. In addition, paralysis can occur as a result of demyelinating diseases associated with the destruction of the protein that ensures the conduction of nerve impulses along the fibers - myelin. Such diseases include: multiple sclerosis, multiple encephalomyelitis, etc.
Causes of paralysis can also be:
- myasthenia gravis – a disease characterized by pathological muscle fatigue;
- myopathy – congenital or acquired metabolic disorders in muscle tissue;
- poisoning with botulinum toxin (botulism), alcohol, industrial poisons, mercury, organophosphorus compounds, salts of heavy metals, nerve poisons;
- epilepsy;
- diseases associated with dysfunction of motor neurons, resulting in pathology of muscle function and paralysis of the limbs;
- damage to a large nerve trunk;
- amyotrophic lateral sclerosis (progressive degeneration of the central nervous system);
- acute cerebrovascular accident;
- immunoinflammatory diseases, in particular Guillain-Barré syndrome;
- congenital or hereditary degenerative diseases of the central nervous system;
- neoplasms (benign and malignant, including metastatic);
- injuries, if they are associated with damage to motor pathways or directly to motor centers;
- infectious diseases (syphilis, tuberculosis, polio, viral encephalitis, tick-borne encephalitis, meningitis);
- some medications (for example, muscle relaxants “turn off” the diaphragm, which is practiced during abdominal surgery);
- radiation exposure;
- hypothermia.
Which doctors to contact for paralysis
To determine the cause of paralysis, you should contact a general practitioner or. In case of infantile paralysis, it is necessary to urgently show the child. The doctor will conduct the necessary examination, consult with specialized specialists, and prescribe the necessary treatment.
Diagnostics and examinations for paralysis
The first and most common manifestation of paralysis is usually the inability to move and control the musculoskeletal system due to a lack of strength in a muscle or an entire group of muscles, namely:
- a complete lack of muscle strength in the muscles of the upper limbs, as a result of which it becomes impossible to perform actions such as grasping an object, lifting, bending and straightening the arm;
- complete lack of muscle strength in the muscles of the lower extremities, which is accompanied by a lack of active movements in the affected limb;
- drooping of the head forward, which is observed with paralysis of the posterior muscles of the neck.
In addition, there may be slurred speech, deviation of the tongue to the side when sticking it out of the mouth, and retraction of food while eating.
In some cases, there is a disturbance in the movement of the eyeballs, which is manifested by a lack of coordinated eye movement, resulting in the development of strabismus or so-called gaze palsy. With some paralysis, the function of the pelvic organs is impaired, which is accompanied by automatic reflex emptying of the bladder and fecal incontinence.
The symptoms of paralysis depend on its type:
- when the facial nerve is damaged, severe headaches appear;
- with bulbar palsy, immobilization of the tongue develops;
- with paralysis of the diaphragm, breathing stops;
- with spastic paralysis of the larynx, spasm of the upper respiratory tract occurs;
- a symptom of upper obstetric palsy (Duchenne-Erb palsy) in children is dysfunction of the muscles of the shoulder girdle;
- with distal obstetric paralysis (Dejerine-Klumpke palsy), paralysis of the hypothenar, thenar, lumbrical and interosseous, long flexor muscles of the hand and fingers is observed, as a result of which the hand is in the “clawed paw” position or hangs down.
During a neurological examination, a differential diagnosis is made between central and peripheral paralysis.
To do this, the volume of active and passive movements, superficial and deep reflexes, the presence of pathological reflexes, muscle tone, identification of atrophies, hypotrophies, fascicular and fibrillar twitches are checked. After a general examination, laboratory and instrumental research methods are prescribed. To detect signs of poisoning, a toxicological blood test is necessary. A general blood test can reveal signs of inflammation.
Treatment of the disease
Elimination of such a disease can be carried out using both conservative and surgical methods.
In the first case, the standard of treatment measures includes:
- use of medications;
- physiotherapeutic procedures;
- massotherapy;
- exercise therapy course;
- folk remedies.
Drug treatment is aimed at using:
- painkillers;
- decongestants;
- vitamin complexes;
- hormonal medications;
- antiplatelet agents;
- means for improving local blood supply to tissues and normalizing blood fluidity;
- neurotrophins.
Physiotherapy is represented by the following procedures:
- heating and UHF;
- paraffin therapy;
- ozokerite applications;
- acupuncture;
- phonophoresis;
- influence of high-frequency currents;
- magnetotherapy;
- ultrasound.
In combination with drug therapy, treatment with folk remedies is carried out, namely:
- warming with salt;
- drinking a decoction based on hawthorn, peony, calendula or motherwort;
- rubbing warm sea buckthorn oil into the affected area.
In situations where conservative therapy for 3 months does not produce positive results, surgical intervention is necessary. In addition, the operation is indicated for:
- congenital Bell's palsy;
- complete rupture of the facial nerve.
Surgical treatment is carried out using:
- nerve suturing;
- neurolysis;
- autotransplantation.
It is very important to note that it is advisable to perform the operation only during the first year from the moment the correct diagnosis is established, since irreversible atrophy of the facial muscles develops in the future.
Given the secondary nature of Bell's palsy, it is very important to fully treat the underlying disease.
How it all began: a cold, psychosomatics
– I literally work my ass off in a large IT office. I have been building a career since I was 22 years old – and have achieved very decent results. But all this began to affect my health.
Last year, after several months of intense workload, I finally started my vacation - and I completely relaxed. My body was in shock: how could it be, before this there was such a load, mobilization, and suddenly bam - relaxation. My body probably went crazy.
I must say that a couple of weeks before, I caught a little cold and went to the office with an untreated cold. Throat, snot, general fatigue - not to say that I suffered, but somehow I quickly got used to it, but my immune system didn’t like it. Colleagues looked askance, but understood: if I left, our project and the prize would be ruined. So I was waiting for a vacation.
It was wildly hot, I was driving in a car with a friend. Tired, fell asleep at the slightly open window. I slept in a draft for several hours of the road. At the gas station I feel my gums tingling, like after being frozen. I wasn’t particularly alarmed at the time, it was just unusual. Everything seems to be ok with my teeth.
The tingling sensation continued throughout the evening – that’s probably when it all happened, although there was no paralysis. I was just very tired and had a bad headache – it seemed like the temperature was about 40. I tossed and turned all night, couldn’t sleep and felt like there was something wrong with my face. I knew I couldn’t open my mouth, but I thought I was just having a bad dream.
Complications of Bell's palsy
It is important to emphasize that the vast majority of patients with Bell's palsy make a full recovery. However, if the facial nerve damage is severe, there may be some complications, including:
- Improper rerouting of nerve fibers – Nerve fibers grow irregularly. This can lead to involuntary contractions of some muscles. The patient may involuntarily close his eyes while trying to smile. It can also be the other way around: when a person closes one eye, the side of the mouth rises.
- Ageusia is a chronic (long-term) loss of taste.
- Gustatolacrimal reflex - also known as crocodile tear syndrome. When the patient eats, their eyes begin to water. Eventually he disappears. In some rare cases, the problem may be longer lasting.
- Corneal ulceration – When the eyelids fail to close completely, the eye's protective and lubricating tear film may become ineffective. This can cause the cornea to dry out. The risk is even higher if Bell's palsy has also reduced tear production. Corneal ulceration is complicated by infection and can lead to significant vision loss.
Symptoms of the disease
When the facial nerve is faulty, as in Bell's palsy, the following symptoms may occur:
- Sudden paralysis/weakness on one side of the face.
- It may be difficult or impossible to close one of the eyelids.
- Irritation in the eyes due to the fact that the eye does not blink and becomes too dry.
- Changes in the amount of tears the eye produces.
- Parts of the face may droop, such as one side of the mouth.
- Output from one side of the mouth. The amount of saliva has changed.
- Difficulty with facial expressions.
- The sense of taste may change.
- The affected ear may result in sound sensitivity. Sounds seem louder.
- Pain in the front or back of the ear on the affected side.
- Headache
The facial nerves control blinking, eye opening and closing, smiling, drooling, lacrimation and frowning. They also connect to the muscles of the stapes, a bone in the ear involved in hearing.
Kinds
The following types of Bell's palsy are distinguished:
- right-sided - affects the facial nerve on the right side;
- left-sided – affects the facial nerve on the left side;
- Bell's palsy, which affects both eyes at once.
The following stages of this disease are distinguished:
- The first stage is characterized by an increase in the development of symptoms. The duration of this stage is about two days. Acute ischemia and edema develop, which leads to nerve compression.
- The second stage or early recovery stage lasts about a month. Characterized by active restoration of function and regression of edema.
- The third stage or stage of protracted (late) recovery – duration is 4 months. Characterized by slow and incomplete recovery of myelin.
- The fourth stage or the stage of consequences and complications – duration is more than 4 months. The development of residual phenomena in the form of paresis or paralysis, as well as contractures and synkinesis of facial muscles is characteristic.
Unilateral damage to the facial nerve occurs in 75% of cases. Bilateral is much less common and accounts for about 25% of the total number of cases.
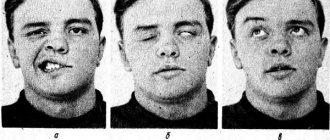
Symptoms
Typically, neuritis of the facial nerve develops gradually. At the beginning, pain occurs behind the ear, after 1-2 days facial asymmetry becomes noticeable, characteristic facial asymmetry is created on the side of the affected nerve:
- smoothing the nasolabial fold
- absence of folds on the corresponding half of the forehead
- The eyelids are wide open and the so-called lagophthalmos (“hare's eye”) - a white strip of sclera between the iris and the lower eyelid
- Dry eyes or watery eyes may occur. In some cases, the symptom of “crocodile tears” develops - against the background of constant dryness of the eye, the patient experiences lacrimation while eating.
On the healthy side:
- a sharp lowering of the corner of the mouth to the healthy side, as a result, the face skews to the healthy side
- less sharp pulling of the nose to the healthy side.
All these disorders are especially noticeable when trying to make active facial movements.
The patient cannot close his eyelids. When he tries to do this, his eye turns upward (Bell's sign).
The weakness of the facial muscles is manifested by the inability to move them:
- when teeth are bared, the mouth and nose are pulled even more sharply to the healthy side
- puffing out cheeks fails
- When you frown, vertical folds do not appear on the affected side
- when raising the eyebrows upward, there are no horizontal folds on the forehead
- drooling occurs due to insufficient function of the oral muscles.
Additional symptoms may accompany the main picture:
- decreased or complete absence of taste sensations in the anterior 2/3 of the tongue
- increased hearing sensitivity (hyperacusis)
- pain in the mastoid area (behind the ear)
- increased sensitivity in the ear area.
For prevention purposes
As a preventive measure, experts advise strengthening the immune system, avoiding hypothermia and drafts, promptly treating infectious diseases, and being wary of traumatic brain injuries.
One of the means of prevention is strengthening the facial muscles through gymnastics. We must take responsibility for our health and treat diseases that can cause complications.
Having discovered the first signs of damage, you should immediately contact a neurologist. Timely treatment will help to completely cope with the disease and avoid complications.
Causes of the disease
Most often, Bell's palsy develops against the background of an infectious process, a viral disease. One of the triggering (provoking) factors of the disease is hypothermia. For example, this could be driving a car with an open window.
The disease occurs due to blockage of the facial nerve, through which the facial muscles are innervated. Often the blockage of the facial nerve is caused by an inflammatory process in the auditory canal during otitis media. Paralysis can also develop with other diseases: meningitis, mumps, injuries, internal bleeding, tumors and others.