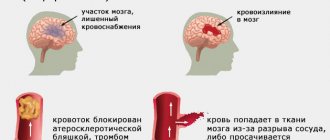
Stroke is a serious disease in which many functions of the body are affected. In case of acute disruption of the blood supply to the brain, some of the cells responsible for certain actions in the body die.
After suffering from this disease, speech and motor functions suffer the most. This article will help answer many questions related to the restoration of the patient’s musculoskeletal system.
In order to understand how complete recovery is possible, you need to pay attention to factors such as:
- previous form of stroke;
- area of brain damage;
- age and general condition of the patient before the stroke;
- completeness and timeliness of medical care to the victim.
In any case, the rehabilitation process is a long-term and difficult period that requires maximum effort and dedication.
When can you start training?
To determine the timing of the start of training activities, their intensity and the possibility of working with an assistant, it is necessary to consider all stages of the disease and their susceptibility to therapeutic effects. There are 6 main periods after a stroke:
- The most acute – the first 24 hours after manifestation. The speed of resuscitation measures and the implementation of high-quality medical intervention directly affect the further recovery of the patient;
- Acute – from the second day to three weeks. Active medical treatment and prevention of negative consequences. During this period, it is not recommended to conduct any activities in order to monitor health conditions and prevent a possible re-strike;
- Subacute – from the fourth week to three months after the moment of impact. During this period, it is recommended to begin performing simple passive exercises with the help of a rehabilitation therapist. An important task is to place the patient's limbs in different positions in order to prevent muscle hypertonicity.
ATTENTION! A prerequisite for speeding up the recovery process is to constantly take medications prescribed by your doctor!
- Earlier recovery - the period from the third to the sixth month from the onset of the disease. Characterized by an active recovery process. Active therapy, massage and physiotherapy are added to the “lying down” exercises. Usually by this period the patient is discharged from the hospital, and he receives all procedures on an outpatient basis or performs them independently at home. But if there is a need or opportunity, then you can undergo a rehabilitation course in a special rehabilitation center.
IMPORTANT! The 4th period is a period of active recovery. If you miss this time, the likelihood of complete and successful rehabilitation is reduced several times.
- Late recovery - from the seventh to the twelfth month. At this stage, the results of previous work are visible. Despite the fact that the potential for recovery decreases every month, constant fruitful work allows you not to stop there, but to continue full recovery.
- Residual effects - the period after one year of treatment. Self-recovery and following doctor’s recommendations continue. Regular consultations and examinations are also necessary to prevent further strokes.
The process of learning to walk
To choose the right program for restoring walking, you need to be able to distinguish the signs of a musculoskeletal disorder:
- unsteadiness of gait;
- inability to fully bend or straighten the limbs;
- impaired coordination of movements;
- decreased sensitivity;
- walking on toes;
- inability to walk quickly.
As mentioned above, treatment with physical exercises must begin from the beginning of the second month.
How to start
There are 4 main stages that precede independent walking.
Stage 1 – passive exercises. These are the very first exercises in a lying position - fixing the limbs in different positions.
All passive exercises are conducted by a rehabilitation specialist. First, he independently warms up the limbs, then connects the patient’s muscle memory. To do this, exercises are performed first with a healthy leg or arm (as a rule, one hemisphere suffers during a stroke), and after the movement they are mentally transferred to the affected limb.
Passive exercises include:
- flexion and extension of the knee joints;
- rotation, flexion and extension of the feet;
- abduction, flexion and extension of the hip joints.
Stage 2 – active exercise and sitting training. After a set of passive exercises, the patient has more strength for new skills. At this stage, you can include the following exercises:
- throwing legs over one another;
- bending and straightening the legs at the knees while lying on the stomach;
- "bike";
- turning the feet from a lying position with bent knees;
- move the heel of the foot along the shin of the other leg;
- lifting with legs moving to the sides;
- lifting the pelvis from a lying position with bent knees;
- raising legs while lying on your side;
- turning to one side.
The last exercise is necessary for further correct sitting. In order to sit the patient down, you need to release your legs to the floor and spread them wider, push off the bed with your healthy hand and take a sitting position.
Stage 3 – learning to get up and stand. When training the process of standing up, the following exercises are used:
- lifting the body while lying on the bed;
- moving along the bed.
After consolidating the exercises and gaining knowledge, the patient can try to stand up.
IMPORTANT! When first attempting to stand up, the patient must be accompanied by a rehabilitation specialist! A fall from muscle weakness can cause shock and delay the rehabilitation process for a long time!
Before the patient himself can take the first steps, it is necessary to do some steps:
- stomping on the spot without lifting your feet off the floor, raising your feet a little later;
- rolling the foot from heel to toe and vice versa;
- stepping over an obstacle - at first it should be something low, with the development of skill the obstacle is increased;
- moving the foot back with support on the toe.
Stage 4 – restoration of the walking process. At this stage, the patient, with the help of a doctor or special assistant, tries to take the first steps. During this period, it is advisable to use special walking devices, for example, three- or four-legged walkers.
Walkers
Walkers are quite heavy and at first will serve as a great support for the victim.
After the patient learns to stand confidently with a walker, then with their help he will be able to move his legs, thereby stepping forward.
It is worth noting that it is necessary to select and adjust the walker correctly so that the rehabilitation process proceeds as quickly and comfortably as possible.
There are different types of walkers on the market, so you can freely choose which one is suitable for a particular patient.
It is worth paying attention to the universal design. These walkers can work as fixed, stationary and walking.
Quick results
For the fastest possible recovery effect, it is necessary to constantly consolidate all the skills acquired during this period with additional exercises and warm-ups. The recommended time for daily exercise is 30 minutes 2 times a day.
If the patient feels strength or, conversely, weakness, then this time must be adjusted depending on the situation.
If a person already knows how to stand up on his own and take steps with support, it is necessary to gradually complicate the activities, for example, by walking on sand or grass. After consolidating these exercises, you need to move on to more complex ones - climbing to small elevations, gradually bringing them to climbing stairs.
To make exercise more comfortable and achieve maximum effect, you must wear special orthopedic shoes that secure the foot.
It is also very important to teach the patient to be independent. He can and should be helped in everything, but not done for him.
The main rule for a quick and effective rehabilitation process is constant exercise with a gradual increase in loads and following all recommendations prescribed by the attending physician.
We invite you to watch an interesting video on the topic:
How to learn the correct gait
After the patient has been able to sit down, stand up and take the first steps independently, it is necessary to use special fixing devices in the exercises to help the correct formation of gait. These include:
- holders for fixing the foot - for proper distribution of weight on the foot and avoiding walking on the toes;
- clamps - knee pads - to hold the knee joint in a vertical position.
One of the effective methods for developing the correct gait is to draw footprints for the patient to walk. This technique is common in rehabilitation centers.
You can also use special treadmills to develop your gait and speed up the recovery process. This device has special extended handrails, the lowest possible speed and an emergency braking button.
IMPORTANT! When performing rehabilitation exercises, you should not rush, even if everything works out; At a rapid pace, one can become accustomed to a comfortable but incorrect position of the ankle joint.
If possible, it is recommended to include Nordic walking in your list of activities.
ABOUT WALKING as a method of REHABILITATION after STROKE.
High-intensity walking is effective in restoring mobility after a stroke.
Rehabilitation programs for stroke patients have traditionally included low-impact walking. High-intensity walking training that mimics real-world conditions can significantly improve mobility in stroke survivors compared with traditional low-impact training, according to a new US study.
The team of rehabilitation specialists published the results of their study in the official journal of the American Heart Association, Stroke, at the end of August 2021. Specialists from the Department of Physical Medicine and Rehabilitation at the Indiana University School of Medicine (USA) took part in the study at the Rehabilitation Hospital of Indiana.
“Stroke survivors often experience difficulty walking and poor balance. Rehabilitation after a stroke traditionally includes low-intensity walking, usually strictly and only forward. This is not enough for the nervous system to prepare it and the body as a whole for real life conditions: uneven surfaces, stairs or changes in direction of movement,” says Professor T. George Hornby, teacher of physiology, physical therapy and rehabilitation physician.
The number of tasks of a specific walking practice included in the rehabilitation plan of a post-stroke patient may influence the speed and efficiency of recovery of motor function. Emerging evidence suggests that markedly increasing the intensity and variability of stepping practice may also be critical, although such strategies are not encouraged during traditional rehabilitation. The purpose of the new study was to determine the individual and cumulative contributions of stepping intensity and variability to improving people's walking speed and duration after impact.
A study has found that stroke patients can perform higher-intensity walking exercises and more challenging tasks than previously thought. According to the study's lead author, “Our research shows that stroke patients can perform higher-intensity walking exercises and perform more complex tasks than we thought was normal and acceptable. We need to go beyond traditional low-intensity rehabilitation to challenge and stimulate the nervous and cardiovascular systems so that patients can restore full body function and adapt it to real-life conditions.”
The study involved 90 people aged 18 to 85 years who had suffered a stroke at least 6 months before the start of the research project. All participants had significantly poor performance on one side of their body.
- The first group of participants engaged in intensive walking training and performed various tasks.
- The second group of participants practiced only intense forward walking.
- The third group of participants walked at a slow pace and performed a variety of tasks, including walking on uneven and inclined surfaces, stairs, randomly placed obstacles on a treadmill, and on a balance beam.
While working with patients, the following was established.
- Patients from groups 1 and 2 began to walk faster and over longer distances than from group 3.
- After training in groups 1 and 2, 57–80% of participants had good clinical indicators, while in group 3, the clinical picture changed for the better in only 9–31% of people.
- Training in group 1 led to an improvement in dynamic balance when walking.
- During training, there was no deterioration in the condition of patients in any of the groups. Thus, it can be assumed that stroke survivors can perform a variety of high-intensity walking exercises.
“When stroke patients exercise more intensely than normal, they see big changes in a short period of time. This increases the efficiency of rehabilitation and the mobility of patients,” Professor Hornby comments on the results.
The researchers' ultimate goal is to incorporate high-intensity exercise training into daily clinical rehabilitation practice after testing a large group of patients.
Read about how walking can eliminate the need for knee arthroplasty if you have osteoarthritis or the risk of developing it on the website of the EVO Specialized Medical Center.
Sources: PLOS.medicine / Operative versus non-operative treatment for 2-part proximal humerus fracture: A multicenter randomized controlled trial
Medical Press / High-intensity step training boosts stroke survivors' walking skills
Devices and simulators
The main devices to help restore walking are walkers, canes, crutches and any other available means that have handrails that you can lean on while moving.
To restore walking, special exercise machines have also been created that allow you to quickly get in shape, namely:
- expander for legs;
- exercise bike - at first used with an automatic motor, which allows you to make movements in the absence of muscle movements; then replaced with a regular one with fixed pedals;
- stepper and step platform - a pedal exerciser for the legs with a handle for body support;
- treadmill – it is advisable to use a special treadmill with additional handrails and supports;
- Shagogon 409 – often used in medical centers; imitates walking in the complete absence of motor ability.
Rehabilitation exercises on simulators
The Yusupov Hospital uses two types of simulators for the rehabilitation of patients after a stroke - mechanical and robotic. Mechanical exercise machines include exercise bikes, treadmills, and exercise machines for restoring balance and gait. Robotic simulators are equipped with electronic biosensors that stimulate activity by influencing the affected limbs. Robotic simulators have wide functionality; they are programmed taking into account the patient’s needs, promote the transmission of nerve impulses from the brain to the injured limb, and stimulate motor activity.
Rehabilitation exercises after a stroke are performed using multifunctional exercise equipment and sports equipment. There are different types of simulators:
- To restore motor activity, use a flexion/extension simulator, a simulator for developing the joints of the limbs, exercise tracks, and exercise bikes.
- For bedridden patients, exercise equipment in the form of a bed or bicycle is used.
- To restore balance, gait, and motor activity, a horizontal simulator is used.
- For patients who cannot yet stand, a seated exercise machine has been created to develop and strengthen the back muscles.