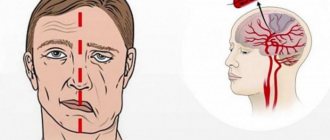
Along with speech and cognitive impairments, patients who have suffered a stroke often develop various types of psycho-emotional disorders. The palm belongs to depression, anxiety, asthenia, apathy, lack of spontaneity, and negativism. Euphoria and complacency are recorded less frequently.
Post-stroke psycho-emotional disorders cause a decrease in the effectiveness of treatment and rehabilitation measures, delaying the prospect of returning to a natural social environment. The development of mental disorders has a depressing effect on patients and their caregivers and significantly reduces their quality of life.
The process of psychological rehabilitation is aimed at the patient’s possible full and early return to work and a full life, overcoming the psycho-emotional consequences of the disease. This is a consistent systemic activity aimed at restoring the patient’s personal and social status.
Psychoemotional disorders as consequences of stroke
A significant number of people experience psychological difficulties, psycho-emotional problems and depression after a stroke. Many sufferers need mental health restoration and relief from depression, anxiety, frustration or anger.
According to statistics, psycho-emotional disorders after a stroke occur in the majority of patients – in 30–65% of cases. The dominant positions are occupied by disorders of the depressive and anxiety spectrum (in 20–45% of patients). These concomitant neurotic and psychotic diseases have a strong negative impact on both the quality of life and the functional abilities of the body.
In a sample of more than 50,000 stroke patients, those patients diagnosed with depression or other mental health problems had a 3-fold increased risk of death within 10 years of the first episode, even after the effects of other negative chronic conditions was statistically controlled.
Post-stroke depression
It has been established that approximately a third of all people who have suffered a stroke develop clinical depression. Women are at higher risk of developing depression than men. Depression after a stroke has both physical and psychological causes. People who had depressive episodes before the stroke are more likely to experience symptoms of the disease after the cerebral circulation has been disrupted. Depressive disorder is closely related to existing cognitive impairment after stroke, so these two problems must be considered and resolved together.
Gloom, sadness and sadness have a huge negative impact on the lives of people after stroke and those who care for them. People who are used to living independently suddenly become dependent on caregivers. A stroke results in significant physical, psychological and financial changes that a person must make in their daily life. Psychotherapy and other forms of psychological counseling can help restore a proper level of independence and gradually adjust to the changes caused by the stroke.
Several factors influence the risk of developing and severity of depressive disorder.
Among them:
- the area of the brain affected by the stroke;
- personal and family history of mood disorders or pathological anxiety;
- level of social isolation before stroke.
The disorder is diagnosed if the classic depressive triad of symptoms has been present for more than two weeks.
Typical signs and warning signs include:
- deep all-encompassing sadness;
- causeless anxiety;
- loss of interest in activities that were once enjoyable;
- lack of motivation to activity;
- difficulties in making decisions;
- poor concentration;
- difficulty remembering details;
- low self-esteem;
- feeling of uselessness, helplessness;
- problems with sleep quality, difficulty falling asleep;
- overeating or loss of appetite.
Some people who are depressed may be unable to properly modulate their emotions. They may laugh or cry for no reason and become emotionally unstable. Existing drug or alcohol problems may resurface or worsen, making rehabilitation efforts much more difficult.
Recovery from depression takes time and consistent medical work, but proper treatment ensures the patient’s full recovery. Currently, specialists from the community of rehabilitation specialists and psychologists Irakli Pozharisky use the most common and effective methods of psychotherapeutic treatment of depression.
People recover faster after a stroke if they receive good support and comprehensive care. Patients recover more quickly when their care is well managed and a well-coordinated team of caregivers identifies and meets needs as they arise. The rehabilitation period after a stroke also requires that the individual be highly motivated to adhere to the care plan. Early identification of depression ensures that patients receive the support and understanding needed to adapt to sudden changes in their lives.
Mania is a syndrome that, along with depression, is the main manifestation of bipolar affective disorder. Mania is characterized by a triad of symptoms: elevated mood (hyperthymia), ideational and mental arousal in the form of acceleration of thinking and speech, and motor agitation. It is also characterized by increased instinctive activity, increased distractibility, and overestimation of one’s own personality [1].
Affective disorders are widespread in various organic brain lesions [1, 2]. For example, the incidence of depression after stroke is about 30% [2]. The incidence of mania after stroke is not precisely known, but according to some authors it is about 1% [3]. Cases of the development of mania have also been described in other neurological diseases: multiple sclerosis, post-traumatic encephalopathy, epilepsy, Parkinson’s disease, etc. [4]. C. Krauthammer and G. Klerman [5] proposed in 1978 the concept of secondary mania associated with organic brain damage and its diagnostic criteria.
Diagnostic criteria for secondary mania according to C. Krauthammer and G. Klerman: a) duration of symptoms for at least 1 week; b) elevated and irritable mood; c) 2 of the following symptoms are present: d) hyperactivity, increased talkativeness, rapid train of thought, ideas of grandeur, decreased need for sleep, distractibility, reckless behavior; absence of a history of manic, depressive or other affective disorders, as well as symptoms of confusion (for example, delirium) accompanying mania.
D. Steffens and K. Krishnan [6] proposed a definition of post-stroke or vascular mania. It is a mania that develops in the presence of clinical (history of stroke or transient ischemic attack (TIA) and/or symptoms of focal brain injury), neuroimaging (altered white matter signal, cortical or subcortical infarcts) or neuropsychological (cognitive deficits in form of decreased regulatory functions, memory and speed of mental operations) symptoms. Additional criteria include onset at the age of 50 years and older, the absence of affective disorders in the family history and the presence of severe disability [6]. Later, C. Wijeratne and G. Malhi [7] revised this definition. Vascular mania is a form of mania that begins in patients 50 years of age or older, after an acute cerebrovascular accident (TIA or stroke) or with at least two vascular risk factors (arterial hypertension, hyperlipidemia, coronary heart disease, diabetes mellitus), and also with additional criteria, including changes according to neuroimaging and neuropsychological studies that go beyond the age norm [7].
Mania is an extremely rare manifestation of cerebral stroke. According to a meta-analysis by C. Santos et al. [8], which included 49 studies, over the past 50 years only 74 cases have been described in the world literature. R. Robinson et al. [9] purposefully examined 700 patients after a stroke and identified only 3 cases of mania; the same number of patients was noted by J. Dunne et al. [10], examining 661 patients, and L. Caeiro et al. [11] - 188 patients. In other words, in these studies, the incidence of mania after stroke ranged from 0.4 to 1.6%. In some cases, mania occurred as part of post-stroke bipolar affective disorder [12]. In terms of time, mania developed in different periods of stroke: from the most acute to 2 years after it [8].
Mania often develops as a result of right hemisphere strokes. Many authors explain this connection by damage to the frontal-subcortical loops, in particular the right orbitofrontal and limbic cortical-striato-thalamocortical loops, which are responsible for the control of the affective sphere and behavior in society, as well as motivation and spontaneity [8]. This finding is consistent with data on the high incidence of post-stroke depression, the opposite of mania, in left-hemisphere lesions [8]. However, in the literature there are reports of cases of the development of mania after strokes of various localizations [8]. It is likely that sometimes a significant role in the development of mania belongs to the phenomenon of diaschisis—a dysfunction of parts of the brain that are not directly damaged, but are connected to the affected area by a system of pathways [13].
Some authors have reported an association between the development of mania and subcortical atrophy according to neuroimaging data [14–17], genetic factors [15–17], and a history of mental illness [16, 17]. However, a meta-analysis by S. Santos et al. [8] did not confirm these data.
Functional neuroimaging methods have provided additional data on the mechanisms of development of mania after stroke. In the literature, there are two descriptions of cases of mania after right hemisphere strokes with examination data using single-photon emission computed tomography [18, 19]. Both cases demonstrated hypoperfusion in the right hemisphere and hyperperfusion in the left hemisphere, indicating an important role of interhemispheric imbalance in its development. In particular, A. Koreki et al. [19] showed that in a patient with hemorrhage in the right putamen, mania was observed against the background of hypoperfusion in the right temporal and frontal regions and hyperperfusion in the inferolateral, prefrontal regions, temporal lobe, as well as in the medial and lateral regions of the parietal lobe of the left hemisphere . A study conducted after the resolution of manic symptoms revealed a decrease in hypoperfusion in the right frontotemporal region and resolution of hyperperfusion in the structures of the left hemisphere. The authors suggested that the development of post-stroke mania in the described patient was based on the phenomenon of contralateral disinhibition [19]. In this case, it was manifested by an increase in the activity of the structures of the left hemisphere due to damage to the right, as a result of a violation of interhemispheric inhibition. In turn, increased activity of the left frontal cortex relative to the right frontal lobe was associated with the development of positive affect and an increase in motivational and motor activity and, as a consequence, symptoms of mania. Damage to the left insular cortex can lead to the development of elevated mood, thereby contributing to the development of mania. In another study, in 3 patients with mania after strokes in the right subcortical region, positron emission tomography revealed a decrease in the metabolic rate in the basal temporal lobes, probably due to the phenomenon of diaschisis. These data highlight the role of limbic system disorders in the development of mania [20].
Mania can develop after strokes in the vertebrobasilar system; there are reports of the development of mania after cerebellar strokes [21–25]. Damage to the cerebellum, along with typical motor disorders, can lead to the development of cognitive-affective syndrome, manifested by disorders of regulatory functions, visuospatial skills, speech, mood, and behavior [25]. Mania may be a rare manifestation of cerebellar cognitive-affective syndrome. The development of mania after cerebellar strokes is probably based on the disconnection of connections between the posterior lobe of the cerebellum and the associative cortex and between the posterior part of the vermis and the structures of the limbic system [26]. These data are supported by studies that revealed cerebellar atrophy in patients with mania as part of bipolar affective disorder [27].
There are reports in the literature [28, 29] of the development of manic symptoms after subarachnoid hemorrhage (SAH). In particular, L. Caiero et al. [29] conducted a neuropsychological examination of 108 patients in the acute period of SAH and found signs of mania in 2 of them. The authors found no association between the development of manic symptoms and the neuroanatomical characteristics of SAH.
Mania can develop as part of behavioral disturbances in a rare hereditary cerebrovascular disease - cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). Symptoms of mania may even be the first symptom of this disease [30].
From a clinical point of view, the symptoms of primary mania in bipolar disorder and secondary mania after a stroke are not fundamentally different [8, 17]. According to a meta-analysis [8], the most common symptoms of post-stroke mania were elevated mood (91%), pathological talkativeness (71%), decreased need for sleep (69%), and agitation (63%). A case has been described of a change in the drawing style of an artist with symptoms of mania after a stroke in the middle cerebral artery system [31]. The meta-analysis made it possible to identify the most characteristic features of patients with post-stroke mania. The typical patient was a man with no past or family history of psychiatric disorders, at least one vascular risk factor, no evidence of subcortical atrophy, and a history of right hemisphere stroke (patients with mania that developed up to 2 years after stroke were included in this analysis). A separate analysis of patients with mania that developed immediately after a stroke gave a similar result [8].
Mania after a stroke must be differentiated from disinhibition syndrome due to damage to the orbitofrontal cortex and its connections, which, in addition to elevated mood, is characterized by dysphoria, as well as severe impairment of regulatory cognitive functions. Behavioral disorders within post-stroke epilepsy may have features of mania. To exclude epilepsy as a cause of manic symptoms, a detailed medical history is important, as well as an electroencephalographic study. Mania-like symptoms may occur as part of a positive psychological response to recovery of neurological deficits. However, in such cases their severity is much less, and their duration is shorter.
Symptoms of hyperactive delirium may resemble mania, but unlike the latter, they develop more acutely, are fluctuating in nature, and are accompanied by global cognitive and behavioral impairment. Symptoms of mania and delirium may occur together. In such cases we are talking about delirious mania or Bell's mania [32]. Some authors consider delirious mania as a form of catatonic syndrome [33]. In the literature [34, 35] there are descriptions of delirious mania after an ischemic stroke in the region of the right thalamus, brainstem and cerebellum.
Patients with mania after a stroke cannot undergo full rehabilitation due to low adherence to rehabilitation treatment. Therefore, timely treatment of mania after a stroke is very important. In terms of treatment, firstly, it is necessary to exclude iatrogenic causes of mania: discontinue psychostimulant drugs (for example, stimulant antidepressants prescribed for depression), normalize the sleep-wake cycle. Secondly, choose psychopharmacotherapy. In post-stroke mania, the use of antiepileptic drugs is more preferable, while lithium preparations are undesirable due to potential side effects and a narrow therapeutic index [36]. Data on the treatment of mania after stroke were reported in 47 of 74 (64%) cases included in the systematic review by Santos et al. [8]. In 62% of cases, normothimic drugs were used (lithium drugs, carbamazepine, valproate), in 32% typical neuroleptics (haloperidol), in 19% atypical neuroleptics (olanzapine, risperidone), in 13% benzodiazepine tranquilizers (lorazepam, diazepam) [8] .
Thus, mania is a rare neuropsychiatric manifestation of stroke. Its timely diagnosis and correction are important for successful rehabilitation and require a multidisciplinary approach with the involvement of a psychiatrist/psychotherapist. Further study of cases of post-stroke mania may help to clarify the neuroanatomical substrate for the development of this syndrome in bipolar disorder and other mental illnesses.
Post-stroke anxiety conditions
Post-stroke anxiety is determined with a frequency of 5 to 15%. At the same time, in countries with insufficient quality of medical care, a constant feeling of anxiety is present in 25% of patients, while in 20% of stroke survivors, a generalized anxiety disorder develops and progresses. In most cases, post-stroke anxiety is a companion to clinical depression. Although an abnormal level of anxiety in itself does not lead to a deterioration in cognitive potential, constant insurmountable anxiety does not allow the patient to adapt normally to functioning in society and significantly worsens the quality of life.
All-consuming anxiety negatively affects a person’s character and his style of interaction with society. A patient with an anxiety disorder becomes nervous and irritable, losing his temper for no reason. Due to constant nervous tension, he conflicts and gets into arguments with others. It is difficult for him to organize his day and bring the work he has begun to its logical conclusion. The slightest obstacles and everyday difficulties lead him into a state of panic.
Since the patient's thinking is overwhelmed by anxious thoughts, he cannot concentrate on the task at hand. Because of this, the quality of performance of his professional duties suffers. A decrease in the ability to concentrate and maintain attention is also due to “chewing mental cud.”
Irrational anxiety negatively affects sleep patterns and quality. Common problems of a patient with an anxiety disorder are persistent insomnia, nightmares, and frequent waking up in the middle of the night. Such phenomena lead to the fact that in the morning a person feels overwhelmed and exhausted.
It should be remembered that no pharmacological products can completely eliminate pathological anxiety, since they only work to relieve the symptoms of the disorder. You can only get rid of abnormal anxiety through psychotherapy. The main task of the psychotherapist is to convey to the client true information about what causes his anxious state, teach him ways to manage his thinking and behavior, and motivate him to replace dysfunctional thoughts with constructive ideas.
Symptoms
Delirium after a stroke can develop not only suddenly, but also have precursors. Character traits appear that were not characteristic before:
- unmotivated aggression,
- constant comments and reproaches to others,
- difficulties with work,
- "complex nature.
After some time, a sharp deterioration occurs. In this case, both inhibition and agitation of the psyche are observed.
There are hyper- and hypoactive forms. With hypoactive confusion, patients appear inhibited, detached, even stunned. They do not pay attention to the interlocutor, their speech is scanty, their phrases are confused and meaningless. Such people do not remember past and present events, they soon get tired, and their activities proceed at a slow pace. Usually there is increased sleepiness during the day, often with mental agitation in the evening.
In the hyperactive form of post-stroke psychosis, the person is fussy and can even destroy everything around him. When on bed rest, he constantly tosses and turns, changes positions, and fidgets with the blanket. Motor excitement is combined with speech - there is loud shouting of words, “verbal nonsense.” All this is accompanied by aggressiveness, excessive fun, and anxiety. Symptoms tend to worsen at night.
The duration of delirium is influenced by the following factors:
- localization and size of the brain lesion,
- general exhaustion,
- accompanying illnesses.
The flow is wavy, with relatively light intervals, when self-criticism and bright consciousness appear. The duration of the acute period usually does not exceed 7 days.
After a stroke, a person’s life suffers on all fronts, not only in terms of physical health. Social significance of post-stroke changes:
- Decreased performance and everyday adaptation.
- Reduced life expectancy.
- Decreased quality of life, material and financial condition of the patient and his loved ones.
Therefore, watch for changes in the character of a person who has had a stroke. It is always better to prevent a disease than to treat it. Early screening for mental disorders is carried out using simple neuropsychological techniques. When significant changes are identified, it is important to act on them immediately.
Post-stroke aggression and rage
In the acute and subacute phase of stroke, patients often experience causeless, uncontrollable aggression, outwardly expressed by an angry attitude towards others and the commission of violent acts. This phenomenon is described by doctors as post-stroke rage. The prevalence of this problem reaches 35% of cases in the acute stage of stroke. As the crisis subsides, the level of aggression and rage decreases.
The mechanism of development of post-stroke rage has been well studied. It has been established that such a psychoemotional disorder is often associated with damage to the ventral prefrontal cortex of the brain.
A stroke survivor may exhibit different types of aggressive reactions. The most common forms are:
- physical aggression, which involves using physical force to attack another person;
- indirect aggression, which means humiliation of another person through slander, gossip, and malicious statements;
- explosions of rage that do not have a specific addressee (stomping feet, banging fists on the table, breaking dishes, slamming doors);
- verbal aggression - demonstration of one’s feelings through screams, threats, curses;
- passive or active negativism – actions aimed at undermining the authority of medical personnel.
Any manifestations of aggressive behavior require immediate consultation with a psychotherapist and corrective work.
Manifestations of aggression in post-stroke psychosis
Aggression after a stroke has a number of features. Usually, when inappropriate behavior develops, the patient is dangerous to himself and others. The aggressive state does not develop immediately, but gradually, over two or three months. It is characterized by the following:
- self-criticism disappears;
- the patient withdraws into his thoughts and withdraws from everyone;
- intense psycho-emotional background;
- slurred speech;
- interest in surrounding things and people disappears;
- inappropriate behavior, especially at night;
- weight loss.
In a person who has suffered a stroke, aggression is often accompanied by a depressive state. Aggression is characterized by attacks. Most often it appears at night. Emotional instability leads to increased vulnerability of the patient, and this, in turn, causes him an inferiority complex. A vicious circle arises. Relatives observe with horror that a loved one has become different, distant and aggressive.
Anosognosia
Another consequence of a stroke is anosognosia, characterized by a lack of critical assessment of health status and denial of an existing defect. The patient can claim that he does not have paralysis, his vision, hearing and speech are normal, and his mental sphere is absolutely healthy. For example, a paralyzed patient can tell the doctor how he moved, lifted, and controlled his injured arm.
In most cases, anosognosia is a consequence of damage to the right parietal lobe of the brain. This phenomenon is considered in psychology as “denial,” that is, a person’s desire to avoid accepting truthful information about himself that is incompatible with existing ideas about his own body and spiritual world.
Denial is a deterrent that allows you to unconsciously reduce disturbing experiences. The development scheme of anosognosia can be presented as follows: distorted perception of real factors - the need to eliminate psycho-emotional stress - the inclusion of psychological defense mechanisms. This protective behavior helps the patient feel included in social activities.
However, anosognosia acts as a significant obstacle to treatment, becoming a kind of “counterweight”. The psychologist has to make considerable efforts to rid the patient of illusions and return him to reality.
Therapeutic approaches in the treatment of psychoemotional disorders
The following therapeutic approaches have proven themselves well in the treatment of psychoemotional disorders initiated by acute cerebrovascular accident.
Brief Solution Focused Therapy (BSFT)
The fundamental difference between this direction and other psychotherapeutic methods is not only the short duration of treatment (1-3 sessions), but also the focus on solving the problem. The psychotherapist's efforts are always aimed at the main goal that the client has set for himself. The specialist’s task is not to focus on problems, but to actualize and stimulate a person’s existing potential, to identify and develop existing abilities.
Problem-Solving Therapy (PST)
This short-term method (4-8 sessions) aims to reduce the severity of depression and anxiety disorders by recognizing the relationship between the symptoms demonstrated and existing problems in the person's life. Problems are identified during an unobtrusive conversation. The psychotherapist’s task is to teach the client to develop a systematic, structured approach to overcome life’s obstacles.
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy focuses on exploring the relationships between an individual's thoughts, experiences, and behavior. By exploring destructive thought patterns that contribute to self-destructive actions and stereotypical beliefs that drive a person's behavior, the therapist motivates the client to replace them with functional ideas.
Acceptance and Commitment Therapy (ACT)
This method teaches stroke survivors to simply “notice,” accept, and take personal responsibility for thoughts, experiences, sensations, memories, and events that occur. Instead of trying to take undesirable phenomena under control, the psychologist invites the client to give up the meaningless struggle with reality and recognize the right to be as he is.
Interpersonal Psychotherapy (IPT)
The direction is based on the working principle of “here and now” and focuses on interpersonal relationships. A therapist helps improve the way a depressed person communicates. The technique allows the client to identify their emotions and their sources, express feelings in a healthy way and eliminate negative emotional baggage from the past.
Mindfulness-based Cognitive Therapy (MCT)
Mindfulness-based cognitive therapy helps those who suffer from recurrent bouts of depression and chronic unhappiness. The method combined the ideas of cognitive therapy with meditative practices and attitudes based on the cultivation of mindfulness. The main idea of the method is based on the assumption that depressive mood and negative catastrophizing self-devaluing thinking form an associative connection.