The mediator acetylcholine: why do humans and other living beings need it? How are acetylcholine and nicotine related? Where is acetylcholine produced and how does it work?
Acetylcholine is one of the main neurotransmitters in the nervous system. But there is very little information about the mediator acetylcholine, written in understandable language. Wikipedia and other sources talk about neurotransmitters with many complex terms that are difficult to understand the first time. In this article we will try to talk about acetylcholine in simple and understandable language.
What are neurotransmitters anyway? Neurotransmitters are chemicals that carry information in the human nervous system. That is, information between nerve structures, in this case, is transmitted not using an electrical impulse, but precisely thanks to special molecules that float in the intercellular fluid. These molecules are called mediators.
We need to immediately tell you about the most important properties of acetylcholine for humans. It directly affects memory and academic performance. The higher the acetylcholine level, the higher they are. And the second important function of the mediator is the process of falling asleep. We fall asleep when we have very little acetylcholine. If you can't sleep, you probably have high acetylcholine levels. This may be due to the fact that you moved a lot or worked at all. We'll tell you why below.
Acetylcholine molecule
Discovery of the neurotransmitter acetylcholine
Acetylcholine was the first neurotransmitter discovered by scientists. And this was done by the German pharmacologist Otto Lewy. In his amazing experiment, acetylcholine stopped a frog's heart.
- Experiment with the neurotransmitter acetylcholine and frog hearts
The scientist took two frog hearts and immersed them in saline solution. And the peculiarity of the frog’s heart is that they can beat for a very long time in a special physiological solution. Then he began to irritate the vagus nerve, which came out of one of the hearts, with an electric current. The heart slowed down its rhythm (this is how it should happen).
After this, the scientist collected some liquid near the heart into a syringe and poured this liquid into the vessel where the second heart was beating. The second heart also slowed down its rhythm.
Otto Lewy's experiment
For the discovery of acetylcholine, and with it neurotransmitters in general, Levy was awarded the Nobel Prize. They say that he dreamed about the experience with frogs at night. Moreover, the dream was repeated twice; the first time the scientist did not understand what he was dreaming about.
Reasons for the shortage
Levels of this neurotransmitter tend to decline with age. The memory loss that we think of as part of age-related cognitive decline is often caused by this decline. Also, a low level can be for several other reasons:
- Antibodies against acetylcholine receptors, in the case of myasthenia gravis [];
- Insulin resistance and diabetes interfere with acetylcholine synthesis [];
- Low fat diets;
- Medicines (anticholinergic drugs).
Acetylcholine and nicotine
The neurotransmitter acetylcholine is important in the sense that it is its molecule that nicotine copies. In general, almost all drugs are similar in molecular structure to different neurotransmitters.
- Nicotine replaces acetylcholine.
- Opium and heroin copy another neurotransmitter - dopamine, which is also called the “happiness hormone”.
- Ecstasy replaces serotonin, one of the pleasure hormones.
- Alcohol does not replace any mediator with its molecule, but its effect on metabolic processes in the brain is very strong. Alcohol increases dopamine levels, although not as much as opium. Alcohol also complicates the functioning of GABA, a neurotransmitter that is responsible for calmness, concentration and learning. That is, alcohol “turns off the brain” and affects two systems of mediators at once.
There is a drug that blocks cravings for nicotine - Tabex with the active substance cytisine. There is also a more modern drug, Champix, with the active ingredient varenicline. The molecules of these substances connect to acetylcholine receptors in those places where acetylcholine is attached in healthy people or nicotine in smokers. As a result, the craving for nicotine disappears. However, medications are not necessary for those who want to quit smoking; the human body has everything to cope with this problem on its own.
In addition to smoking, there is also chewing, snuff and even sucking tobacco. Nicotine can be absorbed through the skin. This is the basis of the action of nicotine patches. There is also nicotine spray and chewing gum.
The acetylcholine molecule is copied not only by nicotine from tobacco. For example, agonist substances or “substitutes” for acetylcholine are also found in belladonna and dope. The effect of these plants on the human body is even more destructive than that of tobacco.
Datura can cause hallucinations, tachycardia, and photophobia.
But any poison in small dosages becomes a medicine, and preparations from dope and belladonna are used to relieve pain, spasms, to test vision and for some other purposes. For example, the main purpose of the drug Bellastesin is pain relief for stomach ulcers. But you should still be extremely careful with such medications and try to avoid them. In addition to many side effects, they cause persistent addiction.
A drug that duplicates acetylcholine
In general, nicotine and similar substances in plants are toxins. Plants use them as a nerve poison against beetles and other pests that want to feast on them. Nicotine acts like a deadly poison on insects; they are smaller and more vulnerable than humans. Even ripe tomatoes contain small amounts of nicotine; there is a little more of it in tomato leaves and potato leaves. To prevent insects from attacking your garden plants, you can use powdered tobacco. It is also used as a fertilizer.
O.A. Gromova1,2, K.V. Rudakov1,2, I.Yu. Torshin1,2
1Russian Satellite Center of the UNESCO Institute of Microelements, Moscow
2Laboratory of Computational and Systems Biology of the Computer Center named after. A.A. Dorodnitsyna, RAS, Moscow
Key words: choline, cellular biochemistry, physiological effects.
Choline is one of the vitamin-like substances. The biological effects of choline are most important in the neuromuscular system, where choline is a precursor to acetylcholine, an essential neurotransmitter. Choline is also necessary for regulating the mechanical properties of cell membranes and is a donor of methyl groups for the synthesis of S-adenosylmethionine. The above-mentioned cellular and biochemical effects of choline correspond to the spectrum of physiological effects of this substance. It should be noted that until now, the reliable range of physiological effects of choline has not been systematically analyzed based on objective data. The latter leads to unfounded speculation in order to promote choline drugs and an extreme exaggeration of the therapeutic significance of cholinergic drugs. In this work, we aim to determine the spectrum of physiological effects of choline based on data from basic medicine. Knowledge of the reliable spectrum of choline allows us to objectively assess the real applicability of choline drugs in various fields of medicine, including neurology. The results of the analysis are compared with available data on evidence-based medicine in order to indicate the real possibilities of choline drugs when used as part of personalized medicine. Introduction The creation and correct use of highly effective neuroprotective drugs of artificial and natural origin is the most important task in modern medicine. In Russia alone, the incidence of stroke is about half a million cases per year, which makes it necessary to develop effective therapeutic protocols based on individual drugs. Adequate implementation of protocols should be carried out within the framework of personalized medicine, i.e., take into account the individual characteristics of each patient. Known neuroprotective drugs differ in the range of their physiological effects on the body. There are drugs with an extremely wide spectrum of effects (for example, Cerebrolysin, which has a positive effect on dozens of physiological mechanisms [1]). There are also drugs with an extremely narrow spectrum of action (for example, thrombolytics, which act exclusively on hemostasis). Other drugs act on several specific physiological subsystems of the body. The intensity and versatility of these effects ultimately determine the degree of therapeutic effectiveness of the drugs. Choline, phosphatidylcholine, CDP-choline and other choline derivatives are well-known dietary supplements that are widely used in healthy eating schools (see, for example, [2]). The subject of this article is to analyze the spectrum of all possible physiological effects of choline-based drugs. It is obvious that the establishment of this spectrum based on data from fundamental medicine, clinical studies and post-genomic biology will allow us to establish the real area of therapeutic applicability of this group of drugs. The analysis in this work was carried out using a search of public databases (including the human genome databases at www.genome.gov, ncbi.nlm.nih.gov) and the existing literature on basic medicine and clinical research. The need for choline, its availability in foods, the fundamental physiological mechanisms of choline and its derivatives, and clinical research data are reviewed in sequence.
Choline: its sources and dietary choline deficiency Choline (vitamin B4, Fig. 1) is part of lecithin, plays a role in the synthesis and metabolism of phospholipids in the liver, and is a precursor of the neurotransmitter acetylcholine. Choline is widely distributed in commonly used foods in the form of free choline; in animal sources and in soy as an integral part of the lecithin molecule. Main food sources of choline: eggs, liver, lean meat, fish, soybeans, oatmeal, cauliflower, spinach, cabbage, peanuts. It is a component of lecithin. The choline content of various foods is shown in Table 1. A typical diet contains 500-900 mg of choline. According to recommendations adopted in Russia, an adult’s need for choline is 500-1500 mg/day. The upper permissible level of consumption: 1000-2000 mg/day for children under 14 years of age, 3000-3500 mg/day for children over 14 years of age and adults [3]. Choline deficiency can only occur in extreme situations (chronic alcoholism, genetic defects), since choline is present in a large number of foods. Moreover, the human body can synthesize choline from other dietary components in the absence of choline in the diet. Choline deficiency (unlike, for example, magnesium or pyridoxine deficiency) is not a nosology according to ICD due to the rather low specificity of symptoms. With proven choline deficiency, the following disorders develop: fat intolerance (diarrhea and flatulence when eating fat), hypertension, impaired growth, stomach ulcers, changes in heart rate, failure of liver and kidney function. An upper permissible level of consumption has been established for choline (3000-3500 mg/day in Russia, Methodological recommendations of the Ministry of Health of the Russian Federation [3]). Large doses of choline (grams) lead to increased sweating, nausea, and a strong fishy odor of the skin. In the group of stroke patients taking 2000 mg/day, cases of headache and dizziness were more common [4]. Manufacturers of neurological choline drugs (citicoline) indicate side effects in the form of allergic reactions (rash, skin itching, etc.), and the development of shock is possible. Contraindications to the use of choline drugs are vagotonia (predominance of the tone of the parasympathetic part of the autonomic nervous system) and hypersensitivity to the drug. Again, in accordance with the manufacturers' recommendations, use in children under 18 years of age is not recommended (due to lack of data), and during pregnancy the drug is prescribed only if the expected benefit outweighs the potential risk.
Fundamental Mechanisms of Choline's Effect on Physiology From a basic medical point of view, choline and its metabolites are essential for three physiological processes (Fig. 2): maintaining the structural stability of membranes, cholinergic neurotransmission (via the synthesis of acetylcholine) and participation in DNA methylation through the choline derivative trimethylglycine (betaine). ). Based on betaine, a source of methyl groups, the S-adenosylmethionine molecule, is synthesized. Phosphatidylcholine (the main component of lecithin) is one of the phospholipids that form the cell membrane. Phospholipids, in addition to forming the cell membrane, also serve as intermediates in cell signaling systems. Released from the cell membrane by phospholipases, phospholipids participate in the arachidonic acid cascade that mediates proinflammatory responses. Phospholipase D catalyzes the hydrolysis of phosphatidylcholine to form phosphatidic acid and, again, choline, which is secreted into the cytosol. Signal transmission through phosphatidylcholine is an integral part of many molecular mechanisms of the cell (for example, signal transmission from the “cell colony stimulating factor” protein, which ultimately leads to an increase in the leukocyte population [5, 6]. Signaling through phosphatidylcholine cascades is what is associated likely to increase apoptosis of cells (e.g. lymphocytes [5]). Acetylcholine is a neurotransmitter in both the peripheral and central nervous systems. In the peripheral nervous system, acetylcholine activates muscle cells. In the central nervous system, acetylcholine forms the cholinergic system, including numerous types of acetylcholine receptors and enzymes catabolizing this neurotransmitter. Activation of the cholinergic system, in general, has an excitatory rather than inhibitory effect on the neuromuscular system [7, 8]. When acetylcholine interacts with the ACh receptors of skeletal muscles, sodium ion channels open, sodium enters the cell and stimulates contraction In the case of the myocardium, acetylcholine has the opposite effect - it reduces the contractility of cardiomyocytes. In the CNS, acetylcholine serves as a neuromodulator of synaptic function, and profound acetylcholine deficiency is associated with memory impairment in Alzheimer's disease [7]. The physiological effects of acetylcholine significantly depend on the localization of receptors in certain tissues and organs (Table 2) and can be very important when analyzing a patient in the context of personalized medicine (see below). There are two main classes of acetylcholine receptors: nicotinic and muscarinic. The names of the receptors are related to the ligands that activate these receptors. Nicotinic receptors are located on muscle cells in the central nervous system and change the permeability of the membrane to sodium, potassium and chloride ions. Muscarinic receptors are located in the central nervous system and periphery, also in the myocardium, lungs, upper gastrointestinal tract and sweat glands. Muscarinic acetylcholine receptors do not change the ionic conductivity of membranes, but initiate intracellular signal transmission through G proteins [9]. Acetylcholine and choline increase plasma nitric oxide and red blood cell nitrite levels. A possible mechanism is activation of M1 muscarinic acetylcholine receptors [10, 11]. Increased NO concentration leads to vasodilation. Nitric oxide is also the most likely mechanism for the disaggregant action of choline [12], and a decrease in red blood cell aggregation also contributes to a decrease in blood clotting [11]. Based on one of the choline derivatives, betaine, the molecule S-adenosylmethionine is synthesized, a component of cellular biochemistry important for maintaining the structure of the genome. S-adenosylmethionine is an intermediate product of the transformation of the amino acid methionine, which comes with excess protein foods (meat, cottage cheese, eggs). The methionine transformation cycle includes homocysteine, methionine, S-adenosylmethionine and S-adenosylhomocysteine (Fig. 3). Homocysteine, an independent factor of atherosclerosis and stroke, significantly aggravates the rehabilitation of patients. Along with folate, vitamins B12 and B6, S-adenosylmethionine is involved in the neutralization of homocysteine (Fig. 4). However, unlike the detoxification of homocysteine in the folate cascade, the transformation of homocysteine and methionine through S-adenosylmethionine can lead to:
1) increased DNA methylation due to higher levels of S-adenosylmethionine and 2) increased levels of catecholamines.
Excess choline can therefore negatively affect genome structure due to increased methylation. It should also be noted that cancer cells contain elevated levels of choline, which is apparently associated precisely with disorders of phospholipid metabolism characteristic of oncology [13]. Increased choline levels correspond to increased DNA methylation (due to increased levels of S-adenosylmethionine) and, therefore, worsening cancer-related chromosomal abnormalities. One of the interesting physiological effects of choline on cellular biochemistry is also its effect on catecholamine levels. Experiments on cells in culture have shown that choline stimulates the secretion of catecholamines (adrenaline, in particular) [14, 15]. Catecholamines are also dependent on S-adenosylmethionine levels [16] and are one of the main regulators of vasoconstriction. CDP-choline (cytidyl diphosphocholine, the basis of such drugs as citicoline, etc.) leads to an increase in plasma catecholamines [17]. Higher levels of catecholamines are associated with increased blood pressure and thus are not always beneficial for stroke and other diseases. Intraperitoneal administration of CDP-choline actually leads to an increase in blood pressure in the experiment [17]. The above-mentioned mechanisms of choline action are also confirmed from a post-genomic point of view, including data on all known genes through functional connectivity analysis [16]. In general, more than 40 proteins, encoded by approximately the same number of genes, interact with choline in the human body. The three pathways discussed above for the physiological effects of choline (phosphatidylcholine, acetylcholine, S-adenosylmethionine) are displayed in Table 3. The biological functions of these proteins clarify the range of influence of acetylcholine on human physiology. In particular, genome-wide analysis data made it possible to identify the main proteins involved in metabolism, choline transport and the functioning of the cholinergic receptor system. Numerous genetic defects (so-called “rare mutations”) of each of these genes will lead to certain biochemical and corresponding clinical manifestations. For example, loss-of-function mutations in choline metabolism proteins result in decreased choline requirements in a given patient. Conversely, mutations of these genes leading to increased function of the corresponding proteins lead to an increased need for choline.
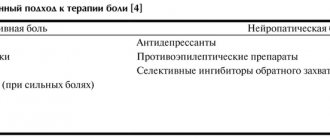
Clinical studies of choline drugs Analysis of data from cell biology and basic medicine indicates that one of the main effects of choline drugs is the effect on cholinergic neurotransmission, which leads to optimization of nerve and neuromuscular conduction. A side effect of this is to slow down the processes of apoptosis in brain tissue. Both of these effects of choline may be important in post-stroke nerve tissue repair. Accordingly, clinical studies of choline drugs, such as citicoline and others, are aimed specifically at recovery after stroke. A meta-analysis of studies on oral administration, for example, cytidyl-diphosphocholine, showed some positive and short-term effect of taking the drug on the functioning of patients' memory [18]. A meta-analysis of 10 studies on citicoline (2,279 patients) indicated a decrease in the incidence of mortality and complications in the group taking the drug [19]. A meta-analysis of studies of 1,372 patients showed a small but statistically significant difference in the rate of recovery of patients (mRS, BI, and NIHSS) treated with oral cytidyl diphosphocholine for 3 months (odds ratio 1.33; 95% confidence interval 1.1 -1.6; p = 0.003) [20] when using drug doses of at least 2000 mg/day. Individual randomized trials of the effects of choline preparations vary in their quality and degree of reliability of the results. A study of the effect of citicoline on the volume of cerebral infarction in 100 patients in the acute period of ischemic stroke based on magnetic resonance imaging showed a significant decrease in the growth of the ischemic lesion in the group of patients receiving 500 mg/day of citicoline for 6 weeks [21]. In a multicenter, double-blind, placebo-controlled study of citicoline in 272 patients with moderate to severe stroke, 133 patients received 1000 mg/day IV citicoline daily for 14 days [22]. By day 14 there was a significant improvement in the citicoline group only in the case of cognitive functions. The result suggests that IV administration of citicoline during the acute period of stroke may promote functional recovery after reversible tissue damage. At the same time, a relatively large multicenter study of 899 patients with acute stroke in the middle cerebral artery showed extremely contradictory results [4]. Thus, taking citicoline at a dose of 2000 mg/day for 6 weeks contributed to a twofold change in the Barthel index compared to the group of patients taking placebo. The same was observed when taking a dose of 500 mg/day. Paradoxically, however, the results in patients taking citicoline 1000 mg/day were comparable to the group of patients taking placebo (Fig. 5). Moreover, although there was a significantly higher proportion of patients in the citicoline group who showed improvement after 6 weeks of therapy, there was no improvement when compared at week 12 of the study. This kind of inconsistency in one of the largest randomized trials of choline drugs for stroke, along with the results of meta-analyses, shows that the use of citicoline has a fairly small effect on improving outcomes in patients with acute ischemic stroke - the main area of use of choline drugs/dietary supplements. The contradictions do not necessarily indicate poor quality of research, but rather are a consequence of neglecting to stratify patients according to blood choline levels and choline depot status. Neglect of stratified data analysis is one of the grossest and most common violations of the analysis of biomedical research results [23]. The relatively small magnitude of the observed therapeutic effect, along with the rather narrow window of physiological effect (acetylcholine-dependent neurotransmission) and the lack of stratification of the data, indicates the possibility that the beneficial effect is observed in only a small number of patients in the studied samples. For example, in a meta-analysis of 1,372 patients, the odds ratio was only 1.33 [20] with p = 0.003, corresponding to no more than a 33% chance of improvement compared with the placebo group. Our analysis of the distribution of c2 at p = 0.003 and other statistical parameters of the studies indicated in [20] confirms this assumption. Data analysis was carried out based on the deletion methodology for analyzing medical data [16]. Thus, obtaining an odds ratio of 1.33 at p = 0.003 becomes possible even with a difference in the number of respondents of 50 people between the control groups and patients taking the drug. Taking into account the large size of both groups (about 500-700 people), it becomes clear that the positive effects of choline drugs are observed in no more than 10% of patients taking the drug.
Choline preparations and personalized medicine Personalized medicine requires maximum consideration of the individual metabolic characteristics of a particular patient and, above all, the individual pharmacokinetics and pharmacogenetics of specific pharmaceuticals. A personalized approach allows you to assess the balance between the effectiveness and side effects of using pharmaceuticals in each individual case. The above analysis of the biological effects of choline indicates certain limitations associated with the use of choline drugs in specific patients. Efficiency. The above-mentioned analysis of trials of choline drugs showed that the effects of choline drugs were observed in no more than 10% of patients taking the drug. It can be assumed that these are patients with severe choline deficiency. Consequently, choline preparations will not be effective in patients with normal choline levels (which is the majority, including, especially, young hypertensive patients), even when using high doses of drugs. The effect of choline on vasodilation is controversial. On the one hand, studies on human cell cultures have shown an increase in nitric oxide when treated with choline and acetylcholine [10, 11]. Increased NO concentration corresponds to vasodilation. At the same time, the experiment established the vasoconstrictor and hypertonic effects of choline drugs when administered intraperitoneally [17]. The antithrombotic effect of choline drugs is observed at very high doses (250 mg/kg in the experiment) [12], which corresponds to taking 10-15 g/day in the case of adult patients. Such high doses (exceeding the maximum permissible by 4-5 times), along with a possible hypertensive effect, raise the question of the safety of using choline drugs (Fig. 6). Choline is required for acetylcholine synthesis [24] and administration of choline supplements, especially in hyperdoses, can increase systemic acetylcholine levels. When prescribing choline preparations, the doctor must take into account the individual pharmacology of acetylcholine. Classical pharmacology indicates different effects of acetylcholine on different organs (see Table 2). As the following examples illustrate, these pharmacological data can be effectively used in personalized medicine.
• For example, in an elderly patient with bradycardia and sufficient choline intake, supplemental choline supplementation may cause a further slowing of the rhythm. • In a patient with bronchial asthma and sufficient choline intake, taking choline supplements increases the risk of bronchospasm. • In a patient with any genetic defect of the “slow metabolizer” type in the genes serving choline metabolism (see Table 3), excessive administration of choline preparations will lead to an increased load on the elimination system and the appearance of the smell of decomposing fish in the patient. • In a patient with cholelithiasis and the presence of calcified gallstones, the use of choline preparations stimulates the tone of the wall of the gallbladder, bile ducts and can cause dangerous movement of gallstones and obstruction of the bile ducts.
Safety. According to the manufacturers, contraindications to the use of choline drugs are vagotonia, hypersensitivity to the drug; use in children under 18 years of age and during pregnancy is not recommended without assessing the risk-benefit balance. At high doses of choline (such as 2000 mg/day), headaches were more common [4]. The antiplatelet effect of choline preparations should be taken into account [12]. In particular, the decrease in red blood cell aggregation observed when taking choline helps reduce blood clotting [11]. Therefore, the use of choline drugs cannot be recommended for hemorrhagic stroke (and in the early period of ischemic stroke), when thrombolytics and antiplatelet agents can do more harm than good. Progressive manufacturers of choline drugs (Somazina, manufactured by Ferrer Internacional, Spain, https://www.ferrergrupo.com) indicate that for persistent intracranial bleeding, it is recommended to administer the drug as a very slow IV infusion (30 drops/min) and not exceed the daily dose of 1000 mg. Excess choline can lead to “fishy odor syndrome” due to the degradation of choline into trimethylamine. The fishy smell of trimethylamine is a sign of choline intoxication and the inability of elimination systems (the liver, first of all) to cope with excess choline intake. Intoxication will be significantly worsened in patients with kidney disease due to prolonged half-life, which should be taken into account in personalized medicine. As both clinical and basic research show, choline preparations are most effective in fairly high doses (grams). One of the most commonly used forms of choline, CDP-choline (citicoline, etc.) is also a significant source of phosphorus. Taking into account the excess phosphorus in the diet of Russians [25] due to excessive consumption of processed meat products (sausages, sausages, etc.), large doses of CDP-choline will only contribute to hyperphosphatemia and create additional stress on the excretory systems. Hyperphosphatemia contributes to an imbalance of macro- and microelements (primarily calcium and magnesium); prolonged hyperphosphatemia contributes to the development of oncology. High levels of phosphorus can also significantly accelerate the formation of kidney stones [26] and possibly gallstones [27].
Conclusion Choline is the basis for the synthesis of the neurotransmitter acetylcholine and one of the most popular dietary supplements. Drugs based on choline derivatives are being promoted for the treatment of stroke, in intensive care and obstetrics. However, both the evidence and the fundamental basis for the use of choline and its derivatives do not provide sufficient justification for the persistent widespread imposition of the use of choline drugs on all patients. In this work, we examined the spectrum of physiological manifestations of the effects of choline. From a neurochemical point of view, choline and drugs based on it are characterized by unidirectional effects (acetylcholine-dependent neurotransmission). In general, stroke involves disruption of multiple neurotransmission pathways (GABA, glutamate, catecholamines, NO, neuropeptides, endocannabinoids, eicosanoids, etc.), not to mention specific neurotrophic factors and interleukins. The effects of other neurotransmitters occur largely independently of acetylcholine. Analysis of evidence-based medicine indicates a high probability that choline-based drugs have a significant effect only in a relatively small proportion of patients (less than 10% of all patients). These patients may, for example, have genetic defects in choline metabolism, characterized by severe choline deficiency, or due to alcoholism or inadequate nutrition. Thus, the prescription of choline drugs requires a physician to assess the appropriateness of using drugs from this group in a given patient and a reasonable assessment of the “efficacy-safety” balance. Pharmacological neuroprotection is only part of a comprehensive program for patient recovery after a stroke. The greatest effectiveness of medications is manifested precisely in the context of comprehensive programs, including motor rehabilitation, physical therapy, classes with a speech therapist, swimming, massage, programmable electrical myostimulation, correction of walking patterns, etc. Prevention of recurrent stroke is very important, which must necessarily include lipid profile correctors and coagulation (aspirin, omega-3 PUFAs, selenium-containing, magnesium-containing drugs and an antiatherogenic diet).
Literature 1. Gromova O.A., Gupalo E.M., Torshin I.Yu. Cerebrolysin: analysis of basic and clinical studies. Methodological letter for doctors. M.: 2008; RSC Institute of Microelements UNESCO, 142. 2. Atkins R. Bioadditives of Dr. Atkins, RIPOL Classic. M.: 1999; 81. M.: 2008; 33. 3. Methodological recommendations of the Research Institute of Nutrition of the Russian Academy of Medical Sciences. Recommended standards for consumption of food and biologically active substances. Project. 2008; MP 2.3.1.1915-04, 39. 4. Clark WM, Warach SJ, Pettigrew LC, Gammans RE et al. A randomized dose-response trial of citicoline in acute ischemic stroke patients. Citicoline Stroke Study Group // Neurology. 1997 Sep; 49: 3: 671-8. 5. da Costa KA, Niculescu MD, Craciunescu CN, Fischer LM, Zeisel SH Choline deficiency increases lymphocyte apoptosis and DNA damage in humans // Am J Clin Nutr. July 2006; 84:1:88-94. 6. Jackowski S., Xu XX, Rock CO Phosphatidylcholine signaling in response to CSF-1 // Mol Reprod Dev. Jan 1997; 46:1:24-30. 7. Katzung, B. G. (2003). Basic and Clinical Pharmacology (9th ed.). McGraw-Hill Medical. ISBN 0-07-141092-9. 8. Kharkevich D.A. Pharmacology. GeotarMed, 2008; 113. 9. Hasselmo ME Neuromodulation and cortical function: modeling the physiological basis of behavior // Behav Brain Res. 1995; 67:1:1-27. 10. Carvalho FA, Mesquita R, Martins-Silva J, Saldanha C. Acetylcholine and choline effects on erythrocyte nitrite and nitrate levels // J Appl Toxicol. 2004; 24: 6: 419-427. 11. Santos T., Mesquita R., Martins E. Silva J., Saldanha C. Effects of choline on hemorheological properties and NO metabolism of human erythrocytes // Clin Hemorheol Microcirc. 2003; 29:1:41-51. 12. Masi I., Giani E., Galli C. Effects of CDP-choline on platelet aggregation and the antiaggregatory activity of arterial wall in the rat // Pharmacol Res Commun. 1986; 18: 3: 273-281. 13. Ackerstaff E., Pflug BR, Nelson JB, Bhujwalla ZM Detection of increased choline compounds with proton nuclear magnetic resonance spectroscopy subsequent to malignant transformation of human prostatic epithelial cells // Cancer Res. 2001; 61:9:3599-3603. 14. Wurtman RJ Stimulation of catecholamine secretion by choline // Science. 1983; 222: 4620: 188. 15. Holz RW, Senter RA Choline stimulates nicotinic receptors on adrenal medullary chromaffin cells to induce catecholamine secretion // Science. 1981; 214: 4519: 466-468. 16. Torshin I.Yu. Bioinformatics in the post-genomic era: sensing the change from molecular genetics to personalized medicine. Nova Biomedical Books, NY, USA, 2009, In “Bioinformatics in the Post-Genomic Era” series, ISBN: 978-1-60692-217-0. 17. Cansev M., Yilmaz MS, Ilcol YO, Hamurtekin E., Ulus IH Cardiovascular effects of CDP-choline and its metabolites: involvement of peripheral autonomic nervous system // Eur J Pharmacol. 2007; 577: 1-3: 129-42 Epub 2007 Au. 18. Fioravanti M., Yanagi M. Cytidinediphosphocholine (CDP-choline) for cognitive and behavioral disturbances associated with chronic cerebral disorders in the elderly // Cochrane Database Syst Rev. 2005; 2:CD000269. 19. Saver JL Citicoline: update on a promising and widely available agent for neuroprotection and neurorepair // Rev Neurol Dis. 2008; 5:4:167-177. 20. Davalos A, Castillo J, Alvarez-Sabin J, Secades JJ et al. Oral citicoline in acute ischemic stroke: an individual patient data pooling analysis of clinical trials // Stroke. 2002; 33:12:2850-2857. 21. Warach S, Pettigrew LC, Dashe JF, Pullicino P et al. Effect of citicoline on ischemic lesions as measured by diffusion-weighted magnetic resonance imaging // Citicoline 010 Investigators. Ann Neurol. 2000;48(5):713-722. 22. Tazaki Y., Sakai F., Otomo E., Kutsuzawa T. et al. Treatment of acute cerebral infarction with a choline precursor in a multicenter double-blind placebo-controlled study // Stroke. 1988; 19:2:211-216. 23. Torshin I.Yu. Bioinformatics in the post-genomic era: physiology and medicine. Nova Biomedical Books, NY, USA (2007), ISBN: 1600217524, 35-67. 24. Freeman JJ, Jenden DJ The source of choline for acetylcholine synthesis in the brain // Life Sci. 1976; 19: 7: 949-961. 25. Tutelyan V.A., Spirichev V.B., Sukhanov B.P., Kudasheva V.A. Micronutrients in the diet of a healthy and sick person. M.: Kolos, 2002; 423. 26. Guan X., Wang L., Dosen A., Tang R. et al. An understanding of renal stone development in a mixed oxalate-phosphate system // Langmuir. 2008; 24: 14: 7058-60. 27. Wolf P., Mannino F., Hofmann AF, Nickoloff B., Edwards DK Calcium oxalate-phosphate gallstones, a unique chemical type of gallstone // Clin Chem. 1982; 28:8:1804-1805.
Where is acetylcholine produced?
Acetylcholine is produced at neuromuscular junctions near the spine. And it is produced in response to movement, in response to stress, and in general almost constantly. That is, if you decide to move your finger, then signals pass through your nerve fibers. For example, the signal passed from the finger to the spine (the axons or processes of nerve cells are sometimes really so long). In response, a nerve synapse near your spine released the neurotransmitter acetylcholine, which caused your finger to bend.
Many conclusions can be drawn from this simple description:
- The simplest conclusion is that active movements and work increase acetylcholine levels and make it difficult to fall asleep.
- Another conclusion is that acetylcholine mobilizes the body. Therefore, if you need to do important work, even mental work, then physical activity will help you.
- Interestingly, acetylcholine is produced not only when you consciously decide to move, but also in nervous and restless individuals. The more anxious a person is, the higher their acetylcholine levels.
- If you decide to quit smoking, then playing sports will make your quitting process faster, but more noticeable. What we don’t use atrophies. And a smoker produces little acetylcholine. If you move a lot, you will put a lot of stress on this system.
Creation and destruction of acetylcholine
How to Increase Acetylcholine Levels
Although acetylcholine plays a key role in many aspects of your health, there are no supplements that can directly increase your levels.
However, you can eat foods or take dietary supplements that indirectly increase the release of acetylcholine or interfere with its breakdown.
One of the easiest ways to raise acetylcholine levels is to eat foods or take supplements that are high in choline, an essential nutrient that can be converted to acetylcholine ().
Choline is present in many foods including ():
- Beef liver : 85 grams contains 65% of the recommended daily intake (RDI).
- Eggs : 1 large hard-boiled egg contains 27% of the RDI.
- Beef : 85 grams contains 21% of the RDI.
- Soybeans, roasted : 85 grams contains 19% of RDI.
- Roasted chicken breast : 85 grams contains 13% of the RDI.
- Fish, cod : 85 grams contain 13% of the RDI.
- Shiitake mushrooms, cooked : 75 grams contains 11% of the RDI.
- Canned beans : 130 grams contains 8% of the RDI.
- Quinoa, cooked : 185 grams contains 8% of the RDI.
- Milk, 1% : 1 cup (240 ml) contains 8% of the RDI.
- Vanilla yogurt, nonfat : 1 cup (245 grams) contains 7% of the RDI.
- Cooked broccoli : 80 grams contains 6% of the RDI.
- Brussels sprouts, cooked : 80 grams contains 6% of the RDI.
Dietary supplements that may increase choline levels include Alpha-GPC (L-alpha-glycerylphosphorylcholine), citicoline (CDP-choline), and choline bitartrate.
However, Alpha-GPC and citicoline generally contain more choline per unit weight and are more easily absorbed than other forms (, ).
Another way to indirectly increase acetylcholine levels is to take supplements that inhibit the enzymes that break down acetylcholine.
Here are some supplements that may inhibit the breakdown of acetylcholine (, , ):
- Ginkgo biloba (ginkgo)
- Bacopa Monnieri
- Huperzine A
However, it is unclear how effective supplements that inhibit the breakdown of acetylcholine are in increasing acetylcholine levels compared to choline supplements.
Summary:
Acetylcholine is not available as a dietary supplement, but its levels can be indirectly increased through consumption of choline, a precursor to acetylcholine, as well as supplements that inhibit the breakdown of acetylcholine.
Life cycle of acetylcholine
Let's explain some terms in the previous diagram:
Choline acetylase is an enzyme that catalyzes, that is, accelerates and enhances the reaction of the formation of acetylcholine. It is created from two substances acetic acid and choline. Scientists have not yet been able to isolate choline acetylase in its pure form. Its quantity can be judged by indirect signs: the amount of acetylcholine and the rate of its accumulation.
Vitamin B1 , also called thiamine, plays a very important role in the production of choliacetylase . Thiamine, as a medicine, is indicated for use in case of its deficiency, sometimes during pregnancy, heart failure, severe liver disease and other disorders. Thiamine supports processes associated with the functioning of insulin and stimulates the production of the mediator acetylcholine.
Thiamine is available in the form of an injection solution and in tablet form in combination with other B vitamins. These vitamins are indicated for neurological disorders, physical damage to nerve tissue, alcoholism, chemical poisoning and some other conditions.
Thiamine preparation
M and N cholinergic receptors. Receptors are structures that catch a certain substance, in our case the neurotransmitter acetylcholine. It often happens that there is only one mediator, but there are several receptors on which it affects. Acetylcholine acts on nicotinic and muscarinic receptors.
- Nicotinic receptors are found in skeletal muscles and in the autonomic ganglia. The agonist, that is, the substance that replaces acetylcholine in them, is nicotine. These receptors are completely blocked by the deadly snake venom curarine.
- Muscarinic receptors can be found in large numbers in smooth muscle and in the brain. Muscarine, the poison of fly agarics, henbane and other nightshade plants, can replace acetylcholine in them. And poisonous atropine blocks these receptors.
Cholinergic synapse[edit | edit code]
Source:
Visual Pharmacology
.
Author
: X. Lulman.
Per. with him. Ed.
: M.: Mir, 2008
Acetylcholine - Vyacheslav Dubynin (Doctor of Biological Sciences, M.V. Lomonosov Moscow State University)
Acetylcholine
(ACh) - a transmitter in postganglionic synapses - accumulates in high concentrations in the vesicles of the axoplasm of the nerve ending. ACh is formed from choline and activated acetic acid (acetyl coenzyme A) under the action of the enzyme acetylcholine transferase. Highly polar choline is actively taken up by the axoplasm. There is a special transport system on the membrane of the cholinergic axon and nerve endings. The mechanism of mediator release has not been fully disclosed. Vesicles are anchored in the cytoskeleton by the synapsin protein in such a way that their concentration near the presynaptic membrane is high, but there is no contact with the membrane. When excitation occurs, the Ca2+ concentration in the axoplasm increases, protein kinases are activated, and phosphorylation of synapsin occurs, leading to the detachment of vesicles and their binding to the presynaptic membrane. The contents of the vesicles are then released into the synaptic cleft. Acetylcholine instantly passes through the synaptic cleft (the ACh molecule is about 0.5 nm long, and the width of the cleft is 30-40 nm). On the postsynaptic membrane, i.e., the membrane of the target organ, ACh interacts with receptors. These receptors are also excited by the alkaloid muscarine and are therefore called muscarinic acetylcholine receptors (M-cholinergic receptors). Nicotine mimics the effect of acetylcholine on receptors at ganglion synapses and the end plate. Nicotine excites cholinergic receptors at ganglion synapses and the end plate of the motor neuron, which is why this type of receptor is called nicotinic acetylcholine receptors (N-cholinergic receptors).
In the synaptic cleft, acetylcholine is quickly inactivated by a specific acetylcholinesterase located in the cleft, as well as by a less specific serum cholinesterase (butyrylcholinesterase) found in the blood serum and interstitial fluid.
Based on their structure, method of signal transmission and affinity for various ligands, M-cholinergic receptors are divided into several types. Let's consider M1, M2 and M3 receptors. M1 receptors are found on nerve cells, such as ganglia, and their activation promotes the transition of excitation from the first to the second neuron. M2 receptors are located in the heart: the opening of potassium channels leads to a slower diastolic depolarization and a decrease in heart rate. M3 receptors play a role in maintaining the tone of smooth muscles, for example, in the intestines and bronchi. Excitation of these receptors leads to activation of phospholipase C, membrane depolarization and increased muscle tone. M3 receptors are also located in gland cells, which are activated by phospholipase C. In the brain there are different types of M-cholinergic receptors that play a role in many functions: transmission of excitation, memory, learning, pain sensitivity, control of brain stem activity. Activation of M3 receptors in the vascular endothelium can lead to the release of nitric oxide NO and thus dilate blood vessels.
Acetylcholine and emotional balance
Smokers know that they need a cigarette to calm down, to cheer up in the morning. Nicotine helps them think about complex problems and, on the contrary, begin active physical work, which does not require much thinking. plays the same role in the human body .
Interestingly, in addition to chemicals, genes also influence the production of acetylcholine. Someone got enzymes and synapses that provide them with a large amount of acetylcholine. And some people have relatively little of this neurotransmitter. Skewing in one direction or the other is not very good.
- With an excess of acetylcholine, a person has excellent memory and a lively mind. But at the same time, he cannot calm down quickly; he is tormented by insomnia.
- With a lack of acetylcholine, a person is calmer and more restrained. But it may seem that he lacks mental agility and speed of reaction.
Acetylcholine levels depend not only on genes. Lifestyle plays a role. Especially physical activity. Psychological attitudes, especially anxiety and severe stress, also play an important role.
Acetylcholine performs the same role as motor oil in an engine
First among equals
Figure 1. Otto Löwy's classic experiment in identifying chemical mediators of nerve impulse transmission (1921). The objects are the hearts of two frogs (donor and recipient) isolated and immersed in a saline solution. Description is given in the text. .
Figure 2. Structural formula of acetylcholine. .
We will talk about acetylcholine, and this will be symbolic, given that it was the first neurotransmitter to be discovered. At the beginning of the 20th century, there was a debate among scientists about how a signal is transmitted from one nerve cell to another. Some believed that an electric charge, having passed through one nerve fiber, was transmitted to another along some thinner “wires.” Their opponents argued that there are substances that carry a signal from one nerve cell to another. In principle, both sides were right: there are chemical and electrical synapses. However, supporters of the second hypothesis turned out to be “to the right” - chemical synapses predominate in the human body.
* - About how our heart contracts - about automatism, conducting pacemakers and even funny channels - read the review “Metronome: how to control the discharges?” . - Ed.
Figure 3. The acetylcholine system of the brain. We see that in the deep parts of the brain there are clusters of nerve cells (in the forebrain and brainstem), which send their processes to various parts of the cortex and subcortical areas. At the terminal points, acetylcholine is released from the neuron endings. The local effects of a neurotransmitter vary depending on the type of receptor and its location. MS - medial septal nucleus, DB - diagonal ligament of Broca, nBM - basal magnocellular nucleus (Meitner's nucleus); PPT - pedunculopontine tegmental nucleus, LDT - lateral dorsal tegmental nucleus (both nuclei are in the reticular formation of the brainstem). Drawing from, adapted.
Acetylcholine receptors are divided into two groups - and. Stimulation of muscarinic receptors leads to a change in metabolism in the cell through the G-protein system* (metabotropic receptors), and the effect on nicotinic receptors leads to a change in membrane potential (ionotropic receptors). This occurs because nicotinic receptors bind to sodium channels on the surface of cells. The expression of receptors varies in different parts of the nervous system (Fig. 4).
* - The spatial structures of several representatives of the huge family of GPCR receptors - membrane receptors acting through the activation of G-protein - are clearly described in the articles: “Receptors in the active form” (about the active form of rhodopsin), “Structures of GPCR receptors “in the piggy bank” "(about dopamine and chemokine receptors), "Mood mediator receptor" (about two serotonin receptors). - Ed.
Figure 4. Distribution of muscarinic and nicotinic receptors in the human brain. .
Acetylcholine dopamine and Parkinson's disease
The mediator acetylcholine is difficult to consider without its connections with other mediators. An example of the improper interaction between acetylcholine and dopamine is the symptoms of Parkinson's disease.
Parkinson's disease is a currently incurable disease that occurs primarily in old age. Although early parkinsonism also occurs from the age of 30. A characteristic feature of such patients is constant trembling of the limbs and difficulties in coordinating movements. Even sitting on a chair or climbing stairs is a problem for such people.
The cause of Parkinson's disease is the depletion and death of cells in the brain that produce the neurotransmitter dopamine. As a result, great difficulty arises in sending a conscious impulse to the muscles, and control over the body is weakened. But the activity of the mediator acetylcholine remains the same. The result is the trembling characteristic of Parkinson's disease.
They try to smooth out this condition using various methods: by blocking the synthesis of acetylcholine or artificially increasing the level of dopamine. But all these drugs are serious and have many side effects. For example, the activity of acetylcholine is reduced by cyclodol, and dopamine is increased by levadopa.
In Alzheimer's disease, which also occurs in old people, acetylcholine, on the contrary, is not enough. And drugs that increase acetylcholine are used for them. These drugs help fight dementia and memory loss in the elderly.
Parkinson's disease
Potential Benefits of Acetylcholine
Increased acetylcholine levels have been associated with several potential health benefits.
May help memory and brain function
Animal and human studies suggest that higher intakes of choline—a precursor to acetylcholine—may improve memory in people with memory problems.
In studies on mice, oral choline supplementation throughout their lifetime significantly improved memory and reduced the formation of beta-amyloid plaques, a compound linked to the development of Alzheimer's disease (, ).
A study of 2,195 participants aged 70–74 found that people with higher levels of choline in their blood had significantly better memory and learning scores than people with lower levels ().
Additionally, supplements that inhibit the breakdown of acetylcholine, such as bacopa monnieri, ginkgo biloba, and huperzine A, have been associated with improved memory and brain function (, , ).
However, research into the effects of these supplements on mental performance is fairly new. More research is needed before recommending them for this purpose.
May support mental health
Some research suggests that acetylcholine precursor supplements may help treat some psychiatric conditions.
An observational study of more than 5,900 participants found that low blood levels of choline were associated with a higher risk of anxiety. However, it did not find a link between blood choline levels and depression ().
Another study of 50 people with depression found that people who took 200 mg of citicoline along with citalopram (an anti-depression medication) daily for 6 weeks had less severe depressive symptoms than those who took anti-depression medications alone ().
There is also some evidence that bacopa monnieri and ginkgo biloba may help reduce anxiety symptoms, but more research in humans is needed (, ).
Additionally, choline supplements are sometimes used to treat symptoms in people with bipolar disorder. However, research in this area is limited and more research is needed before they can be recommended for this purpose (, , ,).
May support a healthy pregnancy
Approximately 90–95% of pregnant women consume less choline than the recommended daily intake ().
There is some evidence that taking choline during pregnancy may promote healthy fetal growth and improved fetal development.
One study found that taking either 480 mg or 930 mg of choline per day during the third trimester of pregnancy significantly improved a child's mental function and memory at 4, 7, 10, and 13 months ().
Another study of 69 pregnant women who drank heavy alcohol found that taking 2 grams of choline daily from mid-pregnancy to birth significantly reduced the effects of alcohol on a child's mental function ().
Several other studies have noted that higher choline intake during pregnancy is associated with a lower risk of neural tube problems in children (, ).
However, other studies have found no association between maternal choline supplementation and fetal brain development or neural tube problems, so more research is needed (, ).
Other Potential Benefits
Taking choline supplements, which can increase acetylcholine levels, may also provide other benefits for various medical conditions.
However, the relationship between choline supplementation and these diseases is not entirely clear, so more research is needed:
- Liver disease. Choline deficiency can cause liver disease, and higher choline intake may be associated with a lower risk of liver disease and liver cancer (, , ).
- Heart disease. There is some evidence that choline may reduce the risk of heart disease and stroke. However, the relationship is unclear and other studies show mixed results ().
Mediator acetylcholine and VSD
The diseases that we wrote about above, parkinsonism and Alzheimer's disease, are poorly understood and require further research. Another mysterious disease that, in our opinion, is associated with the mediator acetylcholine is VSD or vegetative-vascular dystonia.
the diagnosis of VSD very often. According to various sources, this disorder affects from 25 to 70 percent of people. VSD occurs especially often during hormonal changes in adolescents or in women during menopause.
There is an opinion that VSD is a disease that occurs due to the fact that a person’s “needs” and “wants” do not coincide. For example, you are traveling on a trolleybus and are very tired. You relax in the seat and almost fall asleep, but the next second you remember that people are looking at you and force yourself to wake up. This is repeated several times. The balance of neurotransmitters and vascular tone changes. It's tiring. As a result, hypertension may occur or, on the contrary, blood pressure may drop.
Acetylcholine is an important part of the autonomic system. According to the results of recent Russian studies, stress (which is considered the main cause of VSD) causes the release of large amounts of acetylcholine. Acetylcholine is considered a resting neurotransmitter, but after extreme arousal or stress, much more of it is released than usual. If the compensatory systems do not cope and some kind of imbalance occurs in the autonomic system, then this leads to the well-known symptoms of VSD. However, there are now more questions than answers regarding the acetylcholine mediator and the connections between the autonomic and nervous systems.
You may be interested in other articles on our website about hormones and neurotransmitters:
- What is dopamine?
- 5 hormones of joy, happiness and pleasure.
- High and low estrogen in women.
- Oxytocin is the hormone of attachment and pregnancy.
- Adrenaline mediator and medical drug.
Risks and side effects
What happens if you have too much acetylcholine? It's usually difficult to get too much choline from food (which will then be made into acetylcholine), but you can overdose on choline supplements.
The maximum permissible safe daily dosage of choline is 3500 mg. Therefore, to avoid side effects, stay below this level.
Taking high doses of choline can result in the production of too much acetylcholine. In large quantities, supplements can cause low blood pressure, sweating, fishy body odor, and increased salivation.
Conclusion
What is acetylcholine? It is a neurotransmitter that transmits signals between brain cells and is important for memory and other brain functions.
Other functions of acetylcholine include supporting muscle movement, attention, learning, arousal, motivation, and REM sleep.
Acetylcholine dysfunction and deficiency have been linked to cognitive decline, memory impairment, and certain brain disorders such as Alzheimer's disease.
To maintain adequate levels of acetylcholine in the body, it is recommended to include foods rich in choline in your diet - eggs, legumes, turkey. You can also take choline supplements on a short-term basis to enhance cognitive performance with acetylcholine without exceeding the recommended dosage.