Infections that occur in various parts of the central nervous system can be successfully treated by neurologists at our clinic. We will carry out diagnostic measures using the most modern equipment to obtain an accurate diagnosis. The experience of our neurologists allows us to effectively cope with many diseases of the central nervous system, no matter what infections they are caused by: viruses, bacteria, fungal infectious agents, protozoa. We will not only cure the disease, but also restore anti-infective immunity.
The main thing about neuroinfections
The infection can affect any part of the central nervous system: brain, spinal cord, peripheral nerves. Infectious agents can enter through various lesions of the central nervous system. This could be a skull fracture, penetration through the blood or nerves, or other means. The most dangerous are neuroinfections of the brain.
Usually, with good immunity, the central nervous system is completely protected from the penetration of infectious agents (thanks to the skull, spinal column, meningeal membranes). But if the immune system weakens, then due to the penetration of infection (helminthic parasites, fungi, bacteria, viruses) into one or another part of the central nervous system, various pathologies can arise.
Infections are divided into primary and secondary. In the former, an initial infection of the central nervous system occurs; in the latter, infectious agents enter the central nervous system from other foci. Neuroinfections sometimes act as a complication of certain infectious diseases (influenza, tuberculosis, syphilis, herpes, etc.).
There are many separate types of infections of the central nervous system, but doctors distinguish lesions of the membranes of the brain (meningitis) and the spinal cord (myelitis), infection of the substance of the brain (encephalitis) or substance of the spinal cord (encephalomyelitis), inflammation of the roots of the spinal cord (radiculitis), damage to the peripheral nerves (neuritis). ). Our neurologists will provide assistance with a variety of types of neuroinfections, such as:
- Meningitis.
- Encephalitis.
- Leptospirosis.
- Myelitis.
- Rabies.
- HIV.
- Tetanus.
- Borreliosis, tick-borne encephalitis (the infection is transmitted by ticks, the pathogen, when bitten by a tick, enters the bloodstream and then into the central nervous system).
- CNS lesions due to measles, rubella, mumps.
- Infection with herpes group viruses (herpes, cytomegalovirus, etc.).
- Viral hepatitis.
- Parasitic diseases of the central nervous system.
- Toxoplasmosis.
- Leptospirosis.
- Chlamydia.
- Mycoplasmosis.
- Neurosyphilis.
Nervous system damage due to COVID-19
Until recently, the question of whether the SARS-CoV-2 virus affects the structures of the nervous system remained open. Since the beginning of the COVID-19 pandemic, patients have experienced isolated neurological symptoms, and since the beginning of April, reports about the first confirmed cases of damage to the central nervous system and peripheral nerves began to appear in foreign sources. In this material we provide descriptions of these cases. Special thanks to Arthur Arsenyev for his help in translating descriptions of clinical cases.
Some experts suggest that SARS-CoV-2 not only affects the respiratory tract, but also penetrates the central nervous system, causing neurological disorders. The mechanisms of possible involvement of the central nervous system are different, and the authors identify three most likely options.
Firstly, it is possible that the development of respiratory failure accompanying a new coronavirus infection is associated with the involvement in the pathological process of not only the lower respiratory tract, but also the respiratory center in the brain stem. Epidemiological studies show that with the development of coronavirus infection, the average time from the onset of the first symptoms to the development of respiratory failure is 5 days. During this time, the virus can penetrate the blood-brain barrier through the blood or transsynaptically and affect neurons in the brain stem, thereby disrupting the functioning of the respiratory center.
Secondly, the neuroinvasive potential of COVID-19 is studied using the example of coronaviruses that are structurally similar to it. SARS-CoV-1 was detected in the brains of patients and experimental animals, which means that it is possible that penetration into the central nervous system is also possible for SARS-CoV-2. To invade cells, COVID-19 uses angiotensin-converting enzyme type 2 (ACE2) as a receptor, which is found on the surface of neurons and glial cells in the brain. The interaction of coronavirus with these receptors can lead to direct damage to neurons without the development of inflammation. A similar pattern was demonstrated in a series of clinical cases of SARS-CoV-1 infection.
Other mechanisms of damage to the nervous system during a new coronavirus infection are also being considered. Particular attention is paid to immune mechanisms; the possibility of autoimmune effects cannot be excluded. The development of a cytokine storm during coronavirus infection increases the permeability of the blood-brain barrier, allowing the uncontrolled penetration of viruses, bacteria, immune cells, toxic metabolites and inflammatory agents into the structures of the central nervous system. The impact of these factors on the brain tissue and its membranes can lead to the development of neurological symptoms without direct entry of SARS-CoV2, however, these conditions can still be considered associated with this infection.
Sources:
- The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients
- Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host–Virus Interaction, and Proposed Neurotropic Mechanisms
Current studies show that about 8% of patients with confirmed COVID-19 infection complained of headache, 1% of nausea and vomiting. A study of 214 patients confirms that 88% of severely ill patients (78 of 88 in the study group) demonstrate neurological symptoms such as acute cerebrovascular conditions and disturbances of consciousness. According to the same study, in some patients, characteristic symptoms of coronavirus infection appear only some time after the development of the first neurological manifestations. According to postmortem studies, patients who died from the consequences of COVID-19 infection showed signs of cerebral edema.
Thus, healthcare professionals working with COVID-19 should be alert to the possible neuroinvasive potential of the virus. Below we will describe several cases of damage to the nervous system in patients with COVID-19.
Sources:
- The neuroinvasive potential of SARS‐CoV2 may play a role in the respiratory failure of COVID‐19 patients
- Nervous system involvement after infection with COVID-19 and other coronaviruses
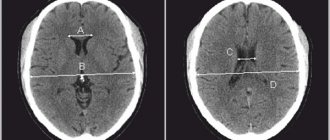
On March 31, a case of COVID-19-associated acute necrotizing hemorrhagic encephalopathy was described in the journal Radiology. This condition is rare and can be associated with viral infections, but this is the first time its association with COVID-19 has been established. The first patient to demonstrate the development of encephalopathy was a woman in her mid-sixties who presented with a three-day history of cough, fever, and confusion. The diagnosis of a new coronavirus infection was confirmed by PCR using a nasal swab. The cerebrospinal fluid showed no bacterial growth or the presence of herpes simplex viruses types 1 and 2, varicella zoster virus, and West Nile virus. It was not possible to test the cerebrospinal fluid for the presence of SARS-CoV-2. Computed tomography of the head without contrast injection showed the presence of symmetrical areas of clearing in the medial parts of the thalamus, as well as normal angiography and venography data. MRI of the brain showed areas of signal enhancement in the thalamus, medial temporal lobes, and subinsular areas suggestive of hemorrhage. .
Picture 1
A. Non-contrast head CT image shows symmetrical areas of hypoattenuation in the medial thalamus (arrows). B. Axial venogram demonstrates normal patency of the venous vasculature, including the internal cerebral veins (arrows). C. Coronal angiogram shows normal alignment of the basilar arteries and proximal portions of the posterior cerebral arteries.
Figure 2
MRI demonstrates T2-FLAIR hyperintense signal in the medial temporal lobes and thalamus ( A, B, E, F ) with evidence of hemorrhage manifested by decreased signal intensity on magnetic susceptibility-weighted images ( C, G ) and edge enhancement in post-contrast images ( D, H ).
The obtained data from instrumental studies indicate the presence of acute necrotizing encephalopathy. This rare complication of viral infections is associated with the development of a cytokine storm, which leads to disruption of the integrity of the blood-brain barrier. In this case, no viral invasion into the brain or demyelination is observed. This condition is more often described in pediatric practice, but its development in adults is not excluded.
Sources:
- COVID-19–associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI Features
Later, the first case of meningitis and encephalitis associated with COVID-19 was described in the International Journal of Infectious Diseases. A 24-year-old patient consulted a doctor at the end of February with complaints of weakness, headache and fever. The doctor suspected the development of influenza and prescribed laninamivir and antipyretics. On the fifth day of the disease, the patient went to another clinic due to a deterioration in his condition, underwent a chest x-ray and a blood test for the presence of coronavirus infection, the blood test was negative. On the ninth day of the disease, the man was found in his own home in an unconscious state, lying in his own vomit. On the way to the hospital, the patient developed generalized seizures that lasted one minute. There was noticeable swelling in the neck area. Upon arrival at the hospital, the patient's impairment of consciousness was assessed as 6 points on the Glasgow Coma Scale (E4 V1 M1) with hemodynamic stability. A blood test showed neutrophilic leukocytosis with lymphopenia and a high level of C-reactive protein. Mononuclear cells and polymorphonuclear cells were detected in the colorless, transparent cerebrospinal fluid, and the presence of SARS-CoV-2 RNA was detected by PCR; the analysis of a nasopharyngeal smear was negative. No IgM antibodies against herpes simplex virus type 1 and varicella zoster virus were detected in the blood serum. Systemic CT did not reveal cerebral edema. A CT scan of the chest showed ground-glass areas in the right upper lobe and both lower lobes. Brain MRI showed hyperintense areas along the wall of the right lateral ventricle and signal changes in the right medial temporal lobe and hippocampus, suggesting the possibility of COVID-19-associated meningitis and encephalitis. .
Figure 3 | MRI of the brain performed 20 hours after the patient was admitted to the hospital
A. Diffusion-weighted images demonstrate hyperintensity along the wall of the inferior horn of the right lateral ventricle. B, C. FLAIR images show hyperintense signal changes in the right temporal lobe and hippocampus with mild hippocampal atrophy. These findings indicate right lateral ventriculitis and encephalitis primarily in the right mesial temporal lobe and hippocampus. D. T2-weighted images show pan-paranasal sinusitis.
In connection with the detection of COVID-19 in the cerebrospinal fluid, in this case we can talk about both an increase in the permeability of the blood-brain barrier and the neuroinvasive potential of the causative agent of coronavirus infection.
Sources:
- A first case of meningitis/encephalitis associated with SARS-Coronavirus-2
One of the characteristic clinical symptoms of a new coronavirus infection is anosmia, sometimes in combination with hypogeusia. The cause of the development of anosmia in the case of a viral infection is considered to be congestion in the mucous membrane of the nasal cavity, leading to obstruction of the nasal passages and temporary loss of sensitivity. However, in some patients, anosmia becomes permanent, which may be due to irreversible viral damage to neurons. It is important to note that ACE2, the receptors required for SARS-CoV-2 invasion, are expressed in the olfactory epithelium.
The structural features of the olfactory areas are studied using MRI. The main MRI findings in anosmia secondary to upper respiratory tract infections are decreased signal levels, suggesting decreased neuronal density that correlates with olfactory function.
On April 13, a case of isolated anosmia in a patient with a new coronavirus infection confirmed by PCR was presented in the journal Academic Radiology. MRI of this patient's olfactory regions was reported to have normal signal intensity and no signs of congestion. This indicates the absence of anatomical changes that could be caused by the SARS-CoV-2 virus, which means that disturbances in the sense of smell are caused rather by functional changes associated with the action of the virus. .
Figure 4
Native T2-weighted coronal MRI images of a 27-year-old man with isolated sudden-onset anosmia and positive PCR for SARS-CoV-2 in the acute phase of the disease show normal signal levels and intensity from the olfactory bulbs without signs of nasal congestion (arrows).
To obtain more detailed data on these changes, the authors proposed conducting combined studies, for example, combining single-photon emission computed tomography with MRI.
Sources:
- Olfactory Bulb Magnetic Resonance Imaging in SARS-CoV-2-Induced Anosmia: The First Report
On April 1, the Lancet published the first case of Guillain-Barré syndrome associated with COVID-19. At the end of February, a 61-year-old woman consulted a doctor with complaints of acute weakness in both legs. She returned from Wuhan in late January but denied developing symptoms such as fever, cough, chest pain and diarrhea. The functional parameters of her respiratory system were normal, and auscultation of the lungs revealed no signs of pathology. Neurological examination showed symmetrical weakness (4/5 MRC muscle strength rating scale) and areflexia in the lower extremities. The symptoms progressed: after three days, muscle strength was 4/5 in the arms and 3/5 in the legs. In the distal parts of the extremities, sensitivity to touch and needle pricks began to decrease. Examination of the cerebrospinal fluid on the fourth day after presentation showed a normal number of cellular elements and a high level of protein. An ENMG performed on day five showed conduction delays in the distal upper and lower extremities and absence of F waves, indicating the presence of demyelinating neuropathy. The woman was diagnosed with Guillain-Barre syndrome.
On the eighth day, the patient developed a dry cough and fever. A chest CT scan showed ground-glass areas in both lungs. SARS-CoV-2 RNA was detected by PCR in nasal mucus smears. After a course of treatment with lopinavir and ritonavir, the patient's condition improved. On the 30th day from the moment of treatment, normal muscle strength in the arms and legs was restored, and tendon reflexes appeared. Relatives who were in contact with a patient with a new coronavirus infection did not experience neurological symptoms.
The authors suggest that COVID-19 is responsible for the development of Guillain-Barré syndrome in this patient. This adds another one to the list of possible mechanisms of damage to the nervous system - autoimmune effects during infection with the new coronavirus.
Thus, at the moment, the literature has already presented cases of damage to the structures of the nervous system during infection with COVID-19 according to three main mechanisms: cytokine storm, direct damaging effect and autoimmune effect. Publication of new clinical cases will shed light on the features of these mechanisms. It is already becoming clear that every specialist working with COVID-19 must be alert to the possible development of neurological symptoms and diagnose them in a timely manner.
Sources:
- Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence?
The development of epilepsy in this case is not entirely correct to consider as associated with COVID-19 - the patient had post-encephalitic epilepsy after another viral disease and successfully controlled the occurrence of epileptic seizures for two years. However, the change in the course of the disease after infection with coronavirus makes us think about the possible impact of a new viral infection on the course of controlled epilepsy.
A 78-year-old woman presented to the emergency department with ongoing myoclonic seizures of the right side of the face and body. The patient has a history of arterial hypertension and postencephalitic epilepsy. At the age of 76 years, a woman suffered from herpesvirus encephalitis, which manifested itself with repeated oral automatisms and aphasia for 6 hours. The EEG showed intermittent epileptiform discharges over the left temporal lobe, forming nonconvulsive status epilepticus. The epistatus was successfully relieved, after which mild aphasia and slight weakness of the limbs persisted. To prevent seizures, the patient took valproic acid and levetiracetam, as a result of which epileptic seizures did not manifest themselves for two years.
On the morning of March 12, 2021, the patient developed focal status epilepticus without prodromal symptoms. The temperature at the time of hospitalization was 36.1 °C. Neurological examination revealed mild aphasia, right facial paralysis, pronation of the right arm, and spastic abduction of the right leg. The patient demonstrated ongoing myoclonic spasms of the right eyelids and upper lip for two hours. Therapy was carried out with intravenous valproic acid and midazolam. The EEG showed irregular, high-amplitude delta activity, mainly localized in the left fronto-central-temporal region. .
Figure 5
15 seconds ( B ) and 30 seconds ( C ) of ictal EEG (study conducted during an attack). Semi-rhythmic irregular high-amplitude delta waves are noted, mainly localized over the left fronto-central-temporal areas, combined with rhythmic artifacts from muscle contractions, more noticeable in the right fronto-temporal projection.
Antiepileptic therapy led to regression of epistatus. A CT scan of the brain did not reveal any acute pathology; an MRI of the brain described foci of gliosis and atrophy of the temporal and parietal lobes on the left, and the absence of new pathological changes and accumulations of contrast agent. Chest X-ray - unremarkable. From laboratory data, lymphocytopenia and thrombocytopenia attract attention. .
Figure 6
A. Axial diffusion-weighted MRI images. B. Axial images with measured diffusion coefficient. C. Axial T1-weighted images after gadolinium administration. D. T2-weighted images in the coronal plane. MRI images demonstrate widespread gliosis and atrophy involving the left temporoparietal lobe and no new brain tissue damage.
12 hours later, the patient developed fever without respiratory manifestations typical of coronavirus infection. Saturation was normal. Blood tests showed a further decrease in white blood cell and platelet levels. C-reactive protein was at the level of 29.7 mg/l, procalcitonin - 0.07 ng/ml. Antibacterial therapy started had no effect on the fever. Blood and urine tests did not reveal the presence of bacteria, fungi or neurotropic viruses.
From the epidemiological history, it became known that in the previous week the patient had seen her son, who had contact with people positive for COVID-19 and had previously been in preventive isolation. PCR of nasopharyngeal and oropharyngeal swabs revealed that the woman had COVID-19. The patient was transferred to the infectious diseases department and received therapy according to the regimen of lopinavir-ritonavir + hydroxychloroquine with a positive effect. Further examination of the lungs did not reveal interstitial pneumonia. The patient did not receive oxygen therapy, and seizures did not recur. On March 28, she was discharged after two negative PCR smears and no fever.
In this case, the coronavirus may have become a trigger for the activation of epileptic activity in a patient who had previously suffered from postencephalitic epilepsy. It should be noted that the invasion of the virus into the central nervous system could not be established, since a spinal puncture and PCR of the cerebrospinal fluid were not performed. For now, it can be assumed that coronavirus infection may be the trigger that, in the absence of other symptoms, can lead to relapses of certain central nervous system diseases.
Sources:
- Focal status epilepticus as unique clinical feature of COVID-19: A case report
To summarize, here is an infographic that visualizes the frequency of the main neurological symptoms that have been reported in COVID-19 patients around the world. .
Sources:
- Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2021 in Wuhan, China
Symptoms of central nervous system damage
Symptoms of diseases vary widely, depending on the type of infection. Movement disorders, muscle weakness, paralysis, and tremors occur. There may be disturbances in speech, coordination, and tactile sensitivity. Symptoms also include headaches, back pain, and limb pain.
Diseases can manifest themselves as fever, convulsions, excitability, epileptic seizures, nausea, vomiting, fatigue, drowsiness, disturbances of consciousness, behavior and mental activity. At the first such signs, you should consult a doctor immediately.
Clinical manifestations.
The symptoms of viral meningitis are similar and do not depend on the causative virus. The onset of the disease is acute. The onset of meningitis may be preceded by a “flu-like” prodrome, as occurs with lymphocytic choriomeningitis. A similar biphasic course of the disease can also occur in young children suffering from polio and diseases caused by viruses carried by insects. Damage to the central nervous system is manifested by intense headache of frontal or retro-orbital localization. Malaise, nausea and vomiting, lethargy, and photophobia may occur. As a rule, disturbances of consciousness are minor. The patient may be drowsy or slightly confused, but is usually oriented and logical. Stupor and coma are rare. The temperature is usually raised to 38-40°C. Rigidity of the neck muscles is detected when the head is flexed. Most patients exhibit Kernig's and Brudzinski's symptoms, but with slight irritation of the meninges, they may be absent. The stiffness of the spine can be so pronounced that the child goes into a sitting position with his head straightened and his arms extended back - a tripod symptom. Symptoms of focal central nervous system lesions are rare. Sometimes it is possible to identify strabismus and diplopia, asymmetry of tendon reflexes, and an unstable extensor plantar reflex.
Clinical symptoms not related to damage to the nervous system can help identify the pathogen. Inflammation of the parotid glands, combined with viral meningitis, indicates mumps. Skin rashes are an important sign of infections caused by the Coxsackie and ECHO viruses. Spotty or pinpoint rashes on the extremities, usually occurring in the summer, are usually observed with an ECHO viral infection. Herpangina (large, painful blisters in the posterior third of the oropharynx) is most often caused by Coxsackie viruses. Sharp pain in the chest, aggravated by deep breathing and coughing, indicates pleuralgia due to Coxsackie virus infection.
Diagnosis of CNS infections in the clinic
Effective treatment of neuroinfections is only possible with an accurate diagnosis. Diagnostic testing may include:
- Examination by a neurologist.
- General urine and blood tests, blood biochemistry.
- Laboratory tests that allow you to identify the pathogen and assess immunity (determination of antibodies to infectious pathogens, PCR diagnostics, cultural cultures). It is a laboratory assessment of immunity that can help determine how the infection entered the central nervous system.
- Electroneuromyography is performed to determine infections of the spinal cord and peripheral nerves.
- Ultrasound diagnostics.
- CT scans of the brain or spinal cord can identify neoplasms and hemorrhages, that is, distinguish infectious causes of central nervous system damage from non-infectious ones.
- Lumbar puncture.
Treatment of neuroinfections
Based on the diagnostic studies performed, the clinic’s specialists will choose intensive therapy aimed at:
- Elimination of the causative agent of the disease. For this, the doctor prescribes the most modern antibiotics, antivirals, interferons, and immunoglobulins.
- Eliminating the source of infection. For example, if the source is in the maxillary sinuses, it is necessary to put them in order.
- Restoration of anti-infective immunity. For this purpose, the neurologist will prescribe special medications.
- Stimulating the functions of affected areas of the central nervous system with the help of effective medications.
Treatment.
Treatment for viral meningitis is symptomatic. In uncomplicated cases, antiviral drugs are not prescribed. Fever and other symptoms resolve within 3-5 days, and within 2 weeks the patient's condition is completely normalized. Changes in the CSF are most pronounced from the 4th to the 6th day, but the increased content of leukocytes in it can persist for several weeks in patients even without any other pathological symptoms. Initial treatment with antimicrobial drugs is indicated in cases where the initial cytosis is not entirely typical for a viral infection. In most cases, patients recover from viral meningitis without consequences. A limited number of patients may develop muscle weakness and other types of movement disorders. Very few patients experience repeated exacerbations of viral meningitis; Multiple episodes of illness are often caused by different viruses.