Venlafaxine
Venlafaxine does not have increased binding to plasma proteins, and practically does not increase the concentration of concomitantly used drugs, which are characterized by high binding to plasma proteins. No clinically significant interaction with antihypertensive (of many pharmacological groups, including beta-blockers, angiotensin-converting enzyme inhibitors and diuretics) and hypoglycemic agents has been identified. Caution should be exercised when used concomitantly with other drugs that affect the central nervous system, since combinations of venlafaxine with such drugs have not been studied.
MAO inhibitors
The simultaneous use of venlafaxine with MAO inhibitors, as well as within 14 days after their discontinuation, is contraindicated (the risk of severe side effects, including death, is likely). Therapy with MAO inhibitors can be carried out no less than 7 days after discontinuation of the drug Venlafaxine. Venlafaxine should be discontinued at least 7 days before starting the use of reversible selective MAO inhibitors (moclobemide). The weakly reversible and non-selective MAO inhibitor linezolid (an antimicrobial agent) and methylene blue (intravenous dosage form) are also not recommended for concomitant use with venlafaxine.
Serotonergic agents
Caution should be exercised in the simultaneous use of drugs that affect the serotonin system of mediators, such as triptans (sumatriptan, zolmitriptan and others), selective serotonin reuptake inhibitors (SSRIs) and SNRIs (prolonged convulsions have been reported), tricyclic antidepressants, lithium, sibutramine or fentanyl (and its analogs dextromethorphan, tramadol and others), as well as excess sources of tryptophan due to the increased potential risk of serotonin syndrome.
Ethanol
During treatment with venlafaxine, ethanol (alcohol) should be completely avoided. Ethanol increases the psychomotor dysfunction that venlafaxine can cause.
Lithium
Lithium preparations do not have a significant effect on the pharmacokinetics of venlafaxine.
Diazepam
There was no effect of diazepam taken orally on the pharmacokinetics of venlafaxine and EDV and, conversely, venlafaxine did not change the pharmacokinetics of diazepam and its metabolite desmethyldiazepam. In addition, the use of both of these drugs does not impair the psychomotor and psychometric effects caused by diazepam.
Cimetidine
The simultaneous use of cimetidine and venlafaxine resulted in a delay in metabolism during the “primary passage” of venlafaxine through the liver. The clearance of venlafaxine when taken orally decreased by 43%, and the AUC (area under the concentration-time pharmacokinetic curve) and maximum concentration (Cmax) in the blood plasma of this drug increased by 60%. However, similar effects were not evident for EFA. Since the total activity of venlafaxine and EDV is expected to increase only slightly, no dose adjustment will be required for most normal patients. However, for patients with existing (identified) arterial hypertension, elderly patients and those with impaired liver or kidney function, a dose adjustment of venlafaxine is possible.
Haloperidol
In a study where venlafaxine was used at steady state at a dose of 150 mg per day, a 42% decrease in the total clearance of oral haloperidol was observed after a dose of 2 g; while AUC increased by 70%, and Cmax increased by 88%, while T1/2 of haloperidol did not change. This should be taken into account when choosing the correct dose of haloperidol.
Imipramine
Venlafaxine does not impair the pharmacokinetics of imipramine and 2-hydroxyimipramine. However, the AUC, Cmax and Cmin (minimum concentration) of desipramine (the active metabolite of imipramine) increase by approximately 35% when used simultaneously with venlafaxine. The concentration of 2-hydroxydesipramine also increases from 2.5 to 4.5 times (depending on the dose of venlafaxine: 37.5 mg for 12 hours or 75 mg for 12 hours), but the clinical significance of this fact is unknown.
Metoprolol
When using metoprolol and venlafaxine simultaneously, caution should be exercised, since due to pharmacokinetic interaction, the concentration of metoprolol in the blood plasma increases by approximately 30-40%, without changing the concentration of its active metabolite α-hydroxymetoprolol. The clinical significance of this interaction has not been studied. Metoprolol does not affect the AUC of venlafaxine and EDV.
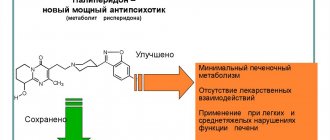
Risperidone
When used concomitantly with risperidone (despite an increase in the AUC of risperidone), the pharmacokinetics of the pair of active molecules (risperidone and 9-hydroxyrisperidone) do not change significantly when used simultaneously with venlafaxine.
Clozapine
During post-marketing studies of venlafaxine, it was found that when used simultaneously with clozapine, its concentration in the blood plasma increases. This results in increased side effects of clozapine, especially seizures.
Indinavir
With simultaneous use, the pharmacokinetics of indinavir changes (AUC decreases by 28%, Cmax decreases by 36%). For venlafaxine, no changes in pharmacokinetics are observed. The clinical significance of this fact is unknown.
Ketoconazole
Pharmacokinetic studies with simultaneous use with ketoconazole showed an increase in plasma concentrations of venlafaxine and EDV in healthy volunteers whose initial metabolism with the participation of the CYP2D6 isoenzyme is both good (X-Met) and poor (P-Met). In particular, the Cmax of venlafaxine increased by 26% for X-Met and by 48% for P-Met. Cmax EFA values increased by 14% and 29% in X-Met and P-Met volunteers, respectively. The AUC of venlafaxine increased by 21% in X-Met and by 70% in P-Met. EFA AUC values increased by 23% and 33% in X-Met and P-Met volunteers, respectively.
Drugs affecting the blood coagulation system and platelet function (non-steroidal anti-inflammatory drugs (NSAIDs), acetylsalicylic acid and other anticoagulants)
Serotonin, released by platelets, plays an important role in hemostasis (stopping bleeding). Epidemiological studies demonstrate an association between the use of psychotropic drugs that interfere with serotonin reuptake and the incidence of upper gastrointestinal bleeding. This relationship is enhanced if NSAIDs, acetylsalicylic acid preparations or other anticoagulants are used simultaneously. The risk of bleeding has been shown to increase when SSRIs and SNRIs (including venlafaxine) are used concomitantly with warfarin. Patients receiving warfarin should be closely monitored for prothrombin time and/or partial thromboplastin time, especially when co-administration with venlafaxine is started or stopped.
Interaction with other drugs at the level of studied metabolism with isoenzymes of the cytochrome P450 system
The main routes of metabolism of venlafaxine include the CYP2D6 and CYP3A4 isoenzymes: the first of them converts venlafaxine into its active metabolite EDV, and the second is less important in the metabolism of venlafaxine compared to the CYP2D6 isoenzyme and forms the product N-desmethylvenlafaxine with low pharmacological activity. The results of preclinical studies showed, and then it was confirmed clinically, that venlafaxine is a relatively weak inhibitor of the CYP2D6 isoenzyme. Therefore, when used with drugs that moderately suppress the activity of this isoenzyme (see information with imipramine above), or in the case of patients with a genetically determined decrease in the function of the CYP2D6 isoenzyme, no dose adjustment of venlafaxine is required, since the total concentration of the active substance and active metabolite (venlafaxine and EFA) does not change significantly. This characterizes venlafaxine positively when compared with other antidepressants. Caution should be exercised when used concomitantly with inhibitors of the CYP2D6 isoenzyme such as quinidine, paroxetine, fluoxetine, haloperidol, perphenazine, levomepromazine, since in this case venlafaxine may potentially increase the plasma concentration of these CYP2D6 isoenzyme substrates. In combination with drugs that inhibit both isoenzymes (CYP2D6 and CYP3A4), special caution is required. Such drug interactions have not yet been sufficiently studied, and in this case such a combination of drugs is not recommended.
In addition, venlafaxine does not suppress the activity of the isoenzymes CYP3A4, CYP1A2 and CYP2C9, therefore, no significant interaction is observed with drugs such as alprozolam, caffeine, carbamazepine, diazepam, tolbutamide, terfenadine.
Interaction with ketoconazole is described above. Inhibitors of CYP3A3/4 isoenzymes such as itraconazole and ritonavir can have a similar effect.
Other interactions with various concomitant therapeutic factors and food
When using venlafaxine, special caution should be exercised when administering electroconvulsive therapy, since there is no experience with the use of venlafaxine in these conditions.
There was no significant effect of different types of food on the absorption of venlafaxine and its subsequent conversion to EDV. Foods (usually high in protein, such as hard cheeses, fish roe, turkey), as well as dietary supplements and fitness diets that are high sources of tryptophan, potentially increase the body's production of serotonin, which may increase the serotonergic side effects of venlafaxine .
Undesirable pharmacodynamic interactions may occur when venlafaxine is used simultaneously with the drug St. John's wort (herb or various preparations made from it); such a combination is not recommended.
There are reports of false-positive results of the immunochromatographic rapid urine test (test strip) for phencyclidine and amphetamines in patients taking venlafaxine, even several days after discontinuation of venlafaxine. This may be explained by the lack of specificity of this test. Venlafaxine can only be distinguished from phencyclidine and amphetamines by a confirmatory test carried out in a specialized anti-doping laboratory.
According to the data available to date, venlafaxine has not shown itself to be a drug that causes drug abuse or addiction (both in preclinical receptor affinity studies and in clinical practice).
Venlafaxine organic 37.5 mg 30 pcs. film-coated tablets
pharmachologic effect
Antidepressant.
Composition and release form Venlafaxine organic 37.5 mg 30 pcs. film-coated tablets
Tablets - 1 tablet:
- Active substance: venlafaxine - 37.5/75 mg;
- Excipients;
- mCC - 53.03/106.06 mg; lactose monohydrate (milk sugar) - 35.1/70.2 mg; sodium carboxymethyl starch (Primogel) - 15.7/31.4 mg; povidone (low molecular weight medical PVP) K17 - 2.65/5.3 mg; magnesium stearate - 1.1/2.2 mg;
- film shell;
- Opadry II (85F28751) white (polyvinyl alcohol - 2/4 mg, titanium dioxide - 1.25/2.5 mg, macrogol (PEG) - 1.01/2.02 mg, talc - 0.74/1.48 mg) - 5/10 mg.
There are 30 pieces in a package.
Description of the dosage form
White or almost white, film-coated tablets, round, biconvex; On a cross section, the core is white or almost white.
Directions for use and doses
The recommended starting dose is 75 mg in 2 divided doses daily (37.5 mg 2 times a day). Depending on tolerability and effectiveness, the dose may be gradually increased to 150 mg/day. If necessary, the dose is increased to 225 mg/day. Dose increases by 75 mg/day can be made at intervals of 2 weeks or more; if clinically necessary, due to the severity of symptoms, it is possible to increase the dose in a shorter period of time, but not less than 4 days. Higher doses (up to a maximum daily dose of 375 mg/day in 2-3 doses) require inpatient monitoring of patients. After achieving the required therapeutic effect, the daily dose can be gradually reduced to the minimum effective level.
Maintenance therapy and relapse prevention. Maintenance treatment can last 6 months or more. The minimum effective doses used in the treatment of a depressive episode are prescribed.
Kidney failure. In case of mild renal failure (GFR > 30 ml/min), no dosage adjustment is required. In case of moderate renal failure (GFR 10-30 ml/min), the dose should be reduced by 25-50%. Due to the prolongation of T1/2 of venlafaxine and its active metabolite (EAM), such patients should take the entire dose once a day. It is not recommended to use venlafaxine in severe renal failure (GFR less than 10 ml/min)).
Pharmacodynamics
Venlafaxine is an antidepressant that does not chemically belong to any class of antidepressants (tricyclic, tetracyclic or others) and is a racemate of two active enantiomers.
Venlafaxine and its main metabolite, O-desmethylvenlafaxine (ODV), are strong SNRIs and weak dopamine reuptake inhibitors.
The mechanism of the antidepressant effect of the drug is associated with its ability to potentiate the transmission of nerve impulses to the central nervous system.
Venlafaxine and ODV are equally effective in influencing the reuptake of the above-mentioned neurotransmitters, while they do not have an affinity (studied in vitro) for cholinergic (muscarinic), H1-histamine, alpha1-adrenergic, opiate and benzodiazepine receptors, and do not suppress MAO activity. Also have no affinity for opiate, phencyclidine, or N-methyl-d-aspartate (NMDA) receptors. Venlafaxine is inferior to SSRIs in inhibiting serotonin reuptake. In addition, venlafaxine and EDV reduce beta-adrenergic reactivity both after a single dose and with chronic use.
Pharmacokinetics
Absorption. Absorption from the gastrointestinal tract is good, about 92% for a single dose, and is not quantitatively dependent on food intake.
Distribution. Overall bioavailability is 40-45%, which is associated with intense first-pass metabolism in the liver. Venlafaxine and EDV bind to human plasma proteins by 27 and 30%, respectively; they both pass into breast milk. In the range of daily doses of venlafaxine 75-450 mg, venlafaxine and EDV have linear kinetics. Tmax in blood plasma of venlafaxine and EDV is 2 and 3 hours, respectively, after taking Venlafaxine tablets orally.
When taking long-acting forms of venlafaxine, Tmax is 5.5 and 9 hours, respectively.
T1/2 was (5±2) hours and (11±2) hours for venlafaxine and EDV, respectively.
Css for venlafaxine and EDV is achieved after 3 days of multiple therapeutic doses.
Metabolism. Metabolized mainly in the liver with the participation of the CYP2D6 isoenzyme to the only pharmacologically active metabolite (EFA), as well as to the inactive metabolite N-desmethylvenlafaxine.
Venlafaxine is a weak inhibitor of the CYP2D6 isoenzyme and does not inhibit CYP1A2, CYP2C9 or CYP3A4.
Excretion. Excreted primarily by the kidneys: approximately 87% of a single dose taken is excreted in the urine within 48 hours (5% unchanged, 29% as unconjugated EDV, 26% as conjugated EDV, 27% as other inactive metabolites) , and after 72 hours, 92% of the drug is excreted by the kidneys.
The mean ± standard deviation for plasma clearance of venlafaxine and EDV is (1.3 ± 0.6) and (0.4 ± 0.2) L/h/kg, respectively; apparent T1/2 (5±2) and (11±2) h, respectively; apparent Vss (7.5±3.7) and (5.7±1.8) l/kg, respectively.
Special groups of patients.
The gender and age of the patient do not have a significant effect on the pharmacokinetic parameters of venlafaxine and EFA.
For elderly patients, no special dose adjustment is required depending on age.
In patients with low activity of the CYP2D6 isoenzyme, there is no need to select individual doses. Despite the multidirectional changes in concentrations taken separately, namely venlafaxine (increases) and EDV (decreases), the sum of the AUC of these two active substances does not actually change due to a decrease in the activity of the CYP2D6 isoenzyme; accordingly, no dose adjustment is required.
In patients with moderate to severe hepatic and renal insufficiency, the metabolism of venlafaxine and the excretion of EDV is reduced, the Cmax of venlafaxine and EDV is increased, and T1/2 is prolonged. The decrease in the total clearance of venlafaxine is most pronounced in patients with creatinine Cl below 30 ml/min, as well as in patients on renal dialysis (T1/2 increases by 180% for venlafaxine and by 142% for ODV, and the clearance of both active substances decreases by approximately by 57%). For such patients, especially those on hemodialysis, it is necessary to individually select the dose of venlafaxine and monitor the kinetics, taking into account the duration of treatment with this drug.
Although data for patients with severe Child-Pugh hepatic impairment are limited, it should be borne in mind that individual variations in pharmacokinetics, in particular drug clearance and T1/2, are very variable, which should be taken into account when prescribing venlafaxine to such patients. In patients with Child-Pugh class A (mild liver dysfunction) and Child-Pugh class B (moderate impairment), the T1/2 of venlafaxine and EDV is approximately 2 times longer than that in healthy patients, and clearance is reduced by more than half.
Indications for use Venlafaxine organic 37.5 mg 30 pcs. film-coated tablets
Depression (prevention and treatment).
Contraindications
- Hypersensitivity to venlafaxine or any of the excipients;
- simultaneous use with MAO inhibitors;
- severe renal and/or liver dysfunction (GFR
Application Venlafaxine organic 37.5 mg 30 pcs. film-coated tablets during pregnancy and breastfeeding
Contraindicated for children under 18 years of age and during pregnancy and breastfeeding.
special instructions
Recent myocardial infarction; unstable angina; arterial hypertension; tachycardia; history of convulsive syndrome; increased IOP; angle-closure glaucoma; history of manic states; predisposition to bleeding from the skin and mucous membranes; initially reduced body weight.
Overdose
Symptoms: impaired consciousness (from drowsiness to coma), agitation, possible vomiting, diarrhea; tremor, decrease or (mild) increase in blood pressure, dizziness, mydriasis, convulsive states, sinus or ventricular tachycardia or bradycardia; changes on the ECG (prolongation of the QT interval, bundle branch block, widening of the QRS complex). Post-marketing experience indicates that the most common overdose of venlafaxine occurred with concomitant use of alcohol and/or other psychotropic drugs. There are repeated reports of deaths. Published literature on retrospective studies of venlafaxine overdoses report that this increased risk of fatal outcomes may be inherent in venlafaxine when compared with commercially available SSRI antidepressants, but this risk is lower than the risk inherent in tricyclic antidepressants. Epidemiological studies have shown that those patients treated with venlafaxine have a greater risk of suicide compared with those patients treated with SSRIs (other than venlafaxine). However, it remains unclear to what extent these high rates of death (due to venlafaxine overdose) are due to the toxic properties of the drug itself or the special characteristics of the group of patients treated with venlafaxine. According to clinical experience, it is recommended that prescriptions for venlafaxine prescribe the minimum possible amount, sufficient only until the patient's next visit to the doctor, in order to reduce the risk of intentional overdose.
Treatment: symptomatic and supportive therapy is provided. Specific antidotes are unknown. Continuous monitoring of vital functions (respiration, circulation and heart rate) is recommended. In case of overdose, immediate gastric lavage and administration of activated charcoal are recommended to reduce absorption of the drug. It is not recommended to induce vomiting if there is a risk of aspiration of vomit. Forced diuresis, dialysis, and blood transfusion are ineffective.
Side effects Venlafaxine organic 37.5 mg 30 pcs. film-coated tablets
General symptoms: often - weakness, increased fatigue, chills; uncommon - Quincke's edema, photosensitivity reactions; frequency not established - anaphylactic reactions.
From the nervous system: very often - dry mouth, headache; often - unusual dreams, decreased libido, dizziness, insomnia, increased excitability, paresthesia, stupor, confusion, depersonalization, increased muscle tone, tremor; infrequently - apathy, agitation, hallucinations, myoclonus, impaired coordination of movements and balance; rarely - akathisia, psychomotor agitation, epileptic seizures, manic reactions; frequency not established - dizziness, neuroleptic malignant syndrome (NMS), serotonin syndrome, delirium, extrapyramidal reactions (including dystonia and dyskinesia), tardive dyskinesia, suicidal thoughts and behavior, aggression.
From the gastrointestinal tract: very often - nausea; often - loss of appetite (anorexia), constipation, vomiting; infrequently - bruxism, diarrhea; rarely - hepatitis; frequency not established - pancreatitis.
From the respiratory system: often - yawning, bronchitis, shortness of breath; rarely - interstitial lung diseases (ILD) and eosinophilic pneumonia, chest pain.
From the cardiovascular system: often - arterial hypertension, hyperemia of the skin; uncommon - postural hypotension, tachycardia, fainting; frequency not established - hypotension, QT interval prolongation, ventricular fibrillation, ventricular tachycardia (including bidirectional tachycardia).
From the hematopoietic system: infrequently - hemorrhages into the skin (ecchymosis), gastrointestinal bleeding; frequency not established - hemorrhages in the mucous membranes, prolongation of bleeding time, thrombocytopenia, pathological changes in the blood (including agranulocytosis, aplastic anemia, neutropenia and pancytopenia).
From the metabolic side: often - increased cholesterol levels in the blood serum, decreased body weight; infrequently - weight gain; very rarely - an increase in prolactin levels; frequency not established - changes in laboratory tests of liver function, hepatitis, hyponatremia, syndrome of insufficient ADH secretion.
From the genitourinary system: often - ejaculation/orgasm disorders in men, erectile dysfunction (impotence), anorgasmia, dysuric disorders (mainly difficulty in starting urination), pollakiuria, menstrual disorders associated with increased bleeding or increased irregular bleeding (menorrhagia, metrorrhagia); infrequently - orgasm disorders in women, urinary retention; rarely - urinary incontinence.
From the senses: often - disturbances of accommodation, mydriasis, blurred vision; infrequently - disturbance of taste, noise or ringing in the ears; frequency not established - angle-closure glaucoma.
From the skin: very often - sweating; infrequently - alopecia, a rapidly passing rash; frequency not established - erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome, itching, urticaria.
From the musculoskeletal system: frequency not established - rhabdomyolysis.
When you stop taking venlafaxine, abruptly discontinue it, or reduce the dose, you may experience symptoms that are referred to as so-called. withdrawal syndrome: increased fatigue, asthenia, headache, dizziness, sleep disturbances (drowsiness or insomnia, difficulty falling asleep, the appearance of unusual dreams), hypomania, anxiety, agitation (increased nervous excitability and irritability), confusion, paresthesia (including spontaneously occurring unpleasant sensation of numbness, tingling, burning, crawling), increased sweating, dry mouth, decreased appetite, nausea, vomiting, diarrhea (most of these reactions are mild and do not require treatment).
Drug interactions
Venlafaxine, which itself does not have increased binding to plasma proteins, practically does not increase the concentration of simultaneously taken drugs, which are characterized by high binding to plasma proteins. No clinically significant interaction with antihypertensive (including beta-blockers, ACE inhibitors, diuretics) and antidiabetic drugs was detected.
Caution should be exercised when co-administered with other drugs that affect the central nervous system, since the interaction of venlafaxine with such drugs has not been studied.
MAO inhibitors. The simultaneous use of venlafaxine with MAO inhibitors, as well as within 14 days after their discontinuation, is contraindicated (the risk of severe side effects, including death, is likely). Therapy with MAO inhibitors can be prescribed no less than 7 days after discontinuation of the drug Venlafaxine. Venflaxin should be discontinued at least 7 days before starting reversible selective MAO inhibitors (moclobemide). The weakly reversible and non-selective MAO inhibitor linezolid (an antimicrobial drug) and methylene blue (IV dosage form) are also not recommended for simultaneous use with venlafaxine.
Serotonergic agents. Caution should be exercised in the simultaneous use of drugs that affect the serotonergic transmission of drugs, such as triptans (including sumatriptan, zolmitriptan), SSRIs, SNRIs (prolonged seizures have been reported), tricyclic antidepressants, lithium, sibutramine or fentanyl (including including its analogues - dextromethorphan, tramadol), as well as excess sources of tryptophan due to the increased potential risk of serotonin syndrome.
Alcohol. During treatment with venlafaxine, alcohol should be completely avoided. Alcohol increases the psychomotor dysfunction that venlafaxine can cause.
Lithium. Lithium preparations do not have a significant effect on the pharmacokinetics of venlafaxine.
Diazepam. There was no effect of orally administered diazepam on the pharmacokinetics of venlafaxine and EDV, and, conversely, venlafaxine did not change the pharmacokinetics of diazepam and its metabolite desmethyldiazepam. In addition, the administration of both of these drugs does not impair the psychomotor effects and psychometric indicators caused by diazepam.
Cimetidine. The simultaneous administration of cimetidine and venlafaxine led to a delay in metabolism during the first passage of venlafaxine through the liver. Oral clearance of venlafaxine decreased by 43%, and AUC and Cmax of the drug increased by 60%. However, such an impact was not evident for EFA. Since the total activity of venlafaxine and EFA is expected to increase only slightly, no dose adjustment will be required for most normal patients. However, in patients with existing (detected) hypertension, elderly patients and those with impaired liver or kidney function, the dose of venlafaxine may be adjusted.
Haloperidol. In a study where venlafaxine was administered in the Css stage at a dose of 150 mg/day, a 42% decrease in total oral haloperidol clearance was observed after a 2 mg oral dose; while AUC increased by 70%, and Cmax by 88%, while T1/2 of haloperidol did not change. This should be taken into account when choosing the correct dose of haloperidol.
Imipramine. Venlafaxine does not impair the pharmacokinetics of imipramine and 2-hydroxyimipramine. However, the AUC, Cmax and Cmin of desipramine (the active metabolite of imipramine) increased by approximately 35% when co-administered with venlafaxine. The concentration of 2-hydroxydesipramine also increases 2.5 or 4.5 times (depending on the dose of venlafaxine: 37.5 mg or 75 mg 2 times a day), but the clinical significance of this fact is unknown.
Metoprolol. When using metoprolol and venlafaxine simultaneously, caution should be exercised because due to pharmacokinetic interaction, the concentration of metoprolol in the blood plasma increases by approximately 30-40%, without changing the concentration of its active metabolite alpha-hydroxymetoprolol. The clinical significance of this interaction has not been studied. Metoprolol does not affect the AUC of venlafaxine and EDV.
Risperidone. When used concomitantly with risperidone (despite an increase in the AUC of risperidone), the pharmacokinetics of a pair of active molecules (risperidone and 9-hydroxyrisperidone) do not change significantly when combined with venlafaxine.
Clozapine. During post-marketing studies of venlafaxine, it was found that when used simultaneously with clozapine, its concentration in the blood plasma increases. This was manifested by an increase in the side effects of clozapine, especially in relation to the incidence of seizures.
Indinavir. With simultaneous use, the pharmacokinetics of indinavir changes (AUC decreases by 28% and Cmax decreases by 36%). There are no changes in the pharmacokinetics of venlafaxine. The clinical significance of this fact is unknown.
Ketoconazole. A pharmacokinetic study when combined with ketoconazole showed an increase in plasma concentrations of venlafaxine and EDV in subjects whose initial metabolism by CYP2D6 is either good (X-Met) or poor (P-Met). In particular, the Cmax of venlafaxine increased by 26% for X-Met and by 48% for P-Met. EFA Cmax values increased by 14 and 29% in X-Met and P-Met subjects, respectively. The AUC of venlafaxine increased by 21% in X-Met and by 70% in P-Met. EFA AUC values increased by 23 and 33% in X-Met and P-Met subjects, respectively.
Drugs that affect blood clotting and platelet function (NSAIDs, acetylsalicylic acid preparations and other anticoagulants). Serotonin, released by platelets, plays an important role in hemostasis (stopping bleeding). Epidemiological studies demonstrate an association between the use of psychotropic medications that interfere with serotonin reuptake and the incidence of upper GI bleeding. This relationship is enhanced if NSAIDs, drugs containing acetylsalicylic acid, or other anticoagulants are used simultaneously. The risk of bleeding has been shown to increase when SSRIs and SNRIs (including venlafaxine) are prescribed concomitantly with warfarin. Patients prescribed warfarin should be closely monitored for PT and/or partial thromboplastin time, especially when co-administration with venlafaxine is started or stopped.
Interaction with other drugs at the level of studied metabolism with cytochrome P450 isoenzymes. The main routes of metabolism of venlafaxine include the isoenzymes CYP2D6 and CYP3A4: the first of them converts venlafaxine into its active metabolite EDV, and the second is less important in the metabolism of venlafaxine compared to CYP2D6 and forms the product N-desmethylvenlafaxine with little pharmacological activity. Preclinical studies have shown, and subsequently confirmed clinically, that venlafaxine is a relatively weak inhibitor of CYP2D6. Therefore, even when prescribing drugs that moderately suppress the activity of this enzyme or in the case of treating patients with a genetically determined decrease in CYP2D6 function, no dose adjustment of venlafaxine is required, because the total concentration of the active substance and active metabolite (venlafaxine and EDV) does not change significantly. This characterizes venlafaxine positively when compared with other antidepressants. Caution should be exercised when co-administered with CYP2D6 inhibitors such as quinidine, paroxetine, fluoxetine, haloperidol, perphenazine, levomepromazine, because in this case, venlafaxine may potentially increase plasma concentrations of these CYP2D6 substrates. In combination with drugs that inhibit both enzymes (CYP2D6 and CYP3A4), special caution is required. Such drug interactions have not yet been sufficiently studied and in this case such a combination of drugs is not recommended. In addition, venlafaxine does not suppress the activity of the enzymes CYP3A4, CYP1A2 and CYP2C9, therefore, no significant interaction is observed with drugs such as alprazolam, caffeine, carbamazepine, diazepam, tolbutamide, terfenadine.
Interaction with ketoconazole is described above. CYP3A3/4 inhibitors such as itraconazole and ritonavir can have a similar effect.
Other interactions with various concomitant therapeutic factors and food. When using venlafaxine, special caution should be exercised during electroconvulsive therapy, because There is no experience with the use of venlafaxine in these conditions. A significant effect of different types of food on the absorption of venlafaxine and its subsequent conversion to EDV has not been identified. Foods (usually high in protein, such as hard cheeses, fish roe, turkey), as well as dietary supplements and fitness diets that contain tryptophan, potentially increase the body's production of serotonin, which may increase the serotonergic side effects of venlafaxine.
Preparations containing St. John's wort. Undesirable pharmacodynamic interactions may occur when Venlafaxine is taken simultaneously with the medicinal plant St. John's wort (herb or various preparations made from it); such a combination is not recommended.
There are reports of false-positive results of the immunochromatographic rapid urine test (test strip) for phencyclidine and amphetamines in patients taking venlafaxine, even several days after discontinuation of venlafaxine. This may be explained by the lack of specificity of this test. Only a confirmatory test in a specialized anti-doping laboratory can distinguish venlafaxine from phencyclidine and amphetamines.
According to the data available to date, venlafaxine has not shown itself to be a drug that causes drug abuse or addiction (both in preclinical receptor affinity studies and in clinical practice).
INSTRUCTIONS for medical use of the drug VELAXIN® (VELAXIN®)
Registration number: LS 000030
Trade name: VELAXIN®
INN: venlafaxine
Dosage form: extended-release capsules
COMPOSITION: active substance: each capsule contains 75 mg and 150 mg of venlafaxine (in the form of venlafaxine hydrochloride). Excipients: MCC - 56/112 mg; sodium chloride - 46/92 mg; ethylcellulose - 17.69/35.38 mg; talc - 5.85/11.7 mg; dimethicone - 3.05/6.09 mg; potassium chloride - 2.41/4.81 mg; copovidone - 1.77/3.54 mg; colloidal silicon dioxide anhydrous - 1/2 mg; xanthan gum - 0.31/0.63 mg; iron oxide yellow - 0.16/0.32 mg
Composition of the gelatin capsule: titanium dioxide - 1/1%; iron oxide red - 0.47/0.47%; iron oxide yellow - 0.45/0.45%; gelatin - up to 100/100%
DESCRIPTION OF DOSAGE FORM
Capsules, 75 mg: hard gelatin self-closing capsules, with a colorless, transparent base and an orange-brown cap, containing a mixture of white and yellow pellets, odorless or almost odorless.
Capsules, 150 mg: hard gelatin self-closing capsules, with a colorless, transparent base and an orange-brown cap, containing a mixture of white and yellow pellets, odorless or almost odorless.
PHARMACEUTICAL GROUP(S): Antidepressant.
ATX CODE: N06AX16.
PHARMACODYNAMICS
Venlafaxine is an antidepressant. Based on its chemical structure, it cannot be classified into any known class of antidepressants (tricyclic, tetracyclic or others). It has two active enantiomeric racemic forms.
The antidepressant effect of venlafaxine is associated with increased neurotransmitter activity in the central nervous system. Venlafaxine and its main metabolite O-desmethylvenlafaxine (ODV) are potent serotonin and norepinephrine reuptake inhibitors and weakly inhibit neuronal dopamine reuptake. Venlafaxine and EDV are equally effective in inhibiting the reuptake of neurotransmitters. Venlafaxine and EDV reduce beta-adrenergic reactions.
Venlafaxine has no affinity for muscarinic, cholinergic, histamine H1- and α1-adrenergic receptors in the brain. Venlafaxine does not inhibit MAO activity. Has no affinity for opiate, benzodiazepine, phencyclidine, or N-methyl-D-aspartate (NMDA) receptors.
PHARMACOKINETICS
After taking Velaxin® extended-release capsules, Cmax of venlafaxine and EDV (main metabolite) in plasma are achieved within (6.0±1.5) and (8.8±2.2) hours, respectively. The rate of absorption of venlafaxine from extended-release capsules is lower than the rate of its elimination. Therefore, T1/2 of venlafaxine after the administration of Velaxin® in the form of extended-release capsules - (15±6) hours - is actually T1/2 of absorption rather than T1/2 of distribution - (5±2) hours - which is noted after the administration of the drug Velaxin ® in tablet form.
The binding of venlafaxine and EDV to plasma proteins is 27 and 30%, respectively. EDV and other metabolites, as well as unmetabolized venlafaxine, are excreted by the kidneys. With repeated administration of venlafaxine Css and EDV are achieved within 3 days. In the range of daily doses of 75–450 mg, venlafaxine and EDV have linear kinetics. After taking the drug with food, Tmax in the blood plasma increases by 20–30 minutes, but the values of Cmax and absorption do not change.
In patients with liver cirrhosis, plasma concentrations of venlafaxine and EDV are increased, and their elimination rate is reduced. In moderate or severe renal failure, the total clearance of venlafaxine and EDV is reduced, and T1/2 increases. A decrease in total clearance is mainly observed in patients with creatinine Cl below 30 ml/min.
The age and gender of the patient do not affect the pharmacokinetics of the drug.
INDICATIONS
Depression (including in the presence of anxiety), treatment and relapse prevention.
CONTRAINDICATIONS
- hypersensitivity to any component of the drug;
- simultaneous use of MAO inhibitors (see also “Interaction”);
- severe renal and/or liver dysfunction (glomerular filtration rate (GFR) less than 10 ml/min, PT more than 18 s);
- age under 18 years (safety and effectiveness for this age group have not been proven);
- pregnancy or suspected pregnancy;
- lactation period (there is insufficient data from controlled studies).
With caution: recent myocardial infarction, unstable angina, heart failure, coronary artery disease, ECG changes, incl. prolongation of the QT interval, electrolyte imbalance, arterial hypertension, tachycardia, history of seizures, intraocular hypertension, angle-closure glaucoma, history of manic states, predisposition to bleeding from the skin and mucous membranes, initially reduced body weight.
USE IN PREGNANCY AND BREAST-FEEDING
The safety of venlafaxine during pregnancy has not been proven, so use during pregnancy (or intended pregnancy) is only possible if the potential benefit to the mother outweighs the possible risk to the fetus. Women of childbearing age should be warned about this before starting treatment and should immediately consult a doctor if they become pregnant or plan to become pregnant during treatment with the drug.
Venlafaxine and EDV are excreted into breast milk. The safety of these substances for newborns has not been proven, so taking venlafaxine during breastfeeding is not recommended. If it is necessary to take the drug during lactation, the issue of stopping breastfeeding should be decided. If maternal treatment was completed shortly before delivery, the newborn may experience drug withdrawal symptoms.
METHOD OF APPLICATION AND DOSES
Inside, during meals. Each capsule should be swallowed whole with liquid. Capsules should not be divided, crushed, chewed, or placed in water. The daily dose should be taken at one time (morning or evening), each time at approximately the same time.
Depression. The recommended starting dose is 75 mg once a day.
If, in the opinion of the doctor, a higher dose is necessary (major depressive disorder or other conditions requiring hospital treatment), you can immediately prescribe 150 mg 1 time per day. Subsequently, the daily dose can be increased by 75 mg at intervals of 2 weeks or more (but not more often than after 4 days) until the desired therapeutic effect is achieved. The maximum daily dose is 350 mg.
After achieving the required therapeutic effect, the daily dose can be gradually reduced to the minimum effective level.
Maintenance therapy and relapse prevention. Treatment for depression should continue for at least 6 months. Stabilization therapy, as well as therapy to prevent relapses or new episodes of depression, usually use doses that have been demonstrated to be effective. The doctor should regularly (at least once every 3 months) monitor the effectiveness of long-term therapy with Velaxin®.
Transfer of patients from Velaxin® tablets. Patients taking Velaxin® in the form of tablets can be switched to taking the drug in the form of extended-release capsules, with an equivalent dose prescribed once a day. However, individual dosage adjustments may be required.
Kidney failure. In case of mild renal failure (GFR more than 30 ml/min), no dosage adjustment is required. For moderate renal failure (GFR 10–30 ml/min), the dose should be reduced by 50%. Due to the prolongation of T1/2 of venlafaxine and EDV, such patients should take the entire dose once a day. It is not recommended to use venlafaxine in severe renal failure (GFR less than 10 ml/min), since there are no reliable data on such therapy. Patients on hemodialysis may receive 50% of the usual daily dose of venlafaxine after completion of hemodialysis.
Liver failure. In case of mild liver failure (PT less than 14 s), no adjustment of the dosage regimen is required. In case of moderate liver failure (PT 14 to 18 s), the dose should be reduced by 50%. The use of venlafaxine in severe hepatic impairment is not recommended as reliable data on such therapy are lacking.
Elderly patients. The elderly age of the patient itself does not require a dose change, however (as with the prescription of other drugs) caution is required when treating elderly patients, for example due to the possibility of impaired renal function. The lowest effective dose should be used. When increasing the dose, the patient should be under close medical supervision.
Children and adolescents (under 18 years of age). The safety and effectiveness of venlafaxine in children and adolescents under 18 years of age have not been established.
Discontinuation of the drug Velaxin®. As with treatment with other antidepressants, abrupt discontinuation of venlafaxine (especially high doses) may cause symptoms and "Special Instructions"). Therefore, before completely discontinuing the drug, a gradual dose reduction is recommended. If high doses have been used for more than 6 weeks, it is recommended to reduce doses for at least 2 weeks. The length of time required to reduce the dose depends on the dose size, duration of therapy, and patient reactions.
SIDE EFFECTS
Most of the side effects listed below are dose dependent. With long-term treatment, the severity and frequency of most of these effects decreases, and there is no need to discontinue therapy.
In order of decreasing frequency: often - <1/10 and >1/100; uncommon - <1/100 and >1/1000; rarely - <1/1000; very rarely - <1/10000.
General symptoms: weakness, fatigue, headache, abdominal pain, chills, fever.
From the gastrointestinal tract: loss of appetite, constipation, nausea, vomiting, dry mouth; infrequently - bruxism, reversible increase in the activity of liver enzymes; rarely - gastrointestinal bleeding; very rarely - pancreatitis.
From the nervous system: dizziness, insomnia, agitation, drowsiness; often - unusual dreams, anxiety, confusion, increased muscle tone, paresthesia, tremor; infrequently - apathy, hallucinations, myoclonus; rarely - ataxia, speech disorders, incl. dysarthria, mania or hypomania (see “Special Instructions”), manifestations resembling neuroleptic malignant syndrome, seizures (see “Special Instructions”), serotonergic syndrome; very rarely - delirium, extrapyramidal disorders, incl. dyskinesia and dystonia, tardive dyskinesia, psychomotor agitation/akathisia (see “Special Instructions”).
From the cardiovascular system: arterial hypertension, dilation of blood vessels (flushes), rapid heartbeat; uncommon - orthostatic hypotension, fainting, tachycardia; very rarely - ari, prolongation of the QT interval, ventricular tachycardia, ventricular fibrillation.
From the senses: disturbances of accommodation, mydriasis, blurred vision, tinnitus; infrequently - disturbance of taste.
From the hematopoietic system: infrequently - hemorrhages in the skin (ecchymosis) and mucous membranes; rarely - thrombocytopenia, prolongation of bleeding time; very rarely - agranulocytosis, aplastic anemia, neutropenia, pancytopenia.
From the skin: sweating, itching and rash; uncommon - photosensitivity reactions, angioedema, maculopapular rash, urticaria; rarely - alopecia, erythema multiforme, Stevens-Johnson syndrome.
From the genitourinary system: disorders of ejaculation, erection, anorgasmia; uncommon - decreased libido, menstrual irregularities, menorrhagia, urinary retention; rarely - galactorrhea.
Metabolism: increased serum cholesterol levels, decreased body weight; uncommon - hyponatremia, syndrome of insufficient ADH secretion, abnormal liver function tests; rarely - hepatitis; very rarely - increased prolactin levels.
Musculoskeletal system: arthralgia, myalgia; infrequently - muscle spasm; very rarely - rhabdomyolysis.
The following side effects have been observed in children: abdominal pain, chest pain, tachycardia, food refusal, weight loss, constipation, nausea, ecchymosis, epistaxis, mydriasis, myalgia, dizziness, emotional lability, tremor, hostility and suicidal ideation.
After abrupt discontinuation of venlafaxine or a reduction in its dose, the following may be observed: fatigue, drowsiness, headache, nausea, vomiting, anorexia, dry mouth, dizziness, diarrhea, insomnia, restlessness, anxiety, disorientation, hypomania, paresthesia, sweating. These symptoms are usually mild and go away without treatment. Because these symptoms are likely to occur, it is important to gradually reduce the dose of the drug (as with any antidepressant), especially after taking high doses. The length of the period required to reduce the dose depends on the dose size, duration of therapy, as well as the individual sensitivity of the patient.
INTERACTION
The simultaneous use of MAO inhibitors and venlafaxine is contraindicated. Taking Velaxin® can be started no less than 14 days after the end of therapy with MAO inhibitors. If a reversible MAO inhibitor (moclobemide) was used, this interval may be shorter (24 hours). Therapy with MAO inhibitors can be started no less than 7 days after discontinuation of Velaxin®.
Concomitant use of venlafaxine with lithium may increase the level of the latter.
When used simultaneously with imipramine, the pharmacokinetics of venlafaxine and EDV do not change. At the same time, their simultaneous use enhances the effects of desipramine, the main metabolite of imipramine, and its other metabolite, 2-OH-imipramine, although the clinical significance of this phenomenon is unknown.
Haloperidol: Concomitant use increases haloperidol blood levels and enhances its effects.
When used simultaneously with diazepam, the pharmacokinetics of the drugs and their main metabolites do not change significantly. There was also no effect on the psychomotor and psychometric effects of diazepam.
When used simultaneously with clozapine, an increase in its level in the blood plasma and the development of side effects (for example, seizures) may be observed.
When used simultaneously with risperidone (despite the increase in AUC of risperidone), the pharmacokinetics of the sum of the active components (risperidone and its active metabolite) does not change significantly.
The decrease in mental and motor activity under the influence of alcohol did not increase after taking venlafaxine. Despite this, as in the case of taking other drugs that affect the central nervous system, the consumption of alcoholic beverages is not recommended during venlafaxine therapy.
While taking venlafaxine, special caution should be exercised during electroconvulsive therapy, because There is no experience with the use of venlafaxine in these conditions.
Drugs metabolized by cytochrome P450 isoenzymes: the cytochrome P450 enzyme CYP2D6 converts venlafaxine to the active metabolite EDV. Unlike many other antidepressants, the dose of venlafaxine does not need to be reduced when coadministered with drugs that inhibit CYP2D6 activity, or in patients with a genetically determined decrease in CYP2D6 activity, since the total concentration of venlafaxine and EDV will not change.
The main route of elimination of venlafaxine involves metabolism by CYP2D6 and CYP3A4; therefore, special caution should be exercised when prescribing venlafaxine in combination with drugs that inhibit both of these enzymes. Such drug interactions have not yet been studied.
Venlafaxine is a relatively weak inhibitor of CYP2D6 and does not suppress the activity of the CYP1A2, CYP2C9 and CYP3A4 isoenzymes; therefore, it should not be expected to interact with other drugs that are metabolized by these liver enzymes.
Cimetidine inhibits the first-pass metabolism of venlafaxine and does not affect the pharmacokinetics of EDV. In most patients, only a slight increase in the overall pharmacological activity of venlafaxine and EDV is expected (more pronounced in elderly patients and with impaired liver function).
Clinical studies have not revealed clinically significant interactions of venlafaxine with antihypertensive (including beta-blockers, ACE inhibitors and diuretics) and antidiabetic drugs.
Drugs bound to plasma proteins: Plasma protein binding is 27% for venlafaxine and 30% for EFA, so drug interactions due to protein binding should not be expected.
When taken simultaneously with warfarin, the anticoagulant effect of the latter may be enhanced, while the PT is prolonged and the MHO increases.
When taken simultaneously with indinavir, the pharmacokinetics of indinavir changes (with a 28% decrease in AUC and a 36% decrease in Cmax), but the pharmacokinetics of venlafaxine and EDV do not change. However, the clinical significance of this effect is unknown.
OVERDOSE
Symptoms: ECG changes (prolongation of the QT interval, bundle branch block, expansion of the QRS complex), sinus or ventricular tachycardia, bradycardia, arterial hypotension, convulsive states, depression of consciousness (decreased level of wakefulness). Death has been reported in cases of overdose of venlafaxine when taken concomitantly with alcohol and/or other psychotropic drugs.
Treatment: symptomatic. Specific antidotes are unknown. Continuous monitoring of vital functions (respiration and circulation) is recommended. Prescribing activated carbon to reduce drug absorption. Inducing vomiting is not recommended due to the risk of aspiration. Venlafaxine and EDV are not eliminated by dialysis.
SPECIAL INSTRUCTIONS
Depression increases the risk of suicidal thoughts and suicide attempts. This risk persists until stable remission occurs. Therefore, patients should be under constant medical supervision and should be given only small quantities of the drug capsules to reduce the risk of possible abuse and/or overdose.
Velaxin® should not be used in the treatment of children and adolescents under 18 years of age. Increases in the likelihood of suicidal behavior (suicide attempt and suicidal ideation) and hostility in clinical trials were observed more often among children and adolescents receiving antidepressants compared with groups receiving placebo.
Aggressive behavior has been reported while taking venlafaxine (especially at the beginning of treatment and after discontinuation of the drug).
The use of venlafaxine may cause psychomotor restlessness, which clinically resembles akathisia, characterized by restlessness with a need to move, often combined with an inability to sit or stand still. This is most often observed during the first few weeks of treatment. If these symptoms occur, increasing the dose may have an adverse effect, and continued use of the drug should be considered.
Like all antidepressants, venlafaxine should be prescribed with caution to patients with a history of mania and/or hypomania, because the drug may cause an increase in their symptoms. In these cases, medical supervision is necessary.
Caution should be exercised when treating patients with a history of seizures. If convulsive seizures occur or their frequency increases, treatment with venlafaxine should be interrupted.
Like selective serotonin reuptake inhibitors, venlafaxine should be used with caution when used concomitantly with antipsychotic drugs, because Symptoms resembling neuroleptic malignant syndrome may develop.
Patients should be warned to seek immediate medical attention if rash, hives, or other allergic reactions occur.
Some patients experienced a dose-dependent increase in blood pressure while taking venlafaxine, and therefore regular blood pressure monitoring is recommended, especially at the beginning of treatment or when the dose is increased.
Isolated cases of orthostatic hypotension have been described while taking venlafaxine. Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance.
Venlafaxine may cause an increase in heart rate, especially at high doses. Particular caution should be exercised when prescribing the drug to patients with conditions that may be aggravated by an increase in heart rate.
There are insufficient studies of the use of venlafaxine in patients who have recently suffered a myocardial infarction or suffering from decompensated heart failure, so this drug should be used with caution in these patients.
Like other serotonin reuptake inhibitors, venlafaxine may increase the risk of bleeding into the skin and mucous membranes, so caution is required when treating patients predisposed to bleeding.
While taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient ADH secretion may occur.
Cases of mydriasis have been reported while taking venlafaxine, so patients with a predisposition to increased IOP or those at risk of angle-closure glaucoma require careful medical monitoring.
In case of renal and liver failure, special caution is required. In some cases, a dose reduction is required (see “Dosage and Administration”).
Safety and effectiveness of using venlafaxine with drugs that reduce body weight, incl. phentermine have not been established, so their simultaneous use (as well as the use of venlafaxine as monotherapy for weight loss) is not recommended. Clinically significant increases in serum cholesterol levels have been observed in some patients receiving venlafaxine for at least 4 months. Therefore, when taking the drug for a long time, it is advisable to monitor serum cholesterol levels.
After stopping the drug, especially abruptly, symptoms o) often occur. The risk of withdrawal symptoms may depend on several factors, including: duration of the course and dose, as well as the rate of dose reduction. Withdrawal symptoms such as dizziness, sensory disturbances (including paresthesia and electrical sensation), sleep disturbances (including insomnia and unusual dreams), agitation or anxiety, nausea and/or vomiting, tremors, sweating , headache, diarrhea, rapid or increased heart rate, and emotional instability are usually mild to moderate in severity, but may be severe in some patients. They are usually observed in the first days after discontinuation of the drug, although there have been isolated reports of such symptoms in patients who accidentally missed a dose. Usually these phenomena resolve on their own within 2 weeks; however, in some patients they may be longer lasting (2–3 months or more). Therefore, before discontinuing venlafaxine, it is recommended to gradually reduce its dose over several weeks or months, depending on the patient's condition (see "Dosage and Administration").
Impact on the ability to drive vehicles and operate machinery. It should be taken into account that any drug therapy with psychoactive drugs may reduce the ability to make judgments, think or perform motor functions. The patient should be warned about this before starting treatment. If such effects occur, the degree and duration of restrictions should be determined by a physician.
RELEASE FORM
Long-acting capsules. 10 or 14 caps. in a blister made of PVC/PVDC/aluminum foil. 2 blisters of 14 caps. or 3 blisters of 10 caps. cardboard pack.
STORAGE CONDITIONS. In a dry place, at temperatures below 30°C.
Keep out of the reach of children.
BEST BEFORE DATE. 5 years.
MANUFACTURER
CJSC "EGIS Pharmaceutical Plant". 1106, Budapest, st. Keresturi, 30-38, Hungary.
Tel.: (36 1) 803-55-55; fax: (36 1) 803-55-29.
Representative office of JSC "EGIS Pharmaceutical Plant" (Hungary) in Moscow. 121108, Moscow, st. Ivana Franko, 8.
Tel..
CONDITIONS OF VACATION FROM PHARMACIES
On prescription.