Valdoxan®
Liver function monitoring
Cases of liver damage (including liver failure, increases in liver enzyme levels more than 10 times the ULN, hepatitis and jaundice) have been reported in patients taking Valdoxan® in the post-marketing period. Most of these disorders occurred in the first months of treatment. The nature of liver damage appears to be primarily hepatocellular. As a rule, after cessation of therapy, transaminase levels returned to normal values.
It is recommended to monitor liver function at the beginning of therapy and then periodically, after 3 weeks, after 6 weeks (end of the relief period of therapy), 12 weeks and 24 weeks (end of the maintenance period of therapy) after the start of therapy, and thereafter in accordance with the clinical situation. When increasing the dose, liver function should be monitored at the same frequency as at the beginning of the drug.
If the activity of transaminases in the blood serum increases, a repeat test should be performed within 48 hours. If the activity of transaminases is more than 3 times higher than the ULN, the drug should be discontinued. In the future, the functional state of the liver should be regularly monitored until transaminase activity normalizes.
If you experience symptoms and signs of possible liver dysfunction (such as dark urine, discolored stools, yellow skin/eyes, pain in the right upper abdomen, new persistent and unexplained fatigue), Valdoxan should be stopped immediately.
Caution should be exercised when prescribing Valdoxan® to patients with elevated transaminase activity before starting therapy (above the ULN, but not more than 3 times the ULN).
Caution should be exercised when prescribing Valdoxan® to patients with risk factors for developing liver dysfunction, such as obesity/overweight/non-alcoholic fatty liver disease, diabetes mellitus, drinking significant amounts of alcohol, or taking medications that can cause liver dysfunction.
Elderly patients
The effectiveness of the drug in elderly patients (aged 65 years and older) has not been established. There is limited data on the use of Valdoxan® for major depressive episodes in patients aged 65 years and older. When prescribing the drug to elderly patients, caution should be exercised.
Patients with kidney failure
In patients with severe renal failure, no significant changes in pharmacokinetic parameters were observed. However, experience with the use of the drug for major depressive episodes in patients with moderate or severe renal failure is limited. When prescribing Valdoxan® to such patients, caution should be exercised.
Bipolar disorders/mania/hypomania
Caution should be exercised when using Valdoxan® in patients with a history of bipolar disorders, manic or hypomanic episodes. If symptoms of mania appear, you should stop taking the drug.
Suicide/suicidal behavior
People who are depressed have an increased risk of suicidal ideation, self-harm, and suicide (suicide-related events). The risk remains until a clear remission occurs. Patients should be under medical supervision until the condition improves (after starting therapy, it may take several weeks for the condition to improve). Clinical experience suggests that the risk of suicide may increase in the early stages of remission.
Patients with a history of events associated with suicide, as well as patients who had suicidal intentions before starting therapy, are at risk and should be under close medical supervision during therapy.
The results of a meta-analysis of clinical trials of antidepressants in patients with mental disorders indicate an increased risk of suicidal behavior in patients under the age of 25 years while taking antidepressants compared with placebo.
During the treatment period, patients, especially those at risk, should be under close medical supervision, especially at the beginning of therapy and when changing the dose of the drug. Patients (and their caregivers) should be advised to seek immediate medical attention if their condition worsens, if they experience suicidal or unusual behavior, or if they experience suicidal thoughts.
Combined use with CYP1A2 isoenzyme inhibitors
Caution should be exercised when using agomelatine simultaneously with moderate inhibitors of the CYP1A2 isoenzyme (such as propranolol, grepafloxacin, enoxacin) due to the possibility of increasing the concentration of agomelatine.
Impact on the ability to drive vehicles and operate machinery
No studies have been conducted to study the effect of Valdoxan® on the ability to drive a car or use other mechanisms. It should be remembered that dizziness and drowsiness are common side effects of agomelatine.
Valdoxan tablets 25 mg 14 pcs. in Novosibirsk
Agomelatine is an agonist of melatonergic receptors MT1 and MT2 and an antagonist of serotonin 5-HT2C receptors.
Agomelatine is an antidepressant active in validated models of depression (learned helplessness test, despair test, moderate chronic stress), as well as in models with desynchronization of circadian rhythms, as well as in experimental situations of anxiety and stress. Agomelatine has been shown to have no effect on monoamine uptake and has no affinity for alpha, beta adrenergic, histaminergic, cholinergic, dopaminergic and benzodiazepine receptors.
Agomelatine enhances the release of dopamine and norepinephrine, especially in the prefrontal cortex, and does not affect the concentration of extracellular serotonin. In animal experiments with circadian rhythm desynchronization, agomelatine has been shown to restore circadian rhythm synchronization through stimulation of melatonin receptors.
Agomelatine helps restore normal sleep structure, reduce body temperature and release melatonin.
The effectiveness of short-term use of agomelatine (therapy for 6–8 weeks) in doses of 25–50 mg in patients with major depressive episodes has been shown.
The use of agomelatine has also been shown to be effective in patients with more severe forms of depressive disorder (Hamilton scale score ≥25).
Agomelatine was also effective for initially high levels of anxiety, as well as for combined anxiety and depressive disorders.
The supporting antidepressant effect of agomelatine was confirmed (with a study duration of 6 months) at a dose of 25–50 mg once a day.
The results of the study confirmed the anti-relapse effectiveness of agomelatine, which was assessed by time to disease relapse (p=0.0001). The relapse rate in the group of patients taking agomelatine was 22%, in the placebo group - 47%.
Agomelatine was shown to be effective in 6 of 7 clinical studies (benefit (2 studies), or comparable efficacy (4 studies)) in heterogeneous populations of adult patients with depression, compared with SSRIs/SNRIs (sertraline, escitalopram, fluoxetine, venlafaxine or duloxetine) . Antidepressant effect was assessed using the Hamilton scale (17-item version) as either a primary or secondary endpoint.
Agomelatine does not have a negative effect on attention and memory; in patients with depression, agomelatine at a dose of 25 mg increases the duration of the slow-wave sleep phase without changing the number and duration of REM sleep phases. Taking agomelatine at a dose of 25 mg also promotes a faster onset of sleep with a decrease in heart rate and improved sleep quality (starting from the first week of treatment); however, there is no inhibition during the daytime.
When taking agomelatine, there was a tendency to reduce the frequency of sexual dysfunction (impact on arousal and orgasm).
Taking agomelatine has no effect on heart rate and blood pressure, does not cause sexual dysfunction, does not cause withdrawal syndrome (even with abrupt cessation of treatment) and addiction syndrome.
The effectiveness of agomelatine at a dose of 25–50 mg once daily was confirmed in elderly depressed patients under 75 years of age during an 8-week clinical trial. There is no evidence of a significant effect in patients aged 75 years and older.
The tolerability of agomelatine in elderly patients is comparable to that in young patients.
In a 3-week, controlled study of patients with major depressive disorder who had experienced insufficient therapeutic response to paroxetine (SSRI) or venlafaxine (SNRI), withdrawal symptoms were observed when switching from these antidepressants to agomelatine. Withdrawal syndrome appeared both after immediate cessation of treatment with previously prescribed SSRIs/SNRIs, and during their gradual withdrawal, which could be mistakenly taken as a manifestation of the low effectiveness of agomelatine at the initial stage of treatment.
The number of patients who experienced at least one withdrawal symptom one week after SSRI/SNRI discontinuation was lower in the long-term taper group (gradually tapering the SSRI/SNRI dose over 2 weeks) than in the rapid taper group. dosage (gradual reduction of SSRI/SNRI dose over 1 week), and than with immediate withdrawal: 56.1%, 62.6% and 79.8% of patients, respectively.
Valdoxan 25 mg 98 pcs. film-coated tablets
Composition and release form Valdoxan 25 mg 98 pcs. film-coated tablets
Film-coated tablets 25 mg - 1 tablet:
- active ingredients: agomelatine - 25 mg;
- excipients: lactose monohydrate; magnesium stearate; corn starch; povidone, colloidal silicon dioxide; sodium carboxymethyl starch; stearic acid; glycerol; hypromellose; iron oxide yellow dye; macrogol 6000; titanium dioxide;
- blue paint composition: shellac; propylene glycol; indigo carmine aluminum varnish.
In a blister pack 10 pcs.; 10 packs in a cardboard pack; or in a blister pack 14 pcs.; in a cardboard pack 1, 2 or 7 packages.
Description of the dosage form
Orange-yellow, oblong, with a blue company logo on one side.
Directions for use and doses
Valdoxan is prescribed at a dose of 25 mg per day (1 tablet), taken in the evening. The attending physician can individually prescribe a dose of 50 mg for daily use.
Pharmacodynamics
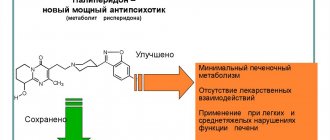
Antidepressant, melatonin agonist (MT1 and MT2 receptors) and serotonin antagonist (5-HT2c receptors). Agomelatine is active in validated models of depression (learned helplessness test, despair test, moderate chronic stress), in models with heart rate desynchronization, as well as in experimental situations of anxiety and stress. It has been shown that agomelatine does not affect the uptake of monamines and has no affinity for alpha, beta adrenergic receptors, histamine receptors, cholinergic receptors, dopamine and benzodiazepine receptors; This explains the absence of agomelatine’s side effects on the gastrointestinal tract, sexual functions and cardiovascular system, which are characteristic of other antidepressants. Agomelatine, due to its antagonistic effect on serotonin 5-HT2c receptors, enhances the release of dopamine and norepinephrine, especially in the prefrontal cortex.
In experimental animal studies with simulated Delayed Sleep Phase Syndrome in blind and aged animals, agomelatine was shown to restore synchronization of circadian rhythms through stimulation of melatonin receptors. In case of chronic stress, agomelatine prevents the occurrence of “broken” (fragmented) sleep. In experiments on healthy volunteers, agomelatine did not disrupt the normal structure of sleep and had a beneficial effect on sleep in patients with depression. In therapeutic doses, agomelatine prevented the development of insomnia and memory impairment from the moment of taking the drug until the morning. Agomelatine is not addictive, as demonstrated in a study of healthy volunteers using a visual analogue scale or the Addiction Research Center Inventory (ARCI 49 check-list). Agomelatine has also been assessed for withdrawal symptoms in depressed patients using the Discontinuation Emergent Signs and Symptoms (DESS) Questionnaire. It has been established that withdrawal syndrome does not develop even with abrupt cessation of treatment. Agomelatine does not affect body weight.
Agomelatine's clinical development program examined its efficacy and safety in major depressive disorder. In a placebo comparative controlled study, 4500 patients were examined, of whom 2500 received the drug for 6 weeks to a year. Agomelatine was statistically significantly more effective compared to placebo, with the antidepressant effect occurring within 2 weeks (efficacy range: from 49.1 to 61% versus 34.3 to 46.3% in the placebo group). Reliable data were also obtained on the effectiveness of agomelatine in patients with more severe forms of depressive disorder (Hamilton scale scores >=25), constituting more than 2/3 of the population. Active control studies confirmed the results. Agomelatine was also effective for initially high levels of anxiety, as well as for combined anxiety and depressive disorders. The effect of agomelatine on the sexual function of patients with depression with a relapsing course of the disease was studied. The Sex Effects Scale (SEXFX) was used. Agomelatine has not been shown to cause sexual dysfunction and does not affect arousal or orgasm. In patients with depression, starting from the second week of treatment, agomelatine statistically significantly improved the process of falling asleep, without causing subsequent daytime lethargy (the Leeds Questionnaire was used).
Pharmacokinetics
Suction
After oral administration, agomelatine is quickly and well (>80%) absorbed from the gastrointestinal tract. Cmax in plasma is achieved 1-2 hours after administration. Bioavailability at a therapeutic dose taken orally is approximately 3% and varies depending on the first pass effect through the liver and individual differences in CYP1A2 activity parameters. When prescribed in therapeutic doses, the therapeutic concentration of the drug increased in proportion to the dose. Meal intake (both regular and high-fat) did not affect either bioavailability or rate of absorption.
Distribution
The volume of distribution at equilibrium was about 35 liters. Plasma protein binding is 95%, regardless of drug concentration, age or the presence of renal failure.
Metabolism
After oral administration, agomelatine undergoes rapid oxidation, mainly due to CYP1A2 (90%) and CYP2C9 (10%). The main metabolites in the form of hydroxylated and demethylated agomelatine are inactive, quickly bind and are excreted in the urine. Removal of T1/2 from plasma is from 1 to 2 hours. Removal occurs quickly. High and mostly metabolic Cl is about 1100 ml/min. Excretion occurs mainly in urine (80%) and in the form of metabolites. The amount of unchanged drug in the urine is insignificant. With repeated administration of the drug, the kinetics do not change.
Pharmacokinetics in special clinical situations
The dependence of the pharmacokinetics of the drug on age has not been identified. Since no significant changes in pharmacokinetics are observed in patients with renal failure, special selection of drug doses for this category of patients is not required. When comparing the effect of the drug in healthy volunteers (matched for age, body weight and number of cigarettes smoked) with patients with mild (Child-Pugh class A) and moderate (Child-Pugh class B) degrees of liver failure, in the latter an increase in the duration of action of the drug was observed when prescribed at a dose of 25 mg/day. No unusual adverse reactions were observed.
Indications for use Valdoxan 25 mg 98 pcs. film-coated tablets
"Valdoxan" is a drug with an antidepressant effect, used in the complex treatment of severe depressive disorder.
Contraindications
You should not take Valdoxan if you have an individual sensitivity to the components of the dietary supplement. A contraindication is considered to be severe renal failure.
Application Valdoxan 25 mg 98 pcs. film-coated tablets during pregnancy and breastfeeding
During pregnancy, Valdoxan is prescribed with caution; lactation should be stopped during the course of therapy. Persons under 18 years of age are not recommended to take the drug due to the lack of sufficient clinical studies in this group of patients.
Overdose
Studies on healthy volunteers have shown that when taken orally, agomelatine is well tolerated at doses up to 800 mg/day. Cases of agomelatine overdose are rare. During clinical trials, doses of up to 300 and up to 375 mg/day were reported in combination with other psychotropic drugs. In all of these cases, no signs or symptoms of overdose were reported.
Treatment: In case of overdose, specific antidotes for agomelatine are not known. Symptomatic therapy and the usual monitoring for such cases in specialized departments are indicated.
Side effects Valdoxan 25 mg 98 pcs. film-coated tablets
"Valdoxan" can cause adverse reactions from:
- central and peripheral nervous system: dizziness, paresthesia;
- Gastrointestinal tract: nausea, diarrhea, dry mouth, pain in the epigastric zone, AST increase 3 times relative to normal;
- skin: dermatitis, itching, eczema, erythematous rash;
- eye: blurred vision.
Drug interactions
Potentially possible interaction: 90% of agomelatine is metabolized in the liver with the participation of CYP1A2 isoenzymes and 10% with the participation of CYP2C9/19. Therefore, any drugs whose metabolism depends on these isoenzymes may increase or decrease the bioavailability of agomelatine. Fluvoxamine, which is a strong inhibitor of CYP1A2 and 2C9, may significantly slow down the metabolism of agomelatine (simultaneous use is not recommended).
Paroxetine (a CYP1A2 inhibitor) and fluconazole (a strong CYP2C9 inhibitor) do not interfere with the pharmacokinetics of agomelatine. Estrogens, which are moderate inhibitors of CYP1A2, have been shown to enhance the effects of agomelatine. As long as the therapeutic concentration of the drug remains within the normal range of pharmacokinetics, no dose adjustment is required.
Smoking increases the effect of CYP1A2, but has been shown to only slightly decrease the duration of action of agomelatine. Therefore, smokers do not need to adjust their dose.
Possibility of action of agomelatine on other drugs Agomelatine does not induce or inhibit CYP450 isoenzymes and therefore does not affect the action of drugs whose metabolism is associated with these isoenzymes. In healthy volunteers, agomelatine did not change the pharmacokinetics of theophylline (CYP1A2). Agomelatine does not change the free concentration of drugs that are significantly bound to plasma proteins and, in turn, do not affect the concentration of agomelatine.
There is no pharmacokinetic or pharmacodynamic interaction between lorazepam and agomelatine. There is no pharmacokinetic or pharmacodynamic interaction between lithium preparations and agomelatine. There are no data on the use of agomelatine concomitantly with electroconvulsive therapy. Since agomelatine did not show seizure-predisposing properties in animal experiments, undesirable effects of electroconvulsive therapy when used together seem unlikely.