Quetiapine
Chemical group: Quetiapine (Seroquel) is a dibenzothiazepine compound.
Release form: tablets 25, 100, 200, 300 mg
Pharmacokinetics: half-life - 7 hours, peak and stabilization of concentration 1.5 hours and 2 days, respectively.
Dosage regimen: Most psychiatrists recommend a gradual increase in quetiapine doses. Initially, the drug is prescribed 25 mg orally twice a day with meals or outside meals. If the drug is well tolerated, the dose is adjusted to 50 mg twice. on the second day, then up to 100 mg twice daily. by 150 mg twice daily on approximately the fourth day of therapy. The average effective daily dose is 300-450 mg in several doses, less often the drug is prescribed at a dose of 150-850 mg/day. If there is no effect within three weeks, the dose of the drug is increased to 600-800 mg per day or more and then, having achieved a positive effect, it is gradually reduced.
According to some researchers, the initial daily dose of quetiapine should not be high due to possible severe sedation and drowsiness. Quetiapine is believed to require a slower dose increase than risperidone and olanzapine. In this case, the daily dose for the first four days of therapy is 50 mg (day 1), 100 mg (day 2), 200 mg (day 3), 300 mg (day 4).
More recent work suggests that the initial daily dose of quetiapine may be higher for the treatment of an acute episode of schizophrenia. On the first day, this dose may correspond to 150-400 mg; 500 mg or more on the second day (Peuskens J. et al., 2007).
In the elderly and in patients with liver disease, the drug is used with caution, starting with 25 mg, with a daily dose increase of 25-50 mg.
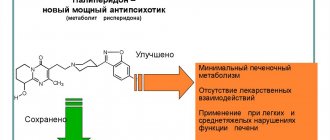
Mechanism of action: the drug has relatively low affinity (compared to other atypical antipsychotics) for 5HT1A and 5HT2A receptors, moderate to high affinity for alpha1, alpha2 and H1 receptors and lower activity against D1, D2, D3, D4, D5 - dopamine receptors. As a result of the above, quetiapine does not cause significant dopaminergic side effects. At the same time, according to the results of some studies, quetiapine at a daily dose of 800 mg blocks up to 50% of dopamine receptors. Quetiapine, unlike risperidone and olanzapine, quickly binds to D2 receptors and is also quickly released from them (“fast dissociation constant”), hence the lack of effect in terms of the occurrence of extrapyramidal disorders. Some authors associate the future direction of the synthesis of new atypical antipsychotics with the effect of “rapid release of dopamine receptors”.
Indications: Compared to risperidone and olanzapine, the drug is considered a relatively weak antipsychotic, but its effect is dose dependent. According to a number of authors, quetiapine is better tolerated than risperidone and olanzapine; in addition, its use is recommended in the treatment of schizoaffective disorders and for the treatment of patients with schizophrenia who are prone to aggression and socially dangerous actions (Styazhkin V.D., Tarasevich L.A., 2007). According to a number of researchers, quetiapine is almost twice as effective as haloperidol in terms of reducing positive and negative symptoms.
Indications for treatment of schizophrenia with quetiapine:
- Poor tolerability of atypical antipsychotics such as risperidone and olanzapine
- Schizoaffective disorders, comorbid depressive spectrum disorders
- Aggressiveness
- Tendency to develop extrapyramidal symptoms
- First psychotic episode
- Maintenance therapy
Side effects: the most common side effects of quetiapine include dizziness, hypotension, tachycardia, and QT segment prolongation on the ECG.
Side effects of quetiapine:
- Cardiovascular disorders (orthostatic hypotension, tachycardia, QT segment prolongation)
- Neurological disorders (drowsiness, rarely: insomnia, epileptiform syndrome, extrapyramidal symptoms, myalgia)
- Mild gastroenterological, endocrine and metabolic disorders (dry mouth, constipation, dyspepsia, weight gain, decreased levels of thyroid hormones)
Orthostatic hypotension, less often hypertension, is more often observed in elderly and debilitated patients. The drug should be used with caution in persons suffering from cardiovascular pathology, as well as in patients with a history of seizures. Cases of cataracts have been reported in patients receiving quetiapine for a long time.
Side effects of the drug also include mild drowsiness and, less commonly, insomnia. Due to drowsiness, the drug is not recommended for patients who drive. There have been cases of increased severity of obsessive states when taking quetiapine.
When taking quetiapine, dizziness, constipation, dry mouth, changes in liver enzyme levels, mild asthenia, rhinitis, dyspepsia, limited weight gain, headache, and fever occasionally occur.
Extrapyramidal symptoms rarely develop when taking quetiapine. Peripheral edema, priapism, myalgia (pain in the abdomen, lower back) are also noted among the rare side effects of the drug.
In some cases, an increase in serum lipids was noted during treatment with quetiapine. Possible increase in cholesterol and serum triglyceride levels, decrease in thyroid hormone levels (total T4 and free T3).
Compared with other atypical antipsychotics, quetiapine is more likely to cause anticholinergic side effects.
As noted above, the medication can affect the QT segment, so caution is required when using it in conjunction with drugs that affect the conduction of the heart muscle.
Interaction with medications: quetiapine does not combine well with alcohol, thioridazine, phenytoin, carbamazepine, microsomal enzyme inducers, drugs with central activity (barbiturates), potential CYP3A4 inhibitors (ketoconazole and erythromycin).
Return to Contents
Quetiapine, 60 pcs., 200 mg, film-coated tablets
With the simultaneous use of drugs that have a strong inhibitory effect on the CYP3A4 isoenzyme (such as azole antifungals and erythromycin, clarithromycin, nefazodone), the concentration of quetiapine in plasma increases, therefore their simultaneous use with quetiapine is contraindicated. When quetiapine is used concomitantly with drugs that induce the liver enzyme system, such as carbamazepine, the plasma concentration of the drug may decrease, which may require an increase in the dose of quetiapine, depending on the clinical effect. In a study of the pharmacokinetics of quetiapine at various doses, when used before or simultaneously with carbamazepine (an inducer of liver enzymes), it resulted in a significant increase in the clearance of quetiapine. This increase in quetiapine clearance reduced AUC by an average of 13% compared with quetiapine without carbamazepine. The simultaneous use of quetiapine with another inducer of microsomal liver enzymes, phenytoin, also led to an increase in the clearance of quetiapine. With simultaneous use of quetiapine and phenytoin (or other hepatic enzyme inducers such as barbiturates, rifampicin), an increase in the dose of quetiapine may be required. It may also be necessary to reduce the dose of quetiapine when phenytoin or carbamazepine or another liver enzyme inducer is discontinued or replaced with a drug that does not induce liver microsomal enzymes (for example, valproic acid).
The pharmacokinetics of lithium preparations does not change with simultaneous use of quetiapine.
Quetiapine did not cause induction of hepatic enzyme systems involved in the metabolism of antipyrine. The pharmacokinetics of quetiapine does not change significantly when used simultaneously with antipsychotic drugs - risperidone or haloperidol. However, simultaneous administration of quetiapine and thioridazine resulted in increased clearance of quetiapine. CYP3A4 is a key enzyme involved in the cytochrome P450-mediated metabolism of quetiapine. The pharmacokinetics of quetiapine does not change significantly with simultaneous use of cimetidine, which is a P450 inhibitor.
The pharmacokinetics of quetiapine were not significantly altered by concomitant use of imipramine (CYP2D6 inhibitor) or fluoxetine (CYP3A4 and CYP2D6 inhibitor). CNS depressants and ethanol increase the risk of side effects from quetiapine.
Quetiapine-SZ
Lipid levels
While taking quetiapine, the concentration of triglycerides and cholesterol may increase (see section “Side effects”).
QT prolongation
There was no relationship between taking quetiapine and a persistent increase in the absolute value of the QT interval. However, prolongation of the QT interval was observed with an overdose of the drug (see section "Overdose"). Caution should be exercised when prescribing quetiapine, as with other antipsychotic drugs, to patients with cardiovascular disease and a history of QT prolongation. Caution should also be exercised when prescribing quetiapine concomitantly with drugs that prolong the QTC interval, other antipsychotics, especially in the elderly, patients with congenital long QT syndrome, chronic heart failure, myocardial hypertrophy, hypokalemia or hypomagnesemia (see section “Interaction with Others”). drugs").
Acute reactions associated with drug withdrawal
If quetiapine is abruptly discontinued, the following acute reactions (withdrawal syndrome) may occur: nausea, vomiting, insomnia, headache, dizziness and irritability. Therefore, it is recommended to discontinue the drug gradually over at least one or two weeks.
Elderly patients with dementia
Quetiapine is not indicated for the treatment of psychoses associated with dementia. Some atypical antipsychotics in randomized placebo-controlled trials increased the risk of cerebrovascular complications by approximately 3 times in patients with dementia. The mechanism for this increased risk has not been studied. A similar risk of increased incidence of cerebrovascular complications cannot be excluded for other antipsychotic drugs or other patient groups. Quetiapine should be used with caution in patients at risk of stroke.
An analysis of the use of atypical antipsychotics for the treatment of psychosis associated with dementia in elderly patients revealed an increased mortality rate in the group of patients receiving drugs of this group compared with the placebo group. In addition, two 10-week placebo-controlled studies of quetiapine in a similar group of patients (n = 710; mean age: 83 years; age range: 56-99 years) showed that the mortality rate in the group of patients taking quetiapine was 5. 5%, and 3.2% in the placebo group. The causes of death observed in these patients were consistent with those expected for this population. No causal relationship has been identified between treatment with Quetiapine and the risk of increased mortality in elderly patients with dementia.
Suicide/suicidal ideation or clinical worsening
Depression is associated with an increased risk of suicidal ideation, self-harm and suicide (suicide-related events). This risk persists until significant remission occurs. Because it may take several weeks or more for the patient's condition to improve from the start of treatment, patients should be under close medical supervision until improvement occurs. According to generally accepted clinical experience, the risk of suicide may increase in the early stages of remission.
Other mental disorders for which quetiapine is prescribed are also associated with an increased risk of suicide-related events. In addition, such conditions may be comorbid with a depressive episode. Thus, the precautions used when treating patients with a depressive episode should also be taken when treating patients with other mental disorders.
Patients with a history of suicidal events, as well as patients who clearly express suicidal thoughts before starting therapy, are at increased risk of suicidal intent and suicide attempts and should be carefully monitored during treatment. An FDA meta-analysis of placebo-controlled trials of antidepressants, summing up data from approximately 4,400 children and adolescents and 7,700 adult patients with mental disorders, found an increased risk of suicidal behavior with antidepressants compared with placebo in children, adolescents and adult patients under 25 years of age. This meta-analysis does not include studies where quetiapine was used (see Pharmacodynamics section).
In short-term, placebo-controlled studies across all indications and all age groups, the incidence of suicide events was 0.9% for both quetiapine (61/6270) and placebo (27/3047).
In these studies in patients with schizophrenia, the risk of suicide-related events was 1.4% (3/212) for quetiapine and 1.6% (1/62) for placebo in patients aged 18–24 years; 0.8% (13/1663) for quetiapine and 1.1% (5/463) for placebo in patients over 25 years of age; 1.4% (2/147) for quetiapine and 1.3% (1/75) for placebo in patients under 18 years of age.