Paroxetine
Paroxetine is a drug from the antidepressant group. Known since the late 1980s. Currently widely used for depression of all types (atypical, seasonal, psychotic, postpartum, dysthymia, etc.), obsessive-compulsive neurosis, episodic paroxysmal anxiety (including those associated with fear of open space), social and generalized anxiety disorders, post-traumatic stress disorder, premenstrual dysphoric disorder, chronic headaches. The antidepressant effect of the drug is determined by its ability to selectively suppress the uptake of serotonin by neurons in the brain - the so-called. “hormone of good mood” or “hormone of happiness” (in terms of the severity of this property, paroxetine is a leader among all antidepressants known today). The drug is well absorbed from the gastrointestinal tract, partially undergoing a first-pass effect through the liver with the formation of pharmacologically inert metabolites. A stable concentration of the active substance in the blood is achieved after 4-14 days of regular pharmacotherapy. The half-life of the drug is 21 hours, which makes it possible to limit the drug to a single dose per day (and this, in turn, increases compliance, i.e., the patient’s adherence to treatment). The pharmacokinetic characteristics of paroxetine vary depending on the age of the patients. The rate of elimination in persons suffering from liver and kidney diseases is reduced.
The drug has a favorable safety profile and, provided the recommended dosage instructions are followed, rarely causes side effects. Paroxetine does not suppress psychomotor processes and does not enhance the inhibitory effect on psychomotor activity of ethanol-containing products. According to a study of behavioral reactions and an encephalogram, the drug exhibits a weak activating effect when slightly exceeding the recommended doses. There are no significant changes in blood pressure, heart rate and EEG. Paroxetine is contraindicated in case of individual intolerance to the components, unstable epilepsy, during pregnancy and breastfeeding, when taking monoamine oxidase inhibitors (and for two weeks after the end of their use). The drug is not used in pediatric practice. Daily dose – 1 tablet. The optimal time to take it is in the morning, during breakfast. Dose selection is carried out on an individual basis with the possibility of further adjustment after two to three weeks from the start of pharmacotherapy. The presence of food contents in the gastrointestinal tract and the use of medications that reduce gastric acidity do not affect the pharmacokinetic characteristics of paroxetine. During drug therapy, it is recommended to abstain from drinking alcohol. Despite the fact that the drug does not affect psychomotor and cognitive functions, during treatment you should be careful when engaging in activities that require increased attention and reaction speed, incl. driving a car.
IN AND. Maksimov
Scientific Center for Mental Health of the Russian Academy of Medical Sciences, Moscow
Summary The article discusses issues related to the representative of the modern group of second-generation antidepressants - paroxetine, and its place in the treatment of depressive disorders, as well as conditions that are accompanied by an anxiety component. The summarized results of numerous studies are presented, confirming the high clinical effectiveness and favorable safety profile of the drug. It is concluded that it is possible to correct established clinical stereotypes, which will allow new drugs, in particular paroxetine, to become more widespread.
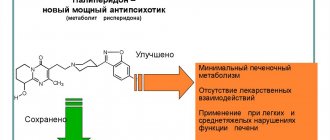
Paroxetine belongs to the selective serotonin reuptake inhibitors (SSRIs) - a modern group of second-generation antidepressants that have gained wide popularity in the treatment of depressive disorders. Common SSRIs include fluoxetine, citalopram, escitalopram, sertraline, fluvoxamine and paroxetine itself. In the light of modern neurotransmitter concepts, an increase in serotonin concentration, facilitated by blockade of postsynaptic 5-HT receptors, determines the antidepressant and anti-anxiety effect of the SSRI group. The coherent concept of these theoretical constructions is cast a “shadow” only by the phenomenon of the drug tianeptine, a serotonin reuptake activator. Tianeptine inexplicably, lowering the concentration of serotonin, has not only anxiolytic and thymoanaleptic, but even a hyperthymic effect, and therefore it is included in the list of subject-quantitative records [1, 2]. As for paroxetine, it has a unique biochemical activity: it is absorbed regardless of food intake with a digestibility above 60%, the concentration in the blood increases parabolically over 5 hours, the half-life is extended for a day, enzymatic utilization in the body does not produce active metabolites that contribute to development of a cumulative effect. At the same time, the effect of paroxetine on neurotransmitter structures is limited mainly by blocking the serotonin uptake system, bypassing other receptors responsible for severe side effects (anticholinergic, antihistamines, etc.) .). The advantages of the drug also include its low metabolic sensitivity to mild and even moderate diseases of the excretory organs; low toxicity - the lethal dose is hundreds of times higher than the therapeutic dose and, in fact, has not been determined [3]. Research into the effects of paroxetine is being conducted in two directions. The first includes studying the effectiveness of the drug in depressive disorders, the second - use in other psychopathological conditions. The first direction, in turn, is divided into two: the effect of paroxetine on individual symptoms of depression, and the comparative effectiveness of the drug among antidepressants. The second direction is also divided into two: the effect of paroxetine on non-depressive mental disorders and its use in somatic conditions.
Efficacy of paroxetine in depressive disorders Studies on this topic are the most numerous and include large cohorts of patients. For example, D. Sheehan et al. used treatment data from 2963 patients [4]. The generalized results indicate that the average therapeutic dose of the drug is 20 mg/day, maximum 60 mg/day. Immediately after the start of therapy, in some cases on the 2nd day, a thymoanaleptic effect appears. Moreover, the reduction in the depth of depression is universal and does not depend on the nosology of psychopathological manifestations, age and gender of recipients. The anxiolytic effect is somewhat more delayed, although it occurs quite quickly - during the first week of therapy. Features of the anti-anxiety effect include restoration of the correct daily sleep pattern: lack of drowsiness during the day and full sleep at night. In the third week of therapy, a mild activating effect appears, not accompanied by an exacerbation of psychopathological symptoms, physical endurance first increases, and in the fourth week the restoration of intellectual performance is reliably recorded. The full clinical effect in most cases occurs after 4 weeks of therapy [3, 4, 16]. A peculiarity of the use of paroxetine is its special significance as a 1st-line drug in the presence of comorbid anxiety-phobic disorders, as well as somatic burden with cardiovascular, endocrine diseases and pathology of parenchymal organs. Favorable reviews have been given by many researchers and practitioners for depressive states of puberty and involutionary ages, which is associated with increased sensitivity and physiological characteristics of people of these age periods. Moreover, the absence of side muscarinic effects and cumulation phenomena is given leading importance [3, 6, 7, 12]. The second subgroup of works in the first direction is devoted to the comparative effectiveness of paroxetine with other antidepressants, mainly TCAs and MAOIs. Compared to TCAs, paroxetine has less activity, but only in severe, psychotic conditions. At the initial stages of the development of depression, as well as in mild and even moderate degrees of the disease, some researchers note a greater effect from treatment with SSRI drugs compared to TCAs. Absence of anticholinergic (dry mouth, blurred vision, difficulty urinating, constipation, memory impairment, exacerbation of cornerstone glaucoma), antihistamine (sedation, weight gain), alpha-adrenolytic (orthostatic hypotension), cardiovascular (sinus tachycardia, arrhythmias, slowing of myocardial conductivity) and other (sexual dysfunction, impaired cognitive and psychomotor processes, convulsive states) actions characteristic of TCAs make the use of paroxetine preferable in many cases [3, 8]. Comparing paroxetine with MAOIs is difficult due to the heterogeneity of the latter. Irreversible MAOIs due to the presence of a “cheese” effect - hypertensive crisis when consuming foods containing tyramine (cheese, cream, smoked meats, legumes, beer, coffee, red wines, yeast, chocolate, liver, bananas - an impressive list), hepatotoxic and gross stimulant actions were not compared with SSRIs. As for reversible MAOIs, there is an opinion that their pharmacological activity is comparable to TCAs, i.e. higher than that of paroxetine, but is accompanied by anticholinergic and cardiovascular side effects. A special issue is the combination of drugs from both groups, which is very risky, leading to the development of “serotonin” syndrome, which will be discussed below. If there is a need to switch from SSRI drugs to MAOIs, a “wash-out” period of 5 weeks is recommended [8, 14, 17].
The use of paroxetine in non-depressive disorders The effect of SSRI drugs on non-depressive mental disorders has been studied mainly in conditions in which anxiety is a significant component. Paroxetine has been used successfully for panic disorder, social phobia, specific phobias, generalized anxiety disorder, obsessive-compulsive disorder and post-traumatic stress disorder. Studies conducted on large groups of patients (from 100 to 1000 people) have shown significant effectiveness of paroxetine. It is prescribed in an average therapeutic dose of 40 mg/day, a maximum therapeutic dose of 60 mg/day. In the second week, a noticeable effect occurs; the course of treatment until a significant reduction in symptoms is achieved is 3 months. After active treatment, such patients usually require fairly long-term maintenance therapy of 20-40 mg/day for 6 months. The effect of paroxetine is significantly more effective than that of clomipramine, a powerful non-selective serotonergic drug, benzodiazepine tranquilizers and reversible MAOI antidepressants. During therapy there are no side effects, signs of addiction or dependence, drinking alcohol does not reduce the effect of the drug. The only weak point of paroxetine is its somewhat delayed action compared to tranquilizers [5, 6, 7, 9]. The experience of using paroxetine in the clinic of somatic diseases has shown the advisability of its use in somatic disasters: strokes, myocardial infarction, hypertensive crises, both in the acute period and in residual phenomena, i.e. in conditions other than somatic ones that include a component of panic or anxiety. The drug is prescribed in an average therapeutic dose of 20 mg/day for 2-3 weeks. Signs of anxiety disappear around the end of the first week of therapy. Researchers attribute the simultaneous positive effect on symptoms of anxiety and lethargy to the peculiarities of the use of paroxetine in somatic practice [11, 13]. In addition to descriptions of psychotropic effects, there are references to the somatotropic activity of the drug. Thus, in patients who have suffered a myocardial infarction, paroxetine has a parasympathetic effect, reducing the risk of ventricular arrhythmias, and patients with bronchial asthma show an increase in bronchial patency [10, 11]. Among the drugs of the SSRI group, paroxetine occupies a place that is characterized by the most balanced effect with a predominance of the anxiolytic effect, which is reflected in the diagram below (Fig. 1). A comparison of some parameters of the most well-known SSRIs is given in the table (S. Puzinski, 1995). As can be seen from the table, the most active drug with accumulation phenomena and the formation of a psychotropic metabolite, stimulating the exacerbation of productive symptoms, is fluoxetine, which requires caution in its use, in contrast to the mild action of paroxetine. Side effects with the use of paroxetine are infrequent and are represented by dyspeptic disorders and isolated cases of hypomania without convincing evidence that hyperthymic symptoms developed as a result of exposure to the drug, and not as part of a change in the phase of the underlying disease [15]. A serious and occasionally fatal complication is the possibility of developing “serotonin” syndrome (SS) with combined therapy of SSRIs and MAOIs, SSRIs and TCAs, SSRIs and tramadol, SSRIs and lithium salts, SSRIs and carbamazepine. This syndrome manifests itself in the form of symptoms of gastrointestinal tract disorders (various dyspeptic phenomena), central nervous system damage (extrapyramidal phenomena, myoclonic convulsions), manic-like disorders, disorders of consciousness (confusion). At the height of its development, CV resembles neuroleptic malignant syndrome, and possible death occurs from acute cardiovascular disorders. Although SS has been described only during fluoxetine therapy, caution should also be exercised during treatment with other SSRI drugs [17]. Finally, there are reports of a possible teratogenic effect of paroxetine when used in the first three months of pregnancy. This effect allegedly can manifest itself in the form of various heart defects with a probability of 1.5-2%. It is planned to study all SSRI drugs to determine their effect on the human fetus. On the other hand, many experts advise the use of SSRIs as the drug of choice, compared with TCAs and MAOIs, during pregnancy [18, 19, 20]. In conclusion, a diagram of the psychotropic profile of paroxetine is provided in comparison with typical TCAs - amitriptyline, and selective MAOIs - pyrazidol (Fig. 2). Despite the obvious advantages of new antidepressants (in particular, paroxetine) over TCAs in certain clinical situations, in Russia, until recently, “old” antidepressants were used to treat most patients. One of the leading reasons for this is the clinical stereotypes developed over the years, which are deeply rooted in the minds of specialists. In addition, a serious limiting factor in the widespread use of new tools was their high cost. But the situation is changing. Year after year, more and more new drugs are becoming more accessible to most patients. It is these requirements that the new antidepressant Plizil (paroxetine), produced by Pliva (Croatia), satisfies.
Literature 1. Encyclopedia of drugs. M.: 2008;1500. 2. Order of the Ministry of Health and Social Development of the Russian Federation dated October 13, 2006 N 703 “On amendments to the order of the Ministry of Health and Social Development of the Russian Federation dated December 14, 2005 No. 785.” 3. Gurovich I.Ya., Shmukler A.B. The place of Paxil (paroxetine) among other antidepressants and clinical and social aspects of its use // Russian Medical Journal. 2007; 5: 67-85. 4. Sheehan D., Dunbar GC, Fuell D. The effect of paroxetine on anxiety and agitation associated with depression // Psychopharmacol. Bull. 1992; 28:2:139-143. 5. Nemeth A., Agoston G. The efficacy of paroxetine in the treatment of anxiety disorders. // Gyуgyszereink. 2002; 52: 46-49. 6. Baldwin D., Bobes J., Stein DJ, Scharwächter I., Faure M., on behalf of the Paroxetine Study Group. Paroxetine in social phobia/social anxiety disorder. Randomised, double-blind, placebo-controlled study. // Br. J. Psychiatry. 1999; 175: 120-6. 7. Mosolov S.N. Clinical use of modern antidepressants. St. Petersburg: 1995; 568. 8. Drobizhev M.Yu. Treatment of depression in the general somatic network // Psychiatry and psychopharmacology. 2004; 5:5:190-193. 9. Voloshin V.M. Typology of chronic post-traumatic stress disorder // J. neurol. and a psychiatrist. them. Korsakov. 2004; 1: 104: 17-23. 10. Drobizhev M.Yu. et al. Paroxetine in the treatment of depressive and anxiety-phobic conditions in patients with bronchial asthma (pilot study). // Pulmonology. 2002; 12:3:55-63. 11. Trofimova O.V. and others. Treatment of anxiety depression with Paxil (paroxetine) in patients in the early post-infarction period // Attending physician. 2003; 7: 113-7. 12. Artyukh V.V. Antidepressant effect of paroxetine (Paxil) in adolescent patients // Psychiatry. 2005; 2: 14-17. 13. Podkorytov V.S. et al. Paroxetine in the treatment of anxiety and depressive disorders in somatic patients // Medicus Amicus. 2006; 1: 112-4. 14. Puzhinsky S. Pharmacotherapy of depressive states. // Depression and comorbid disorders / Ed. Smulevich A.B. M.: 1997; 220. 15. Morishita Sh., Aritab S. Prevalence of induced manic syndrome in patients treated with milnacipran: comparison with paroxetine (extended abstract) // Psychiatry and psychopharmacotherapy. 2007; 09:1:11-12. 16. Shafer M.S. and others. Experience of clinical use of paroxetine (Paxil) in the treatment of depressive disorders in a psychiatric hospital // Psychiatry and psychopharmacotherapy. 2000; 01:1:19-20. 17. Mosolov S.N. and others. Serotonin syndrome in the treatment of depression. // International Journal of Medical Practice. 2000; 8: 56-59. 18. Louik C. et al. First-Trimester Use of Selective Serotonin-Reuptake Inhibitors and the Risk of Birth Defects // N. Engl. J. Med. 2007; 356:2675-83. 19. O'Brien L., Bar-Oz B., Einarson T. et al. Paroxetine and congenital malformations: meta-analysis and consideration of potential confounding factors // Clin. Ther. 2007; May: 29: 5: 918-26. 20. Ushkalova E.A. Pharmacotherapy of neuropsychiatric diseases in pregnant women // Farmateka. 2003; 4: 67: 18-21.