Fetal hypoxia is a dangerous pathological process characterized by reduced oxygen supply to the fetus.
Hypoxia occurs due to atypical processes occurring in the female body. The time of formation, course and intensity of symptoms directly affect the development and general health of the child. Treatment of hypoxia must be carried out as early as possible so that the disease does not cause irreparable consequences.
Hypoxia can be diagnosed at any stage of pregnancy. The sooner intrauterine fetal hypoxia occurs, the more seriously it will affect the development of the child (both mental and physical). It can also cause damage to the central nervous system, but this is in case of untimely or improper treatment. Medical statistics show that oxygen deficiency occurs in 10-15% of all pregnancies. Treatment in this case is primarily aimed at normalizing blood flow to the uterus and placenta, but in case of acute fetal hypoxia, it is recommended to induce labor artificially rather than using any treatment methods.
Intrauterine fetal hypoxia
The causes of intrauterine fetal hypoxia are various pathologies occurring in the maternal body, as well as unfavorable environmental factors. Hypoxia can occur due to diseases:
- hypertension
- diabetes
- heart disease
- preeclampsia and eclampsia
- chronic bronchitis or bronchial asthma
- various kidney diseases
Intrauterine causes of hypoxia:
- damage to the integrity of the uterus
- prolonged compression of the child’s head and neck during childbirth
- complication of the baby’s passage through the birth canal, most often due to large volumes or incorrect position of the baby
- increase in amniotic fluid volume
- pregnancy with two, three or more fetuses
- intrauterine infection of a child
- obstruction of the birth canal from the uterus by the placenta
- wrapping the umbilical cord around the baby's neck
- disruption of blood flow in the placenta
In addition, external factors :
- poor ecology and high air pollution in the place where the expectant mother lives
- taking a large number of medications
- chemical poisoning
- abuse of alcohol, nicotine or drugs by a woman during pregnancy
Degrees of fetal hypoxia
Based on the rate of progression, hypoxia is divided into:
- short-term, i.e. occurs quickly and unexpectedly
- moderate severity – expressed directly during childbirth
- acute – signs of the disease are observed several days before the upcoming birth
- chronic fetal hypoxia - it appears with severe toxicosis, incompatibility of blood groups or Rh factors of the mother and child, intrauterine infections of the fetus.
according to the time of occurrence :
- formed in the first months of pregnancy
- in the second half of the allotted time
- during childbirth
- occurs very rarely after childbirth.
What consequences can a lack of oxygen in the blood have in a pregnant woman?
The consequences of hypoxia depend on the duration and time of manifestation. In the first trimester, it can cause fetal growth retardation. Internal organs form late, which can lead to internal defects. Chronic hypoxia can cause acute asphyxia and even fetal death.
A lack of oxygen in the blood of a pregnant woman can cause placental abruption, placenta previa, and preeclampsia. These are very serious diagnoses, dangerous for both mother and child. Treatment in this case is carried out exclusively in a hospital setting.
Symptoms of fetal hypoxia
Hypoxia is quite difficult to determine, since it can appear suddenly. But it is very important to diagnose hypoxia in the early stages, because this will allow you to quickly begin treatment and avoid consequences.
The main symptom of fetal hypoxia is a slow heartbeat , but this cannot be noticed at home. The first sign to consult a doctor is a change in the intensity of fetal kicks . Every woman feels movement, but if the child makes itself felt less than three times a day, you should immediately contact a specialist, because this indicates chronic intrauterine fetal hypoxia.
The acute form, which occurs suddenly, is characterized by completely opposite signs - the child is too active, pushing hard.
Signs of fetal hypoxia in the first three months of pregnancy are very difficult to determine, so it would be better for the woman and the fetus to be examined by a doctor weekly.
Diagnosis of hypoxia
Children diagnosed with perinatal posthypoxic damage to the central nervous system are observed by a neurologist for 2 years. After this period, the diagnosis is removed or changed to a more complex one (cerebral palsy, hydrocephalus, etc.).
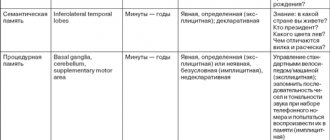
Methods for diagnosing post-hypoxic state:
- Ultrasound of the brain showing the anatomy of the nervous system
- electroencephalogram (EEG) characterizes neuronal function
- Dopplerography of cerebral vessels characterizes the functions of cerebral vessels, with what speed and symmetry they work and how well they deliver oxygen to the brain.
- MRI is extremely rarely performed on children in the first 2 years, as anesthesia is required for this study.
Ultrasound of the brain reveals the following post-hypoxic changes:
- Cysts (appear after 10-14 days after hypoxia).
- Deformation of the gyri and sulci of the brain.
- Periventricular leukomalacia - necrosis of brain cells around the ventricles of the brain, is an extremely unpleasant symptom in terms of prognosis, often ending in hydrocephalus and cerebral palsy.
- An increase in the size of the cerebral ventricles, interhemispheric fissure and other liquor-containing spaces.
The frequency of studies in children who have suffered hypoxia is once every 3 months to a year and once every 6 months. in the second year of life.
The Apgar score is not the only criterion for hypoxia. For example, in a fetus, in response to a lack of oxygen, the rectal sphincter opens and meconium enters the amniotic fluid, causing it to turn green. Oxygen starvation may also be indicated by the condition of the placenta (premature aging, abnormal development of blood vessels, etc.). Sometimes such children are born with a high Apgar score, but hypoxia still occurs.
The brain of children in the first 2 years of life is very plastic and gladly accepts all treatment methods, responds quickly and produces excellent results. Recently, osteopathic treatment has taken a well-deserved place in the treatment program for children who have suffered from hypoxia.
Consequences of fetal hypoxia
If you ignore symptoms or contact a doctor late, hypoxia seriously threatens the health and development of the fetus.
Complications of chronic fetal hypoxia can include:
- disorders of the development and formation of internal organs, bones and brain of the fetus
- intracellular edema
- internal hemorrhages
- delayed fetal development
For a newborn child, the consequences are no less serious:
- changes in the structure and structure of some internal organs; hemorrhages
- inability to independently perform functions characteristic of the first days after birth
- neurological diseases
- mental retardation
- psychical deviations
- Cerebral palsy and autism
Acute and chronic fetal hypoxia can lead to fetal death in the womb or death of the child during the first week of life.
Hypoxia in newborns and older children
Hypoxia (or oxygen starvation) is a fairly common pathology that occurs in children of all ages and especially in newborns.
In newborns, hypoxia is often provoked by diseases of the mother, which affect the intrauterine development of the child and complicate the birth process. These include problems with the circulatory system, heart failure, unhealthy lifestyle - smoking, alcohol, taking drugs prohibited during pregnancy - and much more. If a pathological birth is added to the child’s hypoxia, which arises from the mother’s illnesses, then the degree of hypoxia can increase many times.
In this article we will consider the initial manifestations of insufficient blood supply to the brain.
Damage to the cervical spine, perinatal encephalopathy, asphyxia and other diagnoses can be given to the child immediately after birth, which will be common causes of the development of cerebral hypoxia. Parents most often come to a pediatric neurologist or other specialized specialist when the child’s nervous system receives increased stress - the diagnosis is made immediately before school or in first grade. Moreover, according to experts, the number of such children today is 70-80%. The most common complaints from parents are:
- emotional lability of your child and weather dependence;
- high nervous excitability;
- speech dysfunction of varying degrees;
- difficulties with learning and concentrating;
- bad behavior;
- headaches and dizziness;
- visual impairment, etc.
Despite the fact that cerebral hypoxia as a result of vascular disorders is very often diagnosed in schoolchildren, its first symptoms can be noticed in the first year of a child’s life. Such children, literally from the first days, are characterized by increased excitability, they have sleep and appetite disturbances, increased muscle tone, and suppression of unconditioned reflexes.
The main and most common cause of hypoxia in children is birth trauma. Rapid labor, stimulation of labor, and cesarean section are a trigger for weakening one or another function of the child’s body, resulting in symptoms characteristic of vascular disorders. While moving through the birth canal, the baby's cervical region experiences enormous stress, which can cause displacement of the cervical vertebrae and lead to disruption of the blood supply to the brain.
No less common and dangerous is compression, deformation and damage to the bones of the skull. All this directly affects the membranes of the brain and the blood circulation and oxygen supply.
The nervous system, together with the muscular, skeletal, circulatory and other systems, is part of a single whole organism, and disruptions or changes in function and structure in one of them always cause failure in the others. Therefore, vascular disorders of the brain are always a complex of disorders and symptoms, characterized by individuality for each child. And if your child has some of these manifestations, it is advisable not to delay a visit to specialists.
Treatment of a child with hypoxia should always be comprehensive: the main thing in the process of treating vascular disorders is a favorable atmosphere in the family, a regime and corrective measures that contribute to the child’s recovery, observation by a neurologist, speech therapist, orthopedist and other specialists. Osteopathy has proven itself well in the treatment of hypoxia, since the osteopath, during correction, considers the child’s body as an integral system.
It is a mistake to believe that an osteopath will cure all diseases and forever relieve your child of all adaptive symptoms of vascular disorders of the brain, make him a good student and a successful person in life. Osteopathy only makes some changes, affecting the vascular and nervous systems, the child’s circulatory system and other systems. Since the most common cause of hypoxia is a traumatic injury that provokes impaired blood circulation in the brain, an osteopath must find the main source of the problem and restore these processes using gentle techniques. Osteopathic correction is especially effective in cases where the cause of the disorder lies in the displacement of the vertebrae, block of the sutures of the vault and base of the skull, or injuries of the cervical spinal column. After all, the blood supply to the brain depends on the correct location of the meninges, skull bones and vertebrae and the possibility of free micromovements. During treatment, positive dynamics are not immediately observed. An osteopath can work with both large organs, bones and muscles, and very subtle matters and not only heals them, but directs the child’s body to independent adaptation and correction of congenital and acquired disorders.
It is desirable that osteopathic treatment be combined with a complex of other therapeutic and preventive measures, including physical therapy, constant classes and exercises with the child, work on his upbringing, etc. For example, if the blood circulation in the speech areas of the brain is impaired, the child may pronounce words or letters incorrectly. With osteopathic treatment, restoration of blood supply to these areas will improve the condition of damaged neural connections, and the child’s speech apparatus will have more opportunities to adapt to the new conditions of the body. This moment will be the most fruitful if you work with the child, instilling in him the correct pronunciation. As a result of regular classes, he will learn to speak and think correctly without outside help. We can observe the same processes with disorders in physical development, psychological state, etc.
It is obvious that the mechanical consequences of injury cannot be eliminated with any medications. An osteopath has a large variety of soft manual techniques in his arsenal, which can be used to eliminate the root cause and thereby remove obstacles to good blood circulation and cerebrospinal fluid flow. And the body will then begin to work on its own, because... The self-healing process will begin.
Osteopathic sessions for children with vascular disorders of the brain are usually prescribed once a week and last no more than 30-60 minutes. The duration of the therapeutic course is selected individually in each case. As a rule, after four to five sessions it is possible to normalize the patient’s condition and create the conditions necessary for the proper development of his body. Therefore, if it is important for parents not to let mild hypoxia of their child’s brain turn into more severe forms, it is advisable to see a specialist if there are any abnormalities.
GET A FREE CONSULTATION BY PHONE
+ 7 (495) 114-14-95
How to determine fetal hypoxia
Determining fetal hypoxia starting from the fifth month of pregnancy is not difficult. It is much more difficult to do this in the first 3 months, but the earlier the diagnosis is made, the higher the likelihood of avoiding the consequences of the disease.
Diagnosis of fetal hypoxia consists of:
- Using special gynecological diagnostic techniques, the transparency, color and amount of amniotic fluid is assessed
- Doppler ultrasound, which allows you to track the speed of blood flow in the umbilical cord and placenta
- Ultrasound
- CTG
- listening to heart rate through a stethoscope
- monitoring the intensity of fetal movements
Symptoms and diagnosis
It is extremely difficult to detect hypoxia in the first months of pregnancy. Only a few objective factors (low hemoglobin, diabetes mellitus, smoking, etc.) can suggest its presence.
A reliable diagnosis can be made after 18 weeks of pregnancy, when the fetus begins to move in the uterus. The greatest suspicions are caused by changes in his motor activity, rapid or slow heartbeat.
The expectant mother needs to pay attention to the following manifestations:
- prolonged absence of the baby's movements;
- increased fetal activity (frequent movements);
- change in the nature of the child’s motor activity. For example, the movements were rare, and then suddenly became more frequent. Or, on the contrary, the baby was actively moving, and then suddenly stopped.
In all of the above cases, you should immediately consult a doctor.
CTG is performed several times during the 3rd trimester of pregnancy and during childbirth
Diagnostic methods
Hypoxia is diagnosed using the following methods:
- Ultrasound - performed after 18 weeks of pregnancy;
- CTG (cardiotocography) - performed after 30 weeks of pregnancy and during childbirth and consists of recording and analyzing the fetal heart rate during movement, rest, and contractions;
- Doppler testing is a type of ultrasound diagnostics and is performed after 18 weeks of pregnancy upon the direction of a doctor. The intensity of blood flow in the vessels of the fetus, uterus and placenta is assessed;
- amnioscopy - performed in late stages (after 37 weeks) by inserting a special device - an amnioscope - through the cervix. The method allows you to assess the condition of amniotic fluid (quantity, color and the presence of impurities in it) and the amniotic sac.
Indicators that indicate oxygen deficiency:
- the fetus is smaller in size and weight than normal for a given period of pregnancy, which indicates developmental delay;
- polyhydramnios or oligohydramnios;
- fetal heartbeat disturbance;
- disruption of blood flow in the vessels of the uterus, placenta and umbilical cord;
- The color of amniotic fluid is green and contains meconium (usually diagnosed during childbirth).
Treatment of fetal hypoxia
At the first manifestation of symptoms of fetal hypoxia, a pregnant woman is immediately hospitalized. The first thing treatment is aimed at is stabilizing the oxygen supply to the fetus and reducing the tone of the uterus. To do this, the patient is prescribed strict bed rest and medications that will improve oxygen permeability and metabolism. Oxygen therapy and hyperbaric oxygenation (pressure chamber) are also often prescribed, which increases blood oxygenation not only in the mother’s body, but also in the fetus.
When the first improvements in the condition of the fetus are observed, the woman can perform gymnastics, various breathing exercises, and attend aqua gymnastics. If no measures to normalize the supply of oxygen to the fetus have had the desired effect or symptoms of fetal hypoxia persist for more than twenty-eight weeks of pregnancy, it is best to immediately perform a cesarean section. In case of acute hypoxia, a newborn child requires the help of a resuscitator.
Causes of hypoxia
There are many factors influencing the development of hypoxia:
- chronic diseases of women and weakened immunity;
- immoral lifestyle, abuse of alcohol, nicotine, drugs.
This negatively affects not only the overall health, but also the formation of the fetus, blood flow and other life support systems.
Also among the reasons:
- Rhesus conflict;
- infectious diseases during gestation;
- developmental anomalies;
- incorrect location of the umbilical cord (entanglement, prolapse);
- long-term toxicosis, gestosis;
- multiple pregnancy;
- oligohydramnios, polyhydramnios;
- pathologies of the placenta;
- psychological factor: severe stress and neuroses;
- abnormal structure of the uterus and reproductive organs;
- poor nutrition;
- negative environmental situation;
- use of sedatives and anesthesia during delivery.
It is advisable to plan pregnancy. This allows you to identify possible threats and risks. One of the most important points is constant monitoring by a gynecologist during pregnancy.
The gynecologist carefully examines the medical history and asks the woman about her health and any changes. Hypoxia detected in time can be treated if it is not an acute form.
Prevention of fetal hypoxia
Prevention of fetal hypoxia should be carried out by a woman who has decided to become a mother, namely:
- choose the right way to give birth to a child. A caesarean section is less likely to cause fetal hypoxia than a natural birth.
- timely treatment of diseases that accompany pregnancy
- avoid strong physical exertion, only breathing exercises
- get enough rest
- rationalize your diet by consuming plenty of vitamins and calcium
- lead a healthy lifestyle, give up alcohol, nicotine and drugs
- be regularly observed at the antenatal clinic
- register with an obstetrician-gynecologist on time
- plan pregnancy and carefully prepare for it, through examination by doctors, treatment of chronic, infectious or gynecological diseases
There are many studies related to the treatment of fetal hypoxia. One of them is the use of barotherapy in the treatment of fetal hypoxia.