In this article, medical doctors will help you understand the symptoms of stroke and micro-stroke and tell you what to do if a person has an attack.
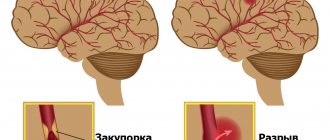
A stroke is a cerebrovascular accident that causes a blood vessel to become blocked or ruptured when a blood clot disrupts the flow of blood to the brain. Brain cells die from lack of nutrition and oxygen, which leads to impaired speech, cognitive and motor functions. If a person does not receive timely assistance, death occurs within 2–3 hours.
Symptoms of a stroke
- Sudden clouding of consciousness. Slurred thoughts, confusion and delirium of speech, difficulty understanding speech.
- Vision problems - blind spots, blurred vision.
- Impaired coordination and balance. The gait may look strange, as if the person has weakness in one or both legs, difficulty moving in space, lost, or dizzy.
- Facial asymmetry: one side of the face relaxes, a person cannot smile from both corners of the mouth.
- Weakness in arm and leg on one side. Ask the person to raise both arms straight in front of them and to the sides.
- A sharp, severe headache for no apparent reason.
A stroke develops quickly. A person himself can identify symptoms within a minute and call for help. If you see the above symptoms in a person near you, immediately call an ambulance and provide first aid.
Manifestations of stroke
Subarachnoid hemorrhage manifests itself as a sudden sensation of a blow to the head (sometimes it is compared to a blow from a dagger), severe headache (at the same time the person screams in pain and even loses consciousness), there may be convulsions, but consciousness is usually restored. The patient is drowsy, lethargic, groans in pain, and holds his head with his hands. A severe headache does not allow the patient lying on his back to bend his head and touch his chin to his neck. Vomiting and nausea often occur. But, unlike hemorrhage with the formation of a cerebral hematoma, such a patient does not have paralysis.
With a hemorrhagic stroke in the cerebral hemisphere with the formation of an intracerebral hematoma, the manifestations are violent: against the background of a hypertensive crisis, a headache appears or significantly intensifies, often in one half of the head, then the patient loses consciousness, the face becomes bluish or red, breathing is hoarse, and frequent vomiting occurs. After some time, a convulsive attack may develop with a predominance of convulsions on one half of the body. If the patient regains consciousness, his limbs become paralyzed. Speech disturbances (aphasia) may also appear. Sometimes the patient does not understand the speech of others. He is like a foreigner in a state whose citizens speak a language unfamiliar to him. Often such patients forget how to read and write. Some patients develop pronounced mental abnormalities (does not know how old he is, where he is, does not recognize his loved ones, considers himself completely healthy, etc.). Sometimes vision is upset, coordination of movements and stability when standing and walking, breathing rhythm are impaired, and swallowing becomes difficult. With a hemorrhagic stroke in the brainstem, patients do not live for more than 2 days and die without regaining consciousness.
Manifestations of ischemic stroke are similar, but less clear, increasing gradually or “flickering.”
If symptoms of brain damage last less than 24 hours and then disappear completely, it is not a stroke. Such cerebrovascular accidents are called transient or (foreign term) transient ischemic attacks. Nevertheless, this is a serious signal about the possibility of developing persistent cerebrovascular accidents. But if the focal neurological symptoms are persistent, that is, they persist after a day, we can already talk about a brain catastrophe.
Recognizing an acute cerebrovascular accident is not difficult when there is severe paralysis, disorders of consciousness and speech, it is more difficult with transient disorders, but there should be one tactic - hospitalization by ambulance, if the patient is not very old and not in a coma.
Symptoms of a microstroke
- Sharp and severe headache.
- Sudden memory loss, difficulty understanding and constructing speech.
- Loss of balance and coordination.
- Numbness in an arm or leg, numbness in one part of the face.
- Severe sound and photophobia.
In case of a micro-stroke, a person can be helped within 4 hours. It is necessary to seek help as soon as possible - either go to the vascular center or call an ambulance.
65% of patients subsequently develop a full-fledged stroke after a mini-stroke, so it is necessary to promptly treat and restore normal blood circulation in the brain.
Stiffness of the leg muscles. Symptoms and treatment
Tension can be associated with prolonged stay in one position and poor circulation. The pathological condition caused by the disease is associated with excessive excitability of the neurons of the anterior horns of the spinal cord.
Types of voltage:
- Spastic. Causes the tone of individual muscles and spreads unevenly.
- Rigid. It affects all muscles at once and causes difficulty walking.
There are many serious illnesses in which rigidity is a symptom. These may include stroke, spinal injuries, inflammation in the brain, nerve disorders, as well as congenital cerebral palsy and phenylketonuria.
Stroke
A stroke causes severe damage to the central nervous system and disruption of communication between the muscles and the brain. As a result, painful, spastic contractions occur, making it difficult to perform normal daily activities. To restore damaged connections, you need to perform special exercises. Taking medications that stimulate the muscular and central nervous systems, as well as massage, contribute to successful recovery.
Hypoxia
Hypoxia – low oxygen content in tissues. The cause of muscle tissue hypoxia is the low activity of mitochondrial enzymes, which leads to impaired cellular respiration. The cause may be a lack of B vitamins, as well as poisoning with heavy metals and microbial toxins. One of the symptoms is parkinsonism, or shaking palsy. Treatment is carried out by taking drugs that perform the function of the missing enzymes.
Cerebral palsy
Cerebral palsy manifests itself in the form of delayed motor development, convulsions and epileptic seizures. The mild form is very difficult to identify, so observation by a neurologist is necessary at an early age.
The main causes of the pathology:
- violation of the development of the cerebral cortex;
- fetal hypoxia, ischemic brain damage during childbirth;
- jaundice caused by Rh conflict between mother and newborn;
- intrauterine infection, such as herpes virus;
- poisoning of a child during childbirth.
Phenylketonuria
Phenylketonuria is a hereditary disease associated with the inability to break down the amino acid phenylalanine. Since the liver lacks the enzyme phenylalanine 4-hydroxylase, it is converted not into tyrosine, but into byproducts that damage the brain. This leads to disruption of nerve impulse conduction, rigidity and developmental delays. A child can grow up healthy with timely diagnosis and exclusion of animal proteins from the diet.
Brain injuries
In case of brain injury, a person experiences:
- memory loss;
- Strong headache
; - spontaneous reflexes;
- muscle spasms.
This is caused by increased arousal and damage. To make a diagnosis, an MRI, X-ray, or, in case of severe traumatic brain injury, a lumbar puncture should be done. After a thorough examination and determination of the cause of muscle stiffness, the patient is prescribed a pastel regimen, as well as taking absorbent agents.
Spinal cord injuries
Spinal injuries can result in vertebral fragments being pushed into the spinal cord. Damaged cells do not receive enough oxygen and die. With significant damage, the process of apoptosis, that is, programmed cell death, is triggered, causing rupture of the spinal cord. After this, the ability to move is temporarily lost, since the body supports the functioning of only vital systems. To avoid complete atrophy of the lower extremities it is necessary:
- immediate surgical intervention;
- administration of drugs that stimulate damaged cells;
- supporting muscle function with electrical impulses.
Sclerosis
Sclerosis causes destruction of the myelin sheaths of neuron axons. As a result, the innervation of muscles, including the lower extremities, is disrupted, and rigidity occurs. In this case, there is poor coordination of movements and severe pain when straightening the leg. Tendon reflexes are especially strong. The patient cannot bend or straighten his legs normally, and his gait becomes wooden.
Nerve impulse conduction disorder
Occurs when nerves are injured. It can also cause muscle stiffness due to neuropraxia, which is a dysfunction of the nerve. Basically, there is a disorder of motor function. Timely diagnosis and surgery using microsurgical techniques help restore nerve function and get rid of nerve impulse conduction disorders.
Meningitis
The disease is associated with inflammation of the membranes of the spinal cord and brain. Penetrating infection causes the development of bacteria:
- meningococci;
- streptococci;
- staphylococci;
- Pseudomonas aeruginosa.
Rigidity manifests itself in the form of Kernig's sign, when a spasm of the knee joint occurs and the patient is unable to straighten the leg.
Encephalitis
Encephalitis is an inflammation of the brain. May be caused by viruses and bacteria. One of the symptoms is muscle rigidity of the lower extremities, manifested by parkinsonism, spasms and convulsions. Encephalitis is difficult to detect due to its asymptomatic early stages. Slight drowsiness and increased fatigue quickly turn into mental disorders and impaired muscle tone.
Treatment
Regardless of the cause, stiffness is treated in two stages:
- elimination of the disease;
- treatment of muscle spasms.
Daily physical exercise will be an excellent prevention and will help treatment.
Surgery is required for serious injuries to the brain and spinal cord, as well as when drug treatment fails. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
What to do if a person has a stroke?
- First of all, call an ambulance. Sometimes the minutes count.
- Provide fresh air, open windows and doors, and free the person’s neck from constricting clothing.
- Leave the person where the attack occurred. The patient cannot be moved.
- Elevate the person's head and upper body 30 degrees by placing several pillows under the thoracic spine.
- If vomiting occurs, turn the person's head to the side and ensure that the vomit passes away so that the person does not suffocate.
- In the event of an epileptic attack, carefully hold the person, turn his head to the side and insert an object wrapped in cloth into his mouth - a stick, a comb, a spoon.
- In case of cardiac arrest, immediately begin compressions through the chest and perform artificial respiration.
- Wait for the ambulance.
Dangerous age and consequences of stroke
After age 55, the risk of stroke increases significantly. For men, the most dangerous age is considered to be from 45 to 55 years, since during this period they have a stroke 2 times more often than women.
If a person can be saved, the stroke still does not go away without leaving a trace. The person may be left partially paralyzed and lose control of urination and bowel movements. Cognitive functions decrease—problems with memory, speech, and information perception appear.
Recovery after a stroke is possible, but it often requires a lot of time and effort from both the patient and his loved ones. Therefore, it is better to prevent a stroke than to deal with its consequences later.
How to avoid stroke and mini-stroke?
Stroke and its precursor, microstroke, are most often caused by features of a person’s lifestyle. The risk of developing an attack increases:
- Hypertension.
- High cholesterol.
- Diabetes.
- Overweight.
- Smoking, drinking alcohol and drugs.
- Cardiovascular diseases.
- Atherosclerosis of cerebral vessels.
This can be avoided if you undergo preventive examinations on time, treat chronic diseases and modify your lifestyle. Giving up bad habits, losing weight and maintaining normal blood pressure are the three main steps towards healthy blood vessels.
At the medical level, you can visit a general practitioner, cardiologist and neurologist, as well as undergo a Holter study and 24-hour blood pressure monitoring. If you are already worried about health problems, do not expect a miracle - consult a doctor to avoid serious consequences.
Call the number listed on the website and make an appointment with a doctor today!
Spinal stroke
Symptoms occur suddenly within a few minutes, less often - hours. Ischemic spinal stroke in some cases has a prodromal period in the form of episodes of intermittent claudication, paresthesia, periodic pain in the spine, symptoms of radiculitis, and transient pelvic disorders. At the onset of the disease, a gradual increase in symptoms is possible. Pain syndrome is uncharacteristic; on the contrary, damage to the sensory areas of the spinal cord leads to the disappearance of pain sensations noted during the precursor period.
Manifestation of hematomyelia occurs after injury to the spine, physical activity, and is accompanied by a rise in body temperature. Acute dagger pain in the spinal column is typical, radiating to the sides, often taking on a girdling character. Hematorahis occurs with irritation of the meninges, the spread of the process to the membranes of the brain causes the appearance of cerebral symptoms: cephalalgia, dizziness, nausea, depression of consciousness.
Spinal stroke is characterized by a large polymorphism of the clinical picture. Neurological deficit depends on the localization and extent of the process across the diameter of the spinal cord and along its length. Movement disorders are characterized by flaccid peripheral paresis at the level of the lesion, central spastic paresis below the affected segment. Peripheral paresis is accompanied by muscle hypotonia, hyporeflexia, and subsequently leads to muscle atrophy. With central paresis, spastic muscle hypertonicity, hyperreflexia, and possible formation of contractures are observed. Localization of the affected area in the cervical segments is manifested by flaccid paresis of the upper extremities and spastic lower extremities, in the thoracic segments - central lower paraparesis, in the lumbosacral segments - peripheral paraparesis.
Sensory disturbances occur below the level of the lesion and depend on the location of the stroke focus across the spinal cord. With an extensive spinal stroke with pathological changes throughout the entire spinal diameter, loss of all types of sensitivity, pelvic disorders, and bilateral motor deficits are noted. Involvement of half the diameter leads to the development of Brown-Séquard syndrome: motor disturbances and loss of deep sensitivity are detected homolaterally, and disturbances in superficial (pain, temperature) perception are detected heterolaterally.
When the ventral half is affected (catastrophe in the anterior spinal artery), motor disorders are accompanied by loss of pain, urinary and fecal retention. Tactile and muscle-articular perception are preserved. Dorsal stroke (pathology of the posterior spinal artery) is rare and is manifested by Williamson's syndrome: spastic paresis, sensory ataxia, segmental hypoesthesia, loss of vibration sensitivity of the lower extremities. An isolated lesion of the anterior horn is distinguished by the presence of only unilateral peripheral paresis.