Vestibular disorder
The causes and mechanisms that cause dizziness in neurological diseases are not fully understood. Discussions continue to this day in medical scientific circles, and this despite the fact that in neurology, the most modern diagnostic methods are used to examine the structures of the brain and inner ear. Conventional drug therapy, which includes the use of sedatives, does not always have the desired effect, and in the case of long-term use, it can even have a negative impact on the processes of compensation of the functions of the vestibular system and the patient’s recovery. Vestibular disorders, manifested in vascular pathologies of the head, are the leaders among all vestibular manifestations known to medicine.
Read also
Smell from the mouth
Strong bad breath, also called halitosis, probably causes a feeling of embarrassment in everyone, and if the disease persists for a long time, even anxiety and depression.
It’s no surprise that the shelves… Read more
Adenoids
Probably, in modern times there is not a single parent who has not heard at least once about adenoids. This is the first question that is asked at an appointment with an ENT doctor: “Do we have adenoids?” What are adenoids?...
More details
Tubootitis
What is tubootitis Tubootitis is an inflammation, also called eustachitis, salpingotitis or tubotympanitis, which occurs in the area of the Eustachian tube, causing a decrease in the lumen of the ear canal. How…
More details
Naphthyzine addiction
In our age of availability of medicines, everyone knows about nasal drops, they have used naphthyzine at least once in their life and have heard about naphthyzine addiction. Some are even so afraid of her that they deliberately...
More details
Runny nose
What is a runny nose? A runny nose is an excessive secretion of mucus from the nasal cavity, caused by its inflammation. The manifestations of a runny nose can range from clear fluid to thick mucus. Source...
More details
What diseases cause vestibular disorders?
Vestibular disorders have the following causes:
1. People aged 60 years and older often experience benign positional vertigo, which occurs against the background of traumatic brain injury, otitis media, and ischemia. However, there are cases where the exact reasons were not established.
This vestibular disorder is characterized by the following symptoms and external signs: a person changes his body position in bed (lays down, stands up, turns around), and he experiences a short-term attack of dizziness. In most patients, the exacerbation phase (attacks of dizziness occur quite often) is replaced by a spontaneous long-term remission.
To confirm the diagnosis, special so-called positional tests are used - the person changes the position of the head, and doctors record when nystagmus and dizziness occur.
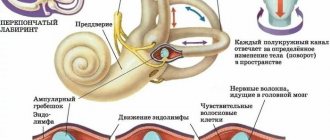
The appearance of this disease is facilitated by the formation of otoliths in the posterior semicircular canal. The force of gravity acts on the otoliths, and they shift, irritating the vestibular receptors of the dome, which leads to dizziness. This condition can last for a very long time without the manifestation of any other disorders.
Treatment of this vestibular disorder with traditional medications often does not produce the desired effect. In cases where the body is particularly resistant to certain medications, surgical intervention is indicated. Severe outbreaks of positional vertigo have another cause - the loop of the anterior inferior cerebellar artery compresses the vestibular nerve, which leads to decreased hearing sensitivity, tinnitus and hyperacusis. Taking carbamazepine (finlepsin) usually helps to relieve the manifestations of this disease, and in cases of ineffectiveness of the drug, a procedure such as microvascular decompression of the nerve is used. Drinking alcohol leads to changes in endolymph density, and this can also cause dizziness.
2. Another fairly well-known cause of dizziness is vestibular neuritis. It is caused by damage to the vestibular nerve or peripheral vestibular apparatus. People of all ages are susceptible to the disease. It is often preceded by infectious diseases affecting the upper respiratory tract. In this case, the following symptoms of the disease and its external signs are distinguished: sudden rotational movements of the head cause an attack of dizziness, vomiting, and a feeling of nausea. The presence of horizontal rotatory nystagmus is observed. An important fact is that in the case of this disease, the nystagmus has only a unilateral direction, while in the case of a bilateral one, we are talking about a different diagnosis. Vestibular neuritis is characterized by the absence of other neurological symptoms (for example, decreased hearing sensitivity). Attacks of severe dizziness, accompanied by repeated vomiting, last in the patient for 3-4 days, but complete remission occurs only after a few weeks. In cases where the patient’s condition does not improve within a month, he is sent to magnetic resonance or computed tomography for additional research. Mild cases of the disease do not require hospitalization; outpatient treatment is quite possible. At the initial stage, short-term treatment with corticosteroids is often prescribed - they reduce vestibular symptoms. The positive effect and improvement in the patient’s condition provide grounds for discontinuing medications and prescribing special exercises to strengthen the vestibular apparatus.
3. The root cause of vestibular disorders in older people with a history of vascular diseases is often vertebrobasilar insufficiency. It can be caused by pathologies such as ischemia of the labyrinth or vestibular nerve or trunk. This vestibular disorder is characterized by the acute development of an attack of dizziness, the presence of disturbances in the functioning of the vestibular system, vomiting, and a feeling of nausea. In some cases of ischemia of adjacent sections of the trunk, other external signs are observed - a person may suddenly fall, he is disoriented, his vision is impaired, his limbs become flaccid and numb.
The occurrence of vertebrobasilar insufficiency can also be caused by some other reasons: atherosclerosis of the arteries, sometimes cardiogenic embolism, increased blood viscosity, vasculitis. To accurately diagnose this disease, it is necessary to take into account the symptoms of various concomitant diseases in the medical history, namely arterial hypertension (high blood pressure), diabetes mellitus, hyperlipidemia. The entire course of treatment for vertebrobasilar insufficiency is primarily aimed at correcting or eliminating risk factors, and includes taking antiplatelet and vasoactive drugs.
4. Blockage of the internal auditory artery is one of the most persistent types of vertigo. The most common external sign of this disease is hearing loss. Cerebellar ataxia and nystagmus, coupled with an acute attack of dizziness, may indicate hemorrhage or cerebellar infarction. And in these cases, emergency intervention is required, since we are talking about human life and death. The initial stage of cerebellar stroke is very similar to vestibular neuritis. And they differ in nystagmus, which in this disorder is bilateral or vertical. The patient is also unable to stand without assistance.
5. Slowly increasing imbalance and moderate dizziness indicate chronic bilateral vestibulopathy. The cause of the disease can be intoxication of the body with certain types of medications. Timely discontinuation of the medication helps restore vestibular function. If this is not done in time, the process becomes irreversible. Various types of solvents, chemicals, and loop diuretins can also sometimes cause a vestibular disorder called chronic vestibulopathy.
6. Here are the known symptoms of Meniere's Disease: dizziness that occurs occasionally, congestion and tinnitus, accompanied by a decrease in hearing sensitivity. An acute attack of dizziness reaches its maximum in a few minutes and regresses in the following hours. At the very beginning of the disease, the process of hearing loss can be stopped. But each subsequent attack leads to the fact that hearing sensitivity becomes lower and lower. In this case, constant tinnitus appears, which intensifies before the onset of an attack and during it. Some patients may fall suddenly without losing consciousness. The reason for this is a sharp increase in pressure in the inner ear and, as a result, irritation of the vestibular receptors. In the process of diagnosing this vestibular disorder, the main condition is the exclusion of other diseases, for example, SLE, neurosyphilis or hypothyroidism.
7. Injuries to the skull and head can often become a source of post-traumatic vertigo. This occurs due to concussion of the labyrinth, the formation of a perilymphatic fistula, or a violation of the integrity of the temporal bone.
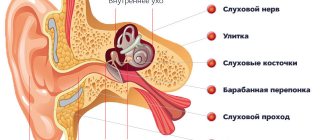
8. There are a number of other ear diseases that can cause vestibular disorders. These include: common wax plugs in the ears, Eustachian tube dysfunction, otosclerosis. Otitis media in acute form can also cause dizziness, especially if it is complicated by purulent processes in the labyrinth.
9. One of the rather rare and infrequent causes of dizziness is a tumor of the cerebellopontine angle. A gradual and slow process of hearing loss, as well as constant tinnitus, indicate a disease such as acoustic neuroma.
10. Let us note another cause of vestibular disorders - basilar migraine. Girls in the prepubertal period are most susceptible to migraine dizziness and pain. They last no more than an hour and are relieved by taking anti-migraine medications.
11. Short-term attacks of dizziness can also occur with epilepsy. But along with them, other symptoms of an epileptic seizure are usually observed: motor, autonomic or sensory, and a disturbance of consciousness is necessarily present.
12. Craniovertebral anomaly - we are talking about it when attacks of dizziness are combined with nystagmus and impaired speech and swallowing functions. Symptoms such as vomiting, nausea, dizziness with rotational movements of the head can signal the initial stage of multiple sclerosis.
Damage to the posterior semicircular tubule
Epley maneuver
The most studied is the Epley maneuver. It is used for pathologies of posterior and lateral SCC:
- The patient sits straight along the couch, with his head turned 45˚ towards the labyrinth that is being examined.
- The patient is placed in a lying position, while the head rotation is maintained, the head is tilted back slightly, hanging over the edge of the couch.
- After 20 seconds, the head turns to the healthy side by 90˚
- After 20 seconds, the head is turned in the same direction by 90˚ along with the patient's body, so that the face is facing down.
- After 20 seconds, the patient returns to a sitting position.
- The Simon maneuver is also used to treat posterior RCC lesions:
- In a sitting position, turn the head 45˚ towards the “healthy” ear, for example the right one
- The patient is quickly placed on his left side (head face up), an attack of dizziness occurs with rotatory nystagmus to the left, the position is maintained for 3 minutes. During this time, the otoliths descend to the lowest part of the RCC.
- Quickly turn the patient onto his right side (head face down). Maintain the position for 3 minutes.
- The patient is slowly returned to the starting position.
The fixed otolith resolves within a few weeks. The same amount of time is required for attacks of dizziness to disappear during the natural course of the disease.
According to research by Casani A.R. et al. (2011) the average duration of dizziness with damage to the posterior ACC was 39 days, with damage to the lateral ACC - 16 days.
Manipulations are often accompanied by a sharp temporary increase in the symptoms of the disease: dizziness, nausea, vegetative symptoms.
After the maneuver, the patient must be monitored after 3 days and 1 month, which will allow the maneuver to be repeated if it is ineffective or to promptly begin a search for other causes of dizziness if new symptoms appear.
Relapses occur relatively rarely (3.8 - 29% of cases).
Brandt-Daroff gymnastics
If the maneuvers performed by the doctor are ineffective, patients with damage to the posterior RCC are recommended to perform Brandt-Daroff gymnastics on their own:
- In the morning, after sleep, sit on the bed with your back straight (Position 1)
- Then you need to lie on your left (right) side with your head turned up at 45° (to maintain the correct angle, it is convenient to imagine a person standing next to you at a distance of 1.5 meters and keep your gaze on his face) (Position 2)
- Hold this position for 30 seconds or until the dizziness disappears
- Return to the starting position sitting on the bed
- Then you need to lie on the other side with your head turned up 45° (Position 2)
- Stay in this position for 30 seconds
- Return to the starting position sitting on the bed (Position 1)
Repeat the described exercise 5 times.
If dizziness does not occur during the exercise, it is advisable to perform it only the next morning. If dizziness occurs at least once in any position, then you need to perform the exercises at least two more times: in the afternoon and in the evening.
Which doctors should I contact if a vestibular disorder occurs?
If you notice disturbances in your vestibular state, you should definitely seek advice from a specialist - a neurologist. Based on certain symptoms and external signs, only a doctor can make an accurate diagnosis. Therefore, if you find signs of a neurological disease, seek help from a neurologist. Do not put your health at risk - do not self-medicate.
Primary appointment with a neurologist: 1850 RUR.
Sign up Online 5% discount when registering from the site
Diagnostics
There are diagnostic criteria for the disease. They are a combination of symptoms. Attacks of rotational vertigo, provoked by the position of the head and a significant change in the duration of the attack (both up and down) when changing the position of the body or head in space. Presence of hearing loss. The presence of persistent vestibular disorders outside of an attack according to objective research methods. Reduced frequency of manifestations when using anticonvulsants.
Differential diagnosis is made with BPPV, psychogenic variant of dizziness, vestibular epilepsy, perilymphatic fistula. The diagnosis of vestibular paroxysmia is a diagnosis of exclusion.
Performing tests to detect BPPV can also provoke an attack, however, unlike it, there will be no rotatory nystagmus.
It is also possible to determine spontaneous nystagmus, sometimes simply by turning off gaze fixation, which can transform in direction after a hyperventilation test.
An instrumental examination will include contrast MRI (detection of vascular conflict), as well as the following research methods:
- EEG. To exclude epilepsy.
- Nystagmography.
- Evoked potentials.
- Audiometric examination