- General characteristics Definition of hypoxia
- Development of hypoxia
- Exogenous hypoxia
Hypoxia is a pathological condition in which oxygen deficiency occurs in the body due to its reduced supply from the outside and/or due to dysfunctional utilization in cells.
hypoxia
“Hypoxia” – hypo and oxigenium (lack of oxygen), translation from ancient Greek. Most people understand hypoxia as oxygen starvation (lack of oxygen) , because... in this case, tissues and organs experience dysfunction from oxygen deficiency.
General characteristics of hypoxia
Definition of hypoxia
Hypoxia is a typical and dangerous pathological process that occurs in the body during a wide range of diseases and acute conditions, and provokes them. For example, hypoxia can be caused by various factors, and also accompany a wide range of diseases, and may even be the main link in the appearance of pathological changes or diseases.
Based on this:
hypoxia is a typical general pathological process and does not relate to either a diagnosis or a syndrome.
The effect of hypoxia at the cellular level is divided into two types - adaptive reactions and decompensation .
During the occurrence of hypoxia, the body launches adaptive protective reactions that maintain for a short time the almost normal functioning of organs and tissues. With prolonged exposure to hypoxia, the body's reserves run out and adaptive defense reactions are switched off - decompensation occurs.
Decompensation is characterized by the occurrence of irreversible disorders in organs and tissues - from organ failure to death.
Development of hypoxia
Compensatory reactions during hypoxia are expressed by oxygen deficiency at the cellular level, and their task is to restore the amount of oxygen in tissues. The complex of compensatory reactions to eliminate the influence of hypoxia includes the organs of the cardiovascular and respiratory systems, and changes in biochemical processes in tissues and organ structures that suffer most from oxygen deficiency are triggered. Until the supply of compensatory reactions is completely exhausted, organs and tissues will not suffer from a lack of oxygen. However, if, when compensatory mechanisms are depleted, the supply of oxygen is not normalized, then irreversible decompensation will begin in the tissues with damage to cells and dysfunction of the entire organ.
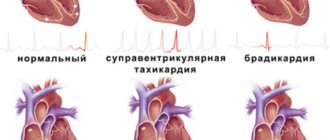
In acute and chronic hypoxia, the nature of compensatory reactions is different. Thus, during acute hypoxia, compensatory reactions consist of increased breathing and blood circulation, that is, blood pressure rises, tachycardia occurs (heart rate more than 70 beats per minute), breathing becomes deep and frequent, the heart pumps a larger volume of blood per minute than normal . In addition, in response to acute hypoxia, all “reserves” of red blood cells, which are necessary to carry oxygen to the cells, are released into the systemic circulation from the bone marrow and spleen.
hypoxia
All these reactions are aimed at normalizing the amount of oxygen delivered to the cells by increasing the volume of blood passing through the vessels per unit of time and increasing the amount of oxygen transferred. With very severe acute hypoxia, in addition to the development of these reactions, centralization of blood circulation also occurs, which consists of redirecting all available blood to vital organs (heart and brain) and a sharp decrease in blood supply to the muscles and organs of the abdominal cavity. The body directs all the oxygen to the brain and heart - organs critical for survival, and, as it were, “deprives” those structures that are currently not needed for survival (liver, stomach, muscles, etc.).
If acute hypoxia is eliminated without depleting the body's reserves, then the person will survive, and all his organs and systems will function completely normally after some time. If hypoxia continues longer than the period of effectiveness of compensatory reactions, then irreversible changes will occur in organs and tissues.
Compensatory reactions during chronic hypoxia develop against the background of severe long-term diseases or conditions. First, to compensate for oxygen deficiency, the number of red blood cells in the blood increases, which allows the volume of oxygen carried by the same volume of blood per unit time to increase. Also, in red blood cells, the activity of an enzyme increases, facilitating the transfer of oxygen from hemoglobin directly to the cells of organs and tissues. New alveoli are formed in the lungs, breathing deepens, the volume of the chest increases, additional vessels are formed in the lung tissue, which improves the supply of oxygen to the blood from the surrounding atmosphere. The heart, which has to pump more blood per minute, hypertrophies and increases in size. Changes also occur in tissues - the number of mitochondria (organelles that use oxygen to ensure cellular respiration) increases in cells, and many new capillaries are formed in tissues. It is precisely because of the activation of microcirculation and a large number of capillaries during hypoxia that a person develops a pinkish coloration of the skin, which is mistaken for a “healthy” blush.
Adaptive reactions during acute hypoxia are reflexive, and therefore, when oxygen starvation is eliminated, they cease their effect, and the organs completely return to the mode of functioning in which they existed before the development of the episode of hypoxia. In chronic hypoxia, adaptive reactions are not reflexive; they develop due to the restructuring of the functioning mode of organs and systems, and therefore their action cannot be quickly stopped after oxygen starvation is eliminated.
With chronic hypoxia, the body can change its functioning mode in such a way that it completely adapts to conditions of oxygen deficiency and does not suffer from it at all. For example, this is how the body of residents of megacities adapts.
In acute hypoxia, complete adaptation to oxygen deficiency cannot occur, since the body simply does not have time to rearrange its functioning modes, and all its compensatory reactions are designed only to temporarily maintain the functioning of organs until adequate oxygen delivery is restored.
That is why a person can have a state of chronic hypoxia for many years without interfering with his normal life and work, while acute hypoxia in a short period of time can lead to death or irreversible damage to the brain or heart.
Compensatory reactions during hypoxia always lead to changes in the functioning of the most important organs and systems. These manifestations of compensatory reactions can be conditionally considered symptoms of hypoxia.
Types of hypoxia
Hypoxia, depending on the mechanism of development, is divided into:
- Exogenous hypoxia (hypoxic hypoxia) is caused by environmental factors.
- Endogenous hypoxia is caused by various diseases or disorders that a person has:
- Respiratory (respiratory, pulmonary) hypoxia.
- Circulatory (cardiovascular) hypoxia: Ischemic; Stagnant.
- Hemic (blood) hypoxia: Anemic; Caused by inactivation of hemoglobin.
- Tissue (histotoxic) hypoxia. Substrate hypoxia.
- Overload hypoxia. Mixed hypoxia.
Depending on the speed of development and course:
- Lightning fast (instant) – develops within a few seconds (no longer than 2 – 3 minutes);
- Acute – develops within several tens of minutes or hours (no longer than 2 hours);
- Subacute – develops within several hours (no longer than 3-5 hours);
- Chronic – develops and lasts for weeks, months or years.
Depending on the prevalence of oxygen starvation , hypoxia is divided into general and local .
Exogenous hypoxia
Exogenous hypoxia (hypoxic) is caused by a decrease in the amount of oxygen in the inhaled air. Accordingly, blood leaves the lungs that is not sufficiently saturated with oxygen and a small amount of gas is brought to the cells of various organs/tissues. Exogenous hypoxia is manifested by cyanosis (blueness of the skin and mucous membranes), dizziness and fainting.
exogenous hypoxia normobaric
Depending on atmospheric pressure, exogenous hypoxia is divided into hypobaric and normobaric.
Hypobaric hypoxia is caused by low oxygen content in rarefied air with low atmospheric pressure. Such hypoxia develops in mountainous areas and at high altitudes.
Normobaric hypoxia develops when there is a low oxygen content in air with normal atmospheric pressure. Normobaric exogenous hypoxia can develop when being in mines, wells, on submarines, in diving suits, in cramped rooms with large crowds of people, with general air pollution or smog in cities, as well as during surgery if anesthesia-respiratory equipment malfunctions.
Respiratory (respiratory, pulmonary) hypoxia
respiratory hypoxia
Respiratory (respiratory, pulmonary) hypoxia develops in diseases of the respiratory system (bronchitis, pulmonary hypertension, any lung pathologies, etc.), when the penetration of oxygen from the air into the blood is difficult. Against the background of respiratory hypoxia, complications may develop, such as respiratory failure, cerebral edema and gas acidosis.
Circulatory (cardiovascular) hypoxia
circulatory hypoxia
Circulatory (cardiovascular) hypoxia develops against the background of various circulatory disorders (for example, decreased vascular tone, decreased total blood volume after blood loss or dehydration, increased blood viscosity, increased coagulability, centralization of blood circulation, venous stagnation, etc.). If a circulatory disorder affects the entire network of blood vessels, then systemic . If blood circulation is disrupted only in the area of an organ or tissue, then hypoxia is local .
During circulatory hypoxia, a normal amount of oxygen enters the blood through the lungs, but due to circulatory disorders, it is delivered to organs and tissues with a delay, as a result of which oxygen starvation occurs in the latter.
According to the mechanism of development, circulatory hypoxia is ischemic and stagnant. The ischemic form of hypoxia develops with a decrease in the volume of blood passing through organs or tissues per unit of time. This form of hypoxia can occur with left ventricular heart failure, heart attack, cardiosclerosis, shock, collapse, vasoconstriction of some organs and other situations.
The stagnant form of hypoxia develops when the speed of blood movement through the veins decreases - with thrombophlebitis of the legs, right ventricular heart failure, increased intrathoracic pressure and other situations when blood stagnation occurs in the venous bed. In the stagnant form of hypoxia, venous blood does not return to the lungs in time to remove carbon dioxide and saturate with oxygen. As a result, there is a delay in the delivery of the next portion of oxygen to organs and tissues.
Hemic (blood) hypoxia
Hemic (blood) hypoxia develops when quality characteristics are impaired or the amount of hemoglobin in the blood decreases. Hemic hypoxia is divided into two forms - anemic and caused by changes in hemoglobin quality .
hemic hypoxia
Anemic hemic hypoxia is caused by a decrease in the amount of hemoglobin in the blood, that is, anemia of any origin or hydremia (dilution of the blood due to fluid retention in the body). During anemic hypoxia, oxygen is normally bound and transported by the blood to organs and tissues. But due to the fact that there is too little hemoglobin, insufficient oxygen is brought to the tissues and hypoxia occurs in them.
Hypoxia, caused by a change in the quality of hemoglobin, is associated with poisoning by various toxic substances, which lead to the formation of forms of hemoglobin that are not capable of carrying oxygen (methemoglobin or carboxyhemoglobin). When the quality of hemoglobin changes, its quantity remains normal, but it loses its ability to carry oxygen. As a result, when passing through the lungs, hemoglobin is not saturated with oxygen and the blood flow does not deliver it to the cells of all organs and tissues. A change in the quality of hemoglobin occurs when poisoned by a number of chemicals, such as carbon monoxide (carbon monoxide), sulfur, nitrites, nitrates, etc.
Tissue (histotoxic) hypoxia
Tissue (histotoxic) hypoxia develops against the background of impaired ability of organ cells to absorb oxygen. The cause of tissue hypoxia is reduced activity or deficiency of mitochondrial respiratory chain enzymes, which convert oxygen into forms in which it is used by cells to carry out all life processes.
Disruption of respiratory chain enzymes can occur in the following cases:
- Suppression of the activity of respiratory chain enzymes in case of poisoning with cyanide, ether, urethane, barbiturates and alcohol;
- Lack of enzymes of the respiratory chain due to deficiency of vitamins B1, B2, PP and B5;
- Disruption of the enzymes of the respiratory chain due to poisoning with nitrates, microbial toxins, exposure to large amounts of thyroid hormones, etc.;
- Damage to the structure of enzymes due to exposure to radioactive radiation, uremia, cachexia, severe infectious diseases, etc.
Tissue hypoxia can exist for a long period of time.
Substrate hypoxia
substrate hypoxia
Substrate hypoxia develops with normal oxygen delivery to tissues, but in conditions of a lack of basic nutrients that undergo oxygen oxidation. Substrate hypoxia can develop during fasting, diabetes and other conditions when there is not enough glucose and fatty acids in the cells.
Overload hypoxia
overload hypoxia
Overload hypoxia can develop during heavy physical work, when cells intensively consume oxygen. In such cases, the cells simply do not have enough oxygen delivered. Such physiological hypoxia is not dangerous and goes away after completing the stage of high physical activity.
Mixed hypoxia
Mixed hypoxia is a combination of several types of endogenous hypoxia and occurs with severe, life-threatening lesions of various organs and systems, such as shock, poisoning, coma, etc.
Acute hypoxia
Acute hypoxia develops quickly, within several tens of minutes, and persists for a limited period of time, ending either with the elimination of oxygen starvation, or with irreversible changes in organs that will lead to severe illness or even death. Acute hypoxia usually accompanies acute conditions in which blood flow, quantity and quality of hemoglobin sharply change, such as, for example, blood loss, cyanide poisoning, heart attack, etc.
acute hypoxia
Any variant of acute hypoxia must be eliminated as soon as possible, since the body will be able to maintain the normal functioning of organs and tissues for a limited period of time until compensatory and adaptive reactions are exhausted. And when the compensatory-adaptive reactions are completely exhausted, the most important organs and tissues (primarily the brain and heart) will begin to die under the influence of hypoxia.
In principle, acute hypoxia is more dangerous than chronic hypoxia, since it can quickly lead to disability, organ failure or death. And chronic hypoxia can exist for years, giving the body the opportunity to adapt and live and function quite normally.
Chronic hypoxia
chronic hypoxia
Chronic hypoxia develops over several days, weeks, months or even years, and occurs with long-term diseases. The body adapts to chronic hypoxia by changing the structure of cells to new conditions, which allows organs to function quite normally. In principle, chronic hypoxia is safer than acute hypoxia, because develops slowly and the body is able to adapt to new conditions using compensation mechanisms.
Story 1: Tregs vs. Th17 lymphocytes
Naive CD4+ T cells, depending on the microenvironment, are able to differentiate into various subpopulations with very different functions: Th1, Th2, Tfh, Th17 and iTreg. In matters of autoimmune diseases and antitumor immunity, great attention has been paid to two recently discovered populations of T lymphocytes: Th17 and iTreg [17].
Th17 cells differentiate from naive CD4+ lymphocytes under the influence of TGF-β and IL-6; activation of the transcription factors STAT3 and RORgt is critical. Th17 lymphocytes have powerful bactericidal and fungicidal effects due to the secretion of IL-17 and IL-22. However, due to their excessive inflammatory potential, Th17 are notorious contributors to many autoimmune diseases.
Induced iTregs differentiate from naïve CD4+ lymphocytes under the influence of TGF-β and IL-2; activation of the transcription factor Foxp3 is critical. Tregs produce IL-10, TGFβ, and express many interesting molecules on their surface (such as the IL-2 receptor CD25, the inhibitory coreceptor CTLA-4), due to which they exhibit their immunosuppressive properties.
In total, we have two subpopulations of lymphocytes that have diametrically opposed properties, are not capable of reprogramming into each other and originate from a single precursor - naive CD4+ lymphocytes. There is often talk about the balance between Tregs and Th17, a shift in the balance either to the immunosuppressive or proinflammatory side in various diseases, and emphasize the paramount importance of the mechanisms that determine differentiation along one of the two pathways. Let's briefly look at the mechanisms and try to understand what the point is.
The first thing the attentive reader will notice is the TGFβ inducer common to the two subpopulations. It is known that high concentrations of TGFβ themselves are capable of supporting the activation of Foxp3 and committing the formation of iTregs. However, Th17 is also characterized by activation of Foxp3, which must be suppressed. It is suppressed due to the activation of the STAT3 factor (under the influence of IL-6, IL-21 or IL-23), which, in turn, activates RORgt, which actively suppresses the activity of Foxp3 and determines the expression of Th17-specific chemokines.
Now about the role of HIF-1. In non-myeloid cells, it has been shown that activation of STAT3 can lead to non-hypoxic activation of HIF-1. HIF-1, in turn, is able to inhibit Foxp3, probably through the mechanism of activation of polyubiquitination followed by proteasomal degradation, i.e. the mechanism by which HIF-1 is destroyed itself. By inhibiting Foxp3, HIF-1 promotes the differentiation of CD4+ naive lymphocytes in the Th17 direction. Interestingly, this STAT3-dependent non-hypoxic activation of HIF-1 followed by Foxp3 inhibition can be replaced by cycles of intermittent hypoxia-normoxia, which leads to stabilization and accumulation of HIF-1 (Fig. 8).
Figure 8. Role of HIF-1 in the differentiation of CD4+ naive lymphocytes into Tregs and Th17.
Interestingly, the same does not happen under conditions of prolonged hypoxia. And the culprit here is negative feedback - prolonged hypoxia increases the expression of HIF-dependent microRNA-210, which can suppress the translation of HIF-1α.
The above concept of a special role for HIF-1 in activating RORgt (critical for Th17) and inhibiting Foxp3 (critical for Tregs) is supported by a recent remarkable paper on the role of Deltex1 in maintaining Foxp3 stability by inhibiting its negative regulator HIF-1 [18].
Not long ago, a new subpopulation of lymphocytes was discovered - Tr1, which has immunosuppressive properties, but does not express Foxp3 (a marker of regulatory T lymphocytes). Tr1 play a special role in the suppression of inflammation in the nervous system and intestine [19].
Interestingly, hypoxia and increased concentrations of extracellular ATP—frequent attributes of inflammation—can inhibit the differentiation of Tr1 lymphocytes. The mechanism turned out to be very beautiful: the critical factor for differentiation into Tr1 lymphocytes is the AHR factor, which, when interacting with its nuclear transporter ARNT, is transferred to the nucleus and activates the expression of IL-10, IL-21 and other factors that determine the immunosuppressive properties of Tr1 lymphocytes. However, ARNT is well known to us as HIF-1β, the oxygen independent subunit with which HIF-1α dimerizes. Under these conditions, competition for ARNT occurs between HIF-1α and AHR, and HIF-1α wins this competition. However, if conditions allow, and ARNT wins the battle, it has something to answer - when activated, it promotes the degradation of HIF-1α, presumably by increasing the expression of PHDs prolyl hydroxylases via an oxygen-dependent mechanism (Fig. 9).
Figure 9. Role of HIF-1 in the differentiation of immunosuppressive Tr1 lymphocytes.
I would also like to note that the inhibitory role of HIF-1α on the differentiation of Tr1 lymphocytes was not so clear - researchers note that the activity of HIF-1α is important in the early stages of differentiation, mainly due to its ability to switch metabolism to the glycolytic type.
Myocardial hypoxia
myocardial hypoxia
Myocardial hypoxia is one of the most dangerous diseases and is characterized by insufficient oxygen supply to the heart muscle.
This condition occurs when there is a sudden decrease in oxygen supply to the heart muscle. Cells do not have time to adapt to changed conditions. Metabolism continues in them, but it becomes incomplete, and under-oxidized metabolites accumulate. If hypoxia persists, cardiac muscle tissue dies.
Clinically, this condition is manifested by attacks of chest pain, increasing their duration and intensity. Subsequently, myocardial infarction develops - necrosis of the heart muscle with loss of its contractile function.
Myocardial hypoxia can be caused by the following reasons:
- low oxygen content in atmospheric air;
- diseases of the lungs with impaired gas exchange in them;
- decrease in the amount of blood flowing through the myocardium due to pathology of the coronary arteries;
- deterioration of the blood's ability to carry oxygen, for example, with carbon monoxide poisoning;
- disruption of oxygen utilization by the cells themselves, for example, in case of poisoning with cyanides and heavy metals.
Drugs for treatment
Another way to saturate the brain with oxygen?
To restore vascular circulation to the brain, medications are used that can relieve severe symptoms of the pathology, improve metabolism in brain cells, and restore mental abilities along with lost coordination of movements. There are several groups of drugs that saturate the brain with oxygen with different mechanisms of action that help normalize cerebral circulation:
- vasodilators (their effect is based on the ability to relax vascular walls);
- anticoagulants that prevent platelets from sticking together;
- nootropics that prevent irreversible changes in nervous tissue.
Everyone should know how to saturate the brain with oxygen at home.
Consequences of hypoxia
The consequences of hypoxia can be different and depend on the period of time during which oxygen starvation was eliminated and how long it lasted. If hypoxia was eliminated during a period when the compensatory mechanisms were not exhausted, then there will be no negative consequences; after some time, the organs and tissues will completely return to their normal mode of operation. But if hypoxia was eliminated during the period of decompensation, when compensatory mechanisms were exhausted, then the consequences depend on the duration of oxygen starvation. The longer the period of hypoxia against the background of decompensation of adaptive mechanisms, the stronger and deeper the damage to various organs and systems. Moreover, the longer hypoxia lasts, the more organs are damaged.
During hypoxia, the brain suffers the most, since it can withstand without oxygen for 3-4 minutes, and from the 5th minute necrosis will begin to form in the tissues. The heart muscle, kidneys and liver are able to tolerate a period of complete absence of oxygen for 30-40 minutes.
The consequences of hypoxia are always due to the fact that in cells, in the absence of oxygen, the process of oxygen-free oxidation of fats and glucose begins, which leads to the formation of lactic acid and other toxic metabolic products that accumulate and ultimately damage the cell membrane, leading to its death. When hypoxia lasts long enough from the toxic products of improper metabolism, a large number of cells in various organs die, forming entire areas of dead tissue. Such areas sharply worsen the functioning of the organ, which is manifested by corresponding symptoms, and in the future, even with the restoration of oxygen flow, will lead to a persistent deterioration in the functioning of the affected tissues.
The main consequences of hypoxia are always caused by disruption of the central nervous system, since it is the brain that suffers primarily from oxygen deficiency. Therefore, the consequences of hypoxia are often expressed in the development of a neuropsychiatric syndrome, including parkinsonism, psychosis and dementia. In 50-70% of cases, neuropsychiatric syndrome can be cured. In addition, a consequence of hypoxia is exercise intolerance, when with minimal exertion a person experiences palpitations, shortness of breath, weakness, headache, dizziness and pain in the heart area. Also, the consequences of hypoxia can be hemorrhages in various organs and fatty degeneration of muscle, myocardial and liver cells, which will lead to disruptions in their functioning with clinical symptoms of failure of one or another organ, which can no longer be eliminated in the future.
Features of the course of brain hypoxia and adaptive reactions of the body
The severity of hypoxia in different organs and tissues may vary. So, if a threatening situation arises, the body will independently redistribute blood in such a way that the brain is supplied with it better than other organs and tissues. This process is called centralization of blood circulation. It can turn on, for example, during acute blood loss.
The result of this mechanism is that the brain suffers less from hypoxia than peripheral organs, such as the liver or kidneys, where irreversible changes do not develop at such a high rate.
Hypoxia - causes
The causes of exogenous hypoxia may be the following factors:
- Thin atmosphere at altitude (mountain sickness, altitude sickness, pilot sickness);
- Being in tight spaces with large crowds of people;
- Being in mines, wells or in any enclosed spaces (for example, submarines, etc.) with no communication with the outside environment;
- Poor ventilation of premises;
- Working in diving suits or breathing through a gas mask;
- Severe air pollution or smog in the city of residence;
- Malfunction of anesthesia-respiratory equipment.
The causes of various types of endogenous hypoxia may be the following factors:
- Respiratory diseases (pneumonia, pneumothorax, hydrothorax, hemothorax, destruction of alveolar surfactant, pulmonary edema, pulmonary embolism, tracheitis, bronchitis, emphysema, sarcoidosis, asbestosis, bronchospasm, etc.);
- Foreign bodies in the bronchi (for example, accidental swallowing of various objects by children, choking, etc.);
- Asphyxia of any origin (for example, due to compression of the neck, etc.);
- Congenital and acquired heart defects (non-closure of the foramen ovale or the duct of Batal, rheumatism, etc.);
- Damage to the respiratory center of the central nervous system due to injuries, tumors and other diseases of the brain, as well as when it is suppressed by toxic substances;
- Impaired breathing mechanics due to fractures and displacements of the chest bones, damage to the diaphragm or muscle spasms;
- Cardiac dysfunction caused by various heart diseases and pathologies (heart attack, cardiosclerosis, heart failure, electrolyte imbalance, cardiac tamponade, pericardial obliteration, blockade of electrical impulses in the heart, etc.);
- A sharp narrowing of blood vessels in various organs;
- Arteriovenous shunting (transfer of arterial blood into veins through vascular shunts before it reaches organs and tissues and releases oxygen to cells);
- Stagnation of blood in the inferior or superior vena cava system;
- Thrombosis;
- Poisoning with chemicals that cause the formation of inactive hemoglobin (for example, cyanide, carbon monoxide, lewisite, etc.);
- Anemia;
- Acute blood loss;
- Disseminated intravascular coagulation syndrome (DIC syndrome);
- Impaired metabolism of carbohydrates and fats (for example, diabetes, obesity, etc.);
- Shock and coma;
- Excessive physical activity;
- Malignant tumors of any location;
- Chronic kidney and blood diseases (for example, leukemia, anemia, etc.);
- Deficiency of vitamins PP, B1, B2 and B5;
- Thyroid diseases;
- Damage to cells by radiation, tissue breakdown products due to cachexia, severe infections or uremia;
- Drug and alcohol abuse;
- Prolonged fasting.
Treatment with medications
Hypoxia is treated using medications from various groups:
- Analgesics. You can use any medications, but only after consulting a doctor. Usually pain is relieved with Akamol, Pentalgin, Bupranal or Anopyrine.
- Antidotes. Designed to get rid of hypoxia that occurs after poisoning. When intoxicating the body, medicinal drugs are used: “Flumazenil”, mushrooms – “Diazepam” or “Atropine”, heavy metals – “Cuprenil” or “Unithiol”, organic acids – “Almagel”, carbon monoxide – glucose.
- Dilatating bronchi. Most often it is recommended to use Truvent, Berodual, Atrovent and Salbumatol.
- Antispasmodics. The drugs are used if a stroke condition occurs as a result of the disease.
- Vitamins. In case of poisoning, the patient is prescribed K1, C and B6. The multivitamin complex is recommended for patients with any form of the disease.
Symptoms (signs) of hypoxia
symptoms of hypoxia
In the fulminant form of hypoxia, clinical symptoms do not have time to appear, since death occurs within a very short period of time (up to 2 minutes).
The acute form of hypoxia lasts up to 2-3 hours, and during this period there is a failure of all organs and systems at once, primarily the central nervous system, respiration and heart (heart rate becomes less frequent, blood pressure drops, breathing becomes irregular, etc.). If hypoxia is not eliminated during this period, then organ failure progresses to coma and agony, followed by death.
Subacute and chronic forms of hypoxia are manifested by the so-called hypoxic syndrome. Against the background of hypoxic syndrome, symptoms from the central nervous system first appear, since the brain is most sensitive to oxygen deficiency, as a result of which foci of necrosis (dead areas), hemorrhages and other types of cell destruction quickly appear in its tissues. Due to necrosis, hemorrhage and death of brain cells against the background of oxygen deficiency at the initial stage of hypoxia, a person develops euphoria, he is in an excited state, and he is tormented by motor restlessness. One's own condition is not assessed critically.
With further progression of hypoxia, the following signs of depression of the cerebral cortex appear, which are similar in manifestations to alcohol intoxication:
- Drowsiness;
- Lethargy;
- Headache and dizziness;
- Noise in ears;
- Lethargy;
- Impaired consciousness;
- Involuntary passage of urine and feces;
- Nausea and vomiting;
- Movement coordination disorder;
- Cramps.
Convulsions during hypoxia appear when exposed to external stimuli. Moreover, a convulsive attack usually begins with twitching of the muscles of the face, hands and feet with the addition of random muscle contractions of the abdomen. Sometimes during convulsions opisthotonus , which represents a person arched with straightened neck and back muscles, head thrown back and arms bent at the elbows. The posture of a person in opisthotonus resembles the gymnastic figure “bridge”.
In addition to symptoms of depression of the cerebral cortex, a person also experiences pain in the heart area, irregular breathing, shortness of breath, a sharp decrease in vascular tone, tachycardia (an increase in heart rate of more than 70 beats per minute), a drop in blood pressure, cyanosis (blueness of the skin), decrease in body temperature. But when poisoned with substances that inactivate hemoglobin (for example, cyanides, nitrites, nitrates, carbon monoxide, etc.), human skin becomes pinkish in color.
With prolonged hypoxia with the slow development of damage to the central nervous system, a person may develop mental disorders in the form of delirium (“delirium tremens”), Korsakov’s syndrome (loss of orientation, amnesia, replacement of real events by fictitious events, etc.) and dementia.
With further progression of hypoxia, blood pressure drops to 20-40 mmHg. Art. and a coma occurs with loss of brain function. If blood pressure drops below 20 mmHg. Art., then death occurs. In the period before death, a person may experience agonizing breathing in the form of rare convulsive attempts to breathe.
General symptoms
The disease can be identified by signs such as:
- severe pain in the head;
- problems with memory and attention;
- the occurrence of ringing and buzzing in the ears;
- loss of concentration;
- fast fatiguability;
- nausea in the morning.
The longer a person is sick, the more manifestations of the disease appear at each stage:
- Excessive excitability. During diagnosis, a specialist may see that the structure of the brain tissue is slightly changed. This leads to the fact that the patient, who is in a state of euphoria, cannot control his behavior.
- Changes in appearance. A person has very pale skin, on which red spots or swelling appear that look blue. The human brain at this stage is busy restoring blood circulation. This leads to the patient's body becoming covered in cold sweat and perspiration appearing on the forehead.
- Disruption of the nervous system. The central nervous system of a sick person begins to slow down, as brain tissue is severely damaged. As a result, the person feels nauseous and constantly vomits. He also begins to feel dizzy, his vision becomes dark, and his visual function is impaired. In the future, the patient may lose consciousness.
- Damage to the central nervous system (perinatal). Edema develops in the brain tissue. As a result, the person loses all reflexes.
Degrees of hypoxia
Depending on the severity and severity of oxygen deficiency, the following degrees of hypoxia are distinguished:
- Mild (usually detected only during physical activity);
- Moderate (phenomena of hypoxic syndrome appear at rest);
- Severe (the symptoms of hypoxic syndrome are strongly expressed and there is a tendency to transition to a coma);
- Critical (hypoxic syndrome has led to coma or shock, which can result in agony and death).
Treatment of oxygen starvation
In practice, mixed forms of hypoxia usually develop , as a result of which the treatment of oxygen deficiency in all cases should be comprehensive, aimed simultaneously at eliminating the causative factor and maintaining an adequate supply of oxygen to the cells of various organs and tissues.
To maintain a normal level of oxygen supply to cells in any type of hypoxia, hyperbaric oxygenation (HBO) - barotherapy - is used. In barotherapy, pressure chambers are used in which a person is under increased pressure with a high oxygen content. Due to the increased pressure, oxygen is additionally dissolved directly in the blood plasma, without contacting red blood cells, which allows its delivery to organs and tissues in the required quantity, regardless of the activity and functional usefulness of hemoglobin. Thanks to hyperbaric oxygenation, it is possible not only to supply organs with oxygen, but also to dilate the blood vessels of the brain and heart, so that the latter can work at full capacity.
In addition to hyperbaric oxygenation, cardiac drugs and drugs that increase blood pressure are used for circulatory hypoxia. If necessary, a blood transfusion is performed (if blood loss incompatible with life has occurred).
For hemic hypoxia, in addition to hyperbaric oxygenation, the following therapeutic measures are carried out:
- Blood or red blood cell transfusion;
- Introduction of oxygen carriers (Perftoran, etc.);
- Hemosorption and plasmapheresis to remove toxic metabolic products from the blood;
- Introduction of substances capable of performing the functions of enzymes of the respiratory chain (vitamin C, methylene blue, etc.);
- Introduction of glucose as the main substance that provides cells with energy to carry out vital processes;
- Administration of steroid hormones to eliminate severe oxygen starvation of tissues.
Treatment of cerebral hypoxia
Since brain hypoxia is most often associated with a number of factors, complex therapy is necessary, which depends on the cause that led to this pathological condition.
If hypoxia is the result of a lack of oxygen in the inhaled air, then the person should be switched to breathing normal air as quickly as possible. Provided that the brain cells have not been destroyed, recovery will not take much time, and all functional disorders will be eliminated. Sometimes patients are advised to add 3-7% carbon dioxide to regular oxygen. This will expand the blood vessels of the brain and stimulate the functioning of the respiratory center.
If there is a foreign object or other obstruction in the airway, tracheal intubation and tracheotomy may be required. The patient is placed in a position that facilitates breathing.
In case of severe respiratory failure, or complete absence of breathing, auxiliary or artificial respiration and artificial ventilation of the lungs are necessary. Oxygen therapy should be continuous and long-lasting until it is no longer needed.
Blood transfusions, cardiac and hypertensive medications are required for circulatory hypoxia. In this case, it is important to normalize blood circulation. If the patient has suffered cardiac arrest, chest compressions and the use of a defibrillator are required. The doctor may administer adrenaline, atropine, and take other resuscitation measures. All these measures must be carried out as quickly as possible, so it is possible that they can be carried out while still in the ambulance.
To treat and prevent cerebral hypoxia, medications with an antihypoxic effect can be used. These are narcotic and neuroleptic drugs, drugs to reduce body temperature, etc. Sometimes glucocorticoids can help.
It is imperative to restore the acid-base and electrolyte balance in the body, but this already applies to symptomatic treatment. Seduxen, which is administered intravenously, allows you to relieve convulsions. If this does not help, then the introduction of muscle relaxants is indicated.
To eliminate the consequences of brain hypoxia, it is possible to use drugs such as:
- Dibazol.
- Galantamine.
- Sodium hydroxybutyrate.
- Nerobol.
- Pyridoxine.
- Cerebrolysin.
- ATP.
- Tranquilizers.
- Vitamin and mineral complexes.
The patient will definitely have to visit the massage therapist’s office and perform therapeutic gymnastic complexes.
First aid for a person with cerebral hypoxia
The only thing a person who does not have a medical education can do for a victim with cerebral hypoxia is to provide him with a flow of fresh air and call an ambulance as quickly as possible. Until doctors arrive, you should ventilate the room and remove from the victim all items of clothing that may interfere with breathing.
Prevention of hypoxia
Effective prevention of hypoxia is to avoid conditions in which the body may experience oxygen starvation. To do this, you need to lead an active lifestyle, be in the fresh air every day, exercise, eat well, and promptly treat existing chronic diseases. When working in an office, you need to periodically ventilate the room (at least 2-3 times during the working day) to saturate the air with oxygen and remove carbon dioxide from it.
prevention of hypoxia in a pressure chamber
It is also recommended to undergo a course of barotherapy (oxygen capsules and pressure chambers) several times a year, which helps reduce cases of oxygen starvation in the body.