Treatment of apraxia in Saratov, Russia, therapy of apraxia
Sarklinik provides treatment for certain types of apraxia in adults, adolescents, children, boys, girls, boys, girls, men, women in Saratov, Russia. The doctor knows how to treat apraxia , how to cure apraxia, how to get rid of apraxia, what to do with apraxia, where to go. At the first consultation, will the doctor tell you what types of apraxia there are? What are the characteristics of kinesthetic (kinetic) apraxia, aphasia and agnosia ? Why does oral apraxia, motor apraxia, constructive apraxia, articulatory apraxia, regulatory apraxia occur in children and adults? What is apraxia of walking and speech? What is the danger of motor left, right hand, left, parva leg, fingers, ideator apraxia? What are the principles for diagnosing apraxia ? Unfortunately, traditional methods, traditional medicine, diet, pills, medicines, drugs, traditional methods, spells, homeopathy rarely help in the treatment of apraxia. On the website sarclinic.ru you can see a doctor online for free.
Sign up for a consultation. There are contraindications. Specialist consultation is required.
Related posts:
Claude H Claude syndrome, alternating peduncular syndrome
Dysmorphophobia, treatment in Saratov, how to treat dysmorphophobia
Foville syndrome (ALF Foville) alternating pontine
Urination, urination mechanism, why does it happen, does urinary incontinence happen?
I'm afraid to speak, logophobia: treatment of logophobia for stuttering, the child is afraid to speak
Comments ()
Ataxias with oculomotor apraxia (AOA) are included in the group of autosomal recessive spinocerebellar ataxias (AR SCA, or SCAR: spinocerebellar ataxias, recessive). The name includes a characteristic symptom - oculomotor apraxia, manifested by difficulty in shifting and fixing gaze, inability to direct the eyes in the desired direction and not caused by weakness of the extraocular muscles.
Clinical descriptions of AOA appeared in the 80-90s, their full characteristics and molecular genetic interpretation date back to the 2000s. Known AOA type 1 (AOA1; OMIM 208920; APTX
encodes the protein aprataxin) and type 2 (AOA2; OMIM 606002; the
SETX
encodes the protein senataxin);
in 2012, AOA3 ( PIK3R5
) was described. Oculomotor apraxia is also typical of Louis-Bar ataxia-telangiectasia (LA). If AOA3 is so far represented by one family, then AOA1 and especially AOA2 are found everywhere and turned out to be quite common. In European countries, AOA2 becomes the second most common AR SCA after Friedreich's ataxia, ahead of AT [6, 35]. DNA analysis allows you to confirm the diagnosis and conduct medical genetic counseling with prenatal DNA diagnostics. However, at the pre-laboratory stage, many cases of AOA are detected late, which is partly due to the lack of awareness of neurologists about these relatively new forms, the features of clinical diagnosis (in particular, the need for targeted detection of oculomotor apraxia), and methods of genetic verification.
In Russian literature there is information about AOA [1] and a description of AOA2 in an Armenian family [2].
In the laboratory of hereditary metabolic diseases (HMD) of the Moscow State Research Center, DNA diagnostics of AOA1 and AOA2 has been started. The case of AOA2 presented in this article is the first Russian case confirmed by DNA analysis, and the first in the Russian population.
Patient A., 25 years old, a resident of Udmurtia, applied to the Medical Genetic Research Center (MGRC) with complaints of unsteady walking and weakness in the legs, difficulty writing, and unclear speech. Heredity is not burdened, the patient is the only child of Russian parents who are not related by blood. In childhood and adolescence he developed normally.
Instability manifested itself at the age of 18: during a medical examination at the military registration and enlistment office, while putting on shoes, he could not stand on one leg and fell; a neurological examination revealed ataxia. Then came weakness in the legs, impaired writing and speech. The patient's leading complaint at the time of admission for examination remained instability. For the last two years he has been walking with support. He was examined and treated in Russian and foreign (Israel, China) medical centers, where a hereditary disease was suspected, but the diagnosis was not established.
Condition on admission: stage I obesity, no telangiectasis, no somatic pathology; neurological status: when tracking the hammer, slight under-adduction of the eyeballs to the left; with voluntary eye movements in the main directions, oculomotor apraxia is detected with a significant slowdown of saccades: an attempt to look to the side is accompanied by a turn of the head with single irregular twitches, eye movements lag behind the turn of the head; mild cerebellar dysarthria; in the hands the range of motion and strength are not reduced; paresis of the legs in the supine position is not detected; tendon areflexia, abdominal reflexes are sluggish, distal pain hypoesthesia is pronounced, muscle-articular sensation in the legs is sharply impaired; with the finger-nose test - a mild intention tremor, with the heel-knee test - pronounced; gait is atactico-paretic, with support; in the Romberg test, as well as on the toes and heels, does not stand even with support; intelligence and memory are not reduced.
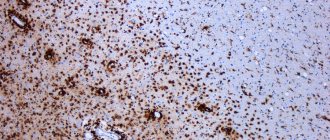
Additional diagnostic studies: fundus without pathology; MRI: moderate pancerebellar atrophy (see picture);
| MRI of patient A., 25 years old, with ataxia with oculomotor apraxia, type 2 (AOA2). |
| Note. Transverse and sagittal sections; cerebellar atrophy. |
ENMG: sensorimotor (more sensory) axonal polyneuropathy;
the immune status is not changed, the blood levels of lactate, albumin, cholesterol, and vitamin E are normal; serum α-fetoprotein (αFP) level is increased: 100 ng/ml (N≤10 ng/ml), CPK activity is slightly increased: 288 U/l (N≤190 U/l). Previously, a number of SCA and hereditary metabolic diseases were laboratory excluded: Friedreich's ataxia and autosomal dominant (AD) SCA types 1-3 - in the DNA diagnostics laboratory of the Moscow State Research Center; disorders of amino and organic acid metabolism, gangliosidosis GM1/GM2, Niemann-Pick disease C and SANDO syndrome (“spinocerebellar ataxia, neuropathy, dysarthria, ophthalmoparesis”) - in the laboratory of hereditary metabolic diseases of the MGNC; Refsum's disease, Wilson's disease and ataxia with vitamin E deficiency - in the medical center of Israel.
During an examination in Israel before this visit to the MGSC, AOA or a variant of AT were suspected, but the diagnosis was not confirmed.
A partial DNA diagnosis of AOA1 and AOA2 was carried out at the MGSC. APRX gene mutations
not found. In the SETX gene, direct sequencing of exons 6-8, where mutations are concentrated, revealed a previously undescribed mutation c.2623-2626 del 4 in a heterozygous state; the mutation results in a reading frameshift, which indicates its pathogenicity. Detection of one mutation with an appropriate clinical picture is sufficient to confirm the diagnosis of AOA2; the search for an allelic mutation, which requires sequencing of the entire gene and possibly the use of additional DNA analysis methods, has not yet been carried out. The parents do not plan to have children, but the prognosis of the offspring is of interest to the patient himself, and information about the low risk turned out to be important. Treatment of the patient remains symptomatic.
As can be seen from the signs of AOA2, summarized in the table,
| Table |
| ]]> |
The clinical picture in our patient is typical, but the diagnosis was established only after 7 years, although a hereditary etiology was assumed from the onset of the disease, and the examination went in this direction.
It should be noted that in previous descriptions of the patient’s status, OA was not indicated: either it formed later, as often happens, or it was not recognized. Indeed, OA can interfere with reading, but more often it does not appear in complaints, as in our patient, and requires targeted identification. A typical sign of OA is a significant slowdown and decrease in the amplitude of saccades - physiological rapid eye movements that occur when looking from object to object. If, to study gaze fixation and slow pursuit eye movements, the patient is asked to follow a small object (hammer) slowly moving in the main directions of gaze, then to study saccades - randomly move the gaze from one stationary object to another: in the center, above, below and along sides of the field of view. With oculomotor apraxia, patients are unable to carry out both tracking and especially saccadic eye movements on command. Dissociation of movements of the head and eyes is characteristic; with a voluntary gaze and an attempt to fix the gaze, the head “leads” the eyeballs, an excessive turn of the head towards the object occurs, jerky movements of the head are possible, a reflexive tonic turn of the eyes in the opposite direction, and only then a slow movement of the eyes towards the object occurs; “de-fixation” of an object is also difficult and requires auxiliary techniques (blinking, etc.) [1]. In AOA2, nystagmus, weakened optokinetic nystagmus, U-shaped impulses, convergent strabismus, and unilateral strabismus in combination with nystagmus are also described [21, 27, 32]. At the same time, the absence of oculomotor ataxia does not exclude AOA2: if with AOA1 it is present in all patients (although not from the onset of the disease), then with AOA2 it is present only in half, and in some samples it is much less common: in 32% of Algerian patients [32] , in 20% in the Italian group [16]; in 10 families from Quebec, oculomotor ataxia was absent (some of the 24 patients had nystagmus, some had strabismus) [18]. In this regard, some authors propose to abandon the name AOA2, replacing it with SCAR1 or SCAN2 (where N is neuropathy) [18], but the term AOA2 has rightfully stuck.
The age of onset of AOA2, according to summary data on 90 patients, ranges from 7-25 years (average 14.6 years) [7], in 10 Italian patients the range of age of onset is wider: 3-30 years (average 20 years) [ 16]. The first symptom is ataxia in the legs, which progresses and determines the severity of the disease; ataxia in the hands and dysarthria are expressed to varying degrees and may not be severe, as in our case. Axonal sensory-motor polyneuropathy, verified by ENMG, develops later, but in almost all patients (90-100%) and also contributes to disability; Sensitivity disorders can be severe, as in our patient [7, 16, 20]. Extrapyramidal symptoms (dystonia of the arms and trunk, chorea, head tremor) occur in 15-20% of cases; according to some data, they persist, but according to others, they decrease over time (as with AOA1) [5, 7, 23, 27, 32]. Some patients from Quebec had tremor, but it was intermittent and not severe [18]. 20% of patients exhibit pyramidal symptoms [7]. There are isolated cases of pelvic function disorders and dysphagia [25]. Intelligence in AOA2 is not reduced; some patients have mild cognitive impairment [16, 23]. Among the extraneural symptoms, hypogonadotropic hypogonadism in women (early menopause, polycystic ovarian dysfunction and dysfunction, secondary amenorrhea) has been described [24, 25].
Neuroimaging always reveals cerebellar atrophy, the degree of which varies from severe [25] to moderate, as in our patient, and even mild [1, 34], and not only depending on the duration of the disease.
A diagnostically important biochemical sign of AOA2, which distinguishes it from AOA1 and brings it closer to AT, is an increased level of AFP in the serum in almost all patients [5, 7, 12, 16, 18, 21, 32]. The AFP level may fluctuate with repeated measurements (it fluctuates normally), but the increase (> 20 ng/l) remains, although in general the numbers are lower than with AT. Interestingly, AFP was also elevated in 5 of 8 examined heterozygous carriers, and in three, it was within the normal range, but higher than in non-carrier relatives [5]. In some patients, CPK activity is slightly increased. A slight increase in the level of total cholesterol in the serum in some patients does not have diagnostic significance [23]. The disease progresses; by the age of 30, patients usually move on a chair, then the condition is relatively stable. Life expectancy is quite long; the recorded length of illness is 53 years. In general, the picture of AOA2 is quite uniform, including within families; as described by Bohlega et al. [12] Only one of the two sisters had OA, which may be due to the different duration of the disease.
There is no specific therapy for AOA2, as well as other AOAs and ATs.
The pathomorphology of AOA2, in addition to peripheral nerve biopsy, is presented by a description of a patient who died at 79 years of age from heart disease [16]. A decrease in the size of the brain was revealed with a pronounced expansion of the sulci of the hemispheres and atrophy of the cerebellum, especially at the level of the vermis and anterior lobe, a slight decrease in the size of the brainstem and spinal cord, histologically - a sharp decrease in the number of Purkinje cells in the cerebellar cortex, mild fibrous gliosis of the cerebellum (larger than the vermis), moderate a decrease in the number of neurons of the dentate nuclei, and in the spinal cord - a pronounced breakdown of the myelin of the gentle and wedge-shaped fasciculi, degeneration of Clark's columns with gliosis.
The AOA2 gene was mapped in 2000 [27] and identified in 2004 [26]. The senataxin protein belongs to the group of DNA/RNA helicases; it is presumably involved in the processing and biosynthesis of mRNA [1, 17]. Senataxin has been shown to be involved in the regulation of transcription [30], and it probably plays a role in neuronal differentiation [33]. SETX gene
contains 24 coding and 2 non-coding exons.
There are about 90 known mutations [22], and the new mutation in our patient adds to this number; a number of mutations have been described repeatedly. The mutational spectrum of SETX
is dominated by nonsense and missense mutations, splice site mutations, and small deletions and insertions; As with many other hereditary diseases, more and more data are emerging on atypical gene mutations - intragenic insertions, extended deletions and duplications (of one or more exons) not detected by sequencing [7, 8, 10, 11, 16, 32], some patients are homozygous for atypical mutations [10]. Due to the significant contribution of such mutations, it is recommended to begin DNA diagnostics of AOA2 with sequencing of all coding and flanking (border) intronic sequences, and if both mutations are not found, use multiplex ligase-dependent amplification (MLPA) and other modern additional methods of DNA analysis. Geno-phenotypic correlations were revealed: an analysis of 90 observations showed that missense mutations in the helicase domain cause a less severe phenotype than missense mutations outside this domain, as well as than deletions and mutations that shorten the protein [7].
AOA2, confirmed by DNA analysis, is described in most European countries, the USA and Canada, Japan, the countries of the Middle East, and Southeast Asia. The frequency of AOA2 is increased in Quebec due to a founder effect, most cases are associated with the Leu1976Arg mutation in the helicase domain, the frequency of the mutation in the French Canadian population of the region was 3.5% (1:47) [18]. In Alsace (Eastern France), the prevalence of AOA2 was about 1:400,000; among 57 cases of AR SCA confirmed by DNA analysis, AOA2 was 14%, ranking second after Friedreich's ataxia [6].
In addition to AOA2 mutation of the SETX
cause one of the forms of juvenile amyotrophic lateral sclerosis - ALS4 (OMIM 602433) [15]. This is a rare form of AD with severe distal weakness and amyotrophy, preserved sensitivity and pyramidal symptoms. The disease begins before the age of 25 and progresses slowly; the bulbar and respiratory muscles are not affected.
AD SCA, described in an African-American family, can also be considered an allelic form of AOA2 [9]. Two SETX
p.Asn603Asp and p.Gln653Lys, located on the same chromosome and being part of a common haplotype. The mother fell ill at the age of 13, the daughter at the age of 3, both had ataxia, cerebellar atrophy on MRI, tremor, and some signs of oculomotor apraxia, but there was no polyneuropathy, increased AFP and CPK. The authors suggest that the mutations, acting synergistically, lead to the formation of a protein with partially preserved function and the formation of AOA2 with an incomplete phenotype.
An interesting family with pseudodominant inheritance of AOA2 [29]: siblings aged 14 and 17 years and a 23-year-old paternal uncle had OA, severe ataxia and atrophy of the cerebellum, severe polyneuropathy with distal amyotrophy and high AFP. The disease was regarded as AD SCA with incomplete gene penetrance, but, having identified an increase in AFP, DNA diagnostics of AOA2 was performed:
The siblings were found to have compound heterozygosity for the single-nucleotide deletion c.2835delC, causing a reading frame shift, and the base substitution c.6106G>A; the uncle had homozygosity for c.6106G>A, probably due to distant consanguinity in the paternal branch of the family. Another feature of the case is the combination of symptoms of AOA2 and ALS4 (severe amyotrophy).
S.A. Klyushnikov et al. [2] described early-onset AOA2 in a non-inbred Armenian family in sisters aged 17 and 15 years. At 3 years old, ataxia appeared, at 6 years old - hyperkinesis, at 6-8 years old - strabismus and OA. As in our patient, other hereditary diseases were excluded for a number of years. AOA2 was confirmed at Tel Aviv University: immunobiochemical methods revealed reduced expression of senataxin with normal expression of aprataxin; high AFP also indicated AOA2; DNA diagnostics were not performed. We have not encountered any other observations by Russian authors.
The main characteristics of AOA1, AOA3 and AT are shown in the table. AOA1 was clinically described in the late 80s, the gene was mapped and identified in 2001-2002. [9, 28]. Typical onset is 4–5 years (range 1–16 years). Oculomotor apraxia always develops (often several years after the onset of ataxia) and progresses to external ophthalmoplegia. Hyperkinesis is present in more than 50% of patients, and unlike other symptoms, they often subside as the disease progresses. Walking is lost after 7-10 years. Possible cognitive impairment. Biochemical signs are hypoalbuminemia and hypercholesterolemia (but not at the onset of the disease). An important difference from AOA2 and AT is the normal level of AFP (although a slight increase was noted in some patients [13]). The frequency of AOA1 is increased in Japan and Portugal [14]; in Alsace, AOA1 ranks 4th in prevalence among NCA ARs [6]. Of 204 Italian patients with ataxia, AOA1 was diagnosed by DNA analysis in 13 (6%) [13]. In the NBO laboratory, AOA1 was confirmed in a 15-year-old Russian patient from the Altai region, who was not clinically examined by us: two previously undescribed mutations were found in a compound heterozygous state.
The allelic form of AOA1, ataxia with coenzyme Q10 deficiency (OMIM 607426), is highly variable clinically and genetically. APTX
is just one of several genes associated with this phenotype. Most often the disease begins in childhood, but there are also late forms. The clinical picture combines multi-symptom damage to the central nervous system and myopathy, as in many mitochondrial diseases; oculomotor apraxia is uncommon. Identification of this form is important not only for medical genetic counseling, but also from the point of view of treatment (coenzyme Q10).
In 2012, AOA3 was described in 4 siblings in an inbred family from Saudi Arabia [3]. The disease begins at 12-18 years of age and is similar to AOA2: ataxia, dysarthria, oculomotor apraxia, distal weakness (more legs) with amyotrophy, hypo-/areflexia and severe sensory disorders, intact intelligence, cerebellar atrophy on MRI, axonal sensorimotor neuropathy with ENMG, increased AFP, loss of walking in the 3rd decade. The gene was mapped to the 17p13.1 region and upon sequencing of all genes in the region, homozygosity for the Rro629Ser mutation in the PIK3R5
, presumably playing an important role in the development of the cerebellum.
The clinical picture of AT, one of the most common ARs in SCA, is well known. ATM gene
identified in 1995, but practical DNA diagnostics is difficult due to the large size of the gene and the variety of mutations in the absence of frequent ones. Direct DNA diagnostics of AT, which allows confirming the diagnosis, is not carried out at the MGNC; indirect DNA diagnostics (preclinical and prenatal), which is carried out in a DNA diagnostic laboratory, is possible only in families with an undoubted clinical diagnosis of AT.
Along with classical AT, there is a much rarer AT-like form (ATLD: AT-like disease, OMIM 604391), associated with the MRE11A
[28]. Differences from AT - less severity, absence of telangiectasia, normal AFP; other symptoms, including oculomotor apraxia, are similar. ATLD has been described in different countries, most often in inbred families [12, 19].
Slowing saccades is not pathognomonic for the presented forms. It is also characteristic of some SCA ADs (especially SCA2) [1] and has been described in Wilson’s disease. This is one of the main symptoms of SCAR4 (OMIM 607317), described in 5 siblings in a Slovenian family [31]: the disease begins in the 3rd decade, in addition to ataxia and oculomotor symptoms, it is manifested by polyneuropathy, pyramidal syndrome, mild myoclonus and mild cerebellar atrophy; the gene has been mapped but not identified.
Various oculomotor disorders are a diagnostically valuable symptom of many ataxias and NBO with ataxia. In addition to the most typical nystagmus, this is ophthalmoplegia, characteristic of some AD SCA (especially SCA9) [1], a number of mitochondrial diseases - Kearns-Sayre syndrome, SANDO syndrome (a new AR form associated with the mitochondrial polymerase gamma gene POLG), vertical ophthalmoparesis with Niemann-Pick disease C and others. When examining patients with ataxia, especially children and young people, it is important to pay close attention to a detailed study of oculomotor functions [1].
The SCA AR group, which includes AOA, has expanded significantly in recent years and continues to grow rapidly, facilitated by the development of molecular genetic technologies [4]. Most of the “old” and “new” SCA ARs and hereditary metabolic diseases with ataxia are accessible to practical DNA diagnostics and, therefore, genetic prevention (prenatal diagnosis); for some, specific treatment exists or is being developed (vitamin E deficiency ataxia, Refsum’s disease, abetalipoproteinemia , Niemann-Pick disease C, Friedreich's ataxia), therefore their timely detection by clinicians is of particular practical importance.
Diagnosis of pathology
Since the symptoms of the disease are very specific, the diagnosis is made already at the first visit to the doctor. A detailed examination is necessary only to establish the type of disease. To achieve this, the following activities are carried out:
- Studying the patient's medical history. This is necessary to identify the cause of the disease.
- Conducting collection and analysis of life history.
- Neurological examination of the patient.
- Assessment of the patient's performance of simple motor actions.
The information obtained allows the doctor to assess when the disease began to manifest itself and the severity of symptoms.
The patient is prescribed:
- Ultrasound;
- CT;
- MRI.
There is no special technique aimed at treating this disease. Patients are prescribed:
- drugs to restore cerebral circulation;
- nootropic medications;
- tablets to normalize blood tone.
Complex therapy necessarily includes:
- Physiotherapy.
- Massotherapy.
- Physical therapy courses.
- Occupational therapy.
- Consultations with a psychologist.
Treatment methods are selected individually depending on the type of speech, spatial or articulation disorders the patient has.
Associated disorders
The following disorder may be associated with apraxia as a secondary characteristic. It is not necessary for differential diagnosis:
Aphasia is an impairment in the ability to understand or use language. Usually occurs as a result of damage to the language centers of the brain (cerebral cortex). Affected people may choose the wrong words in conversation and have trouble interpreting verbal messages. Children born with aphasia may not speak at all. A speech therapist can assess the quality and extent of aphasia and help teach communication techniques to those people who most often interact with the affected person.
Causes
Apraxia results from a defect in the brain pathways that contain the memory of learned movement patterns. The damage may result from certain metabolic, neurological, or other disorders that affect the brain, especially the frontal lobe (inferior parietal lobe) of the left hemisphere of the brain. This region retains complex three-dimensional representations of previously learned patterns and movements. Patients with apraxia are unable to regain these stored skilled movement patterns.
Oculomotor apraxia is a dominant genetic feature. The gene for this condition was found on chromosome 2p13. Each chromosome has a short arm, designated "p", and a long arm, designated "q". The chromosomes are further divided into many bands, which are numbered. For example, "chromosome 2p13" refers to band 13 on the short arm of chromosome 2. The numbered bands indicate the location of the thousands of genes present on each chromosome.
Genetic diseases are determined by two genes, one from the father and the other from the mother.
Dominant genetic disorders occur when only one copy of the abnormal gene is needed to cause the disease. The abnormal gene may be inherited from either parent or may be the result of a new mutation (gene change) in the affected person. The risk of passing the abnormal gene from the affected parent to the offspring is 50% for each pregnancy, regardless of the sex of the child.
Tissue or cellular damage (lesion) to other specific parts of the brain, whether from stroke or injury, tumors or dementia, can also cause apraxia. These other locations include the so-called supplementary motor area (premotor cortex) or corpus callosum.
If apraxia is the result of a stroke, it usually improves within a few weeks. Some cases of apraxia are congenital. When a child is born with apraxia, it is usually the result of a malformation of the central nervous system. On the other hand, people with declining mental functioning (degenerative dementia) may also develop apraxia.
People with a condition of declining mental functioning (degenerative dementia) may also develop apraxia.
Description
Apraxia is understood as a motor impairment that cannot be explained by an underlying motor disability: there is no paralysis or incoordination. However, victims are unable to make voluntary, purposeful movements or handle objects (such as cutlery or tools).
Apraxia usually results from damage to the left side of the brain (for example, from a stroke). It usually affects both sides of the body and, in most cases, is accompanied by a simultaneous speech disorder (aphasia). Often apraxia is accompanied by paralysis of the right side of the body, so that the effects of dysfunction can only be seen on the left (still mobile) side.
Signs and symptoms
A key disability of patients with structural apraxia is the inability to copy or draw images correctly. There are qualitative differences between patients with left hemisphere damage, right hemisphere damage, and Alzheimer's disease.
Left hemisphere damage
Patients with left hemisphere damage tend to retain objects, simplify drawing elements, and omit details when drawing from memory. In addition, left-hemisphere patients are less likely to systematically arrange parts of their drawing.
Damage to the right hemisphere
Patients with damage to the right hemisphere cannot correctly reproduce the spatial relationships of complex figures. Elements of a design are often scattered, moved to different positions or orientations, or displayed diagonally on the page. As a result, right-hemisphere patients tend to produce asymmetrical or distorted drawings, characterized by hemispheric neglect, the absence of elements on one side of the model. It was once thought that right-hemisphere patients were twice as likely to make errors in 3D construction tasks as left-hemisphere patients, but this inaccurate finding was due to participant selection bias because researchers excluded people with severe left-hemisphere lesions from studies. -for the grueling speech of the devaluation of these individuals. However, the studies included people with severe right hemisphere lesions. Subsequent studies confirmed that there was no significant difference in the performance of left- and right-hemisphere patients on 3D construction tasks.
Alzheimer's disease
Alzheimer's patients with construction apraxia have unique symptoms. Their drawings contain fewer angles, spatial variations, lack of perspective, and simplifications that are not common in left-brain or right-brain patients. Structural disorders are present in the early stages of the disease and progress over time; however, even patients with advanced Alzheimer's disease can perform some constructive tasks. Spontaneous drawing is impaired early and is highly dependent on semantic memory; therefore, simplifications in the drawing may be due to limited access to semantic knowledge. As Alzheimer's disease progresses, the patient's ability to copy objects becomes increasingly impaired, and they may lose the ability to draw simple shapes correctly due to loss of motor skills in everyday memories.