What is hypothalamic syndrome?
Hypothalamic syndrome is a symptom complex of damage to the hypothalamic region, characterized by autonomic, endocrine, metabolic and trophic disorders.
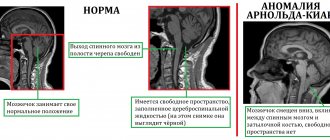
Various stressful situations, psychotraumatic effects, intoxication, traumatic brain injuries, vascular diseases, tumors, acute infections (influenza, ARVI (ARI), pneumonia, viral neuroinfections), chronic infections (cholecystitis, sinusitis, tonsillitis) play a significant role in the occurrence of hypothalamic syndrome. , rheumatism, tuberculosis). Increased vascular permeability of the hypothalamus can facilitate the penetration of toxins and viruses from the blood into the brain, and displacement of cerebrospinal fluid during traumatic brain injury can cause hypothalamic dysfunction. The occurrence of hypothalamic syndrome is also facilitated by hereditary and acquired constitutional defects of the hypothalamus and closely related structures of the limbic-reticular complex (limbic system and reticular formation) and the pituitary gland. Often, the pathological course of pregnancy and childbirth can be one of the factors of improper formation and maturation of the hypothalamus at various stages of fetal ontogenesis.
Sympathoadrenal crisis
Sympathoadrenal crisis in hypothalamic syndrome is manifested by severe headache, pain in the heart, palpitations, a feeling of fear, palpitations, a feeling of fear, difficulty breathing, numbness of the extremities. During a crisis, the skin is pale, dry, blood pressure (BP) is elevated, there may be slight hyperthermia (37.0; 37.1; 37.2; 37.3; 37.4; 37.5; 37.6; 37.8 ; 37.9 degrees Celsius), dilated pupils, increased erythrocyte sedimentation rate (reaction) (ESR, ROE), hyperglycemia (increased blood glucose levels). The attack often ends with chills, frequent urination (pollakiuria) or a single copious discharge of urine (polyuria).
Hypertensive cerebral crisis
Angiohypotonic crisis
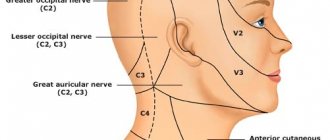
Angiohypotonic hypertensive cerebral crisis usually develops against the background of a typical and common headache for hypertensive patients, which is localized in the occipital region or occurs as a feeling of heaviness in the head.
A characteristic sign of such a headache is that it intensifies when the body is positioned in a way that impedes venous outflow from the cranial cavity (straining, bending, lying down, coughing). In itself, a headache of this nature is already a sign of angiodystonia of the cerebral vessels, but it often goes away in an upright position of the body and when taking caffeine-containing drinks. The onset of a hypertensive cerebral crisis is indicated by the spread of headache to the retro-orbital region. In this case, patients complain of pressure on the eyes and behind the eyeballs. A distinctive feature of angiohypotonic hypertensive cerebral crisis is its occurrence with a moderate increase in blood pressure (170/100 mm Hg). Next, there is a rapid (within an hour) intensification of the headache and its diffuse spread throughout the head. Nausea and repeated vomiting appear, bringing some temporary relief. Angiohypotonic hypertensive cerebral crisis is usually accompanied by autonomic reactions: increased sweating, tachycardia, wave-like breathing, and sometimes facial cyanosis. The late phase of the crisis is characterized by increasing lethargy, nystagmus, and dissociation of tendon reflexes. During this period, blood pressure can be at the level of 220/120 mm Hg. Art. or more, but in some cases it does not rise above 200/100 mm Hg. Art.
Ischemic crisis
Ischemic hypertensive cerebral crisis is observed much less frequently than angiohypotonic crisis and is typical mainly for hypertensive patients who do not suffer from headaches and tolerate increased blood pressure well. Often, ischemic hypertensive cerebral crisis develops against the background of very high blood pressure numbers, sometimes beyond the tonometer scale. Clinical manifestations of such a crisis may go unnoticed in the initial period. They relate mainly to mental disorders in the form of increased energy, excessive emotionality or external efficiency. Then irritability appears, giving way to depression and tearfulness, and possibly aggressive behavior. At the same time, due to the lack of criticism, patients themselves cannot adequately assess their condition.
Further development of ischemic hypertensive cerebral crisis is accompanied by the appearance of focal symptoms: visual impairment (flickering “spots” in the eyes, diplopia), sensitivity disorders (numbness, tingling, etc.), dysarthria (speech impairment), unsteady gait, vestibular ataxia, asymmetry tendon reflexes.
Complex crisis
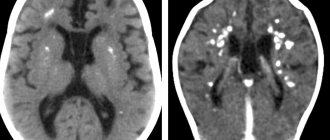
Complex hypertensive cerebral crisis begins with clinical manifestations characteristic of the angiohypotonic variant of cerebral crisis, but often occurs against the background of significantly elevated blood pressure. As the crisis develops, during the period of pronounced clinical manifestations, focal symptoms typical of the ischemic variant of cerebral crisis appear. In this case, the nature of the focal symptoms that arise depends on the location of the ischemic areas of brain tissue.
Neuroendocrine-metabolic form | Hypothalamic syndrome
The neuroendocrine-metabolic form of the hypothalamic syndrome is characterized mainly by endocrine disorders due to loss or increased secretion of hormones of the anterior pituitary gland.
The following diseases may occur.
Diabetes insipidus
1) diabetes insipidus (polyuria, polydipsia, dry mouth, general weakness);
Adiposogenital dystrophy
2) adiposogenital dystrophy - Pechkranz-Babinsky-Fröhlich syndrome (nutritional obesity, increased appetite, hypogenitalism, general weakness, various endocrine disorders);
Frontal hyperostosis
3) frontal hyperostosis - Morgagni-Stewart-Morel syndrome (hyperostosis of the internal plate of the frontal bone, amenorrhea, obesity, virilism);
Juvenile basophilism
4) juvenile basophilism - prepubertal basophilism (obesity, increased blood pressure / arterial hypertension /, stretch marks / stretch marks / on the skin;
Pituitary cachexia
5) pituitary cachexia - hypothalamic-pituitary cachexia, panhypopituitarism, Simmonds syndrome (rapid decrease in body weight by 1.5 - 2 times with the development of cachexia / exhaustion /;
Malignant exophthalmos
6) malignant exophthalmos - exophthalmic ophthalmoplegia (slowly progressive exophthalmos without thyrotoxicosis, at first it can be one-sided, oculomotor disorders, more often external ophthalmoplegia, diplopia, possible keratitis, atrophy of the optic discs);
Precocious puberty
7) premature puberty (pubertas praecox) - more often manifested in girls by the early development of secondary sexual characteristics, often combined with the following symptoms: high growth, bulimia, polydipsia, polyuria, sleep disturbance (insomnia), changes in the emotional-volitional sphere / children become rude, cruel, evil, have a tendency towards vagrancy, theft, antisocial violations/;
Delayed puberty
 delayed puberty – occurs mainly in boys during adolescence and is manifested by female-type obesity, hypogenitalism, lethargy, and decreased initiative;
delayed puberty – occurs mainly in boys during adolescence and is manifested by female-type obesity, hypogenitalism, lethargy, and decreased initiative;
Gigantism
9) gigantism is a disease that is characterized by the presence in adolescents and children of open epiphyseal growth zones with excessive secretion of self-tropic hormone (STH), height in boys and young men reaches more than 200 cm, and in girls and women more than 190 cm;
Acromegaly
10) acromegaly - Marie syndrome, or Marie-Lery syndrome - is a neuroendocrine syndrome caused by a significant increase in the secretion of somatotropic hormone of the anterior pituitary gland; the syndrome was first described in 1886 by P. Marie; and in most cases it is associated with an eosinophilic pituitary adenoma, sometimes acromegaly can develop after traumatic brain injury, intoxication, infection, stressful conditions; there is an increase in the size of the hands, feet, facial skeleton, nose, tongue, ears, and internal organs;
Dwarfism, dwarfism
11) nanism / dwarfism / - (nanos - dwarf) is a clinical syndrome manifested by extremely short stature (compared to the gender and age norm), occurs relatively often, causing mental distress in both the child and his parents, especially against the background acceleration in other children, often manifests itself in combination with other developmental defects (hydrocephalus, microcephaly, mental retardation, eye changes), in patients with chromosomal syndromes (Down disease, where, along with dwarfism, there are multiple developmental anomalies);
Itsenko-Cushing's disease
12) Itsenko-Cushing's disease (pituitary basophilism, Cushing's disease) develops due to excessive release of adrenocorticotropic hormone (ACTH) by the pituitary gland; first described by N. M. Itsenko and H. W. Cushing; occurs more often with basophilic pituitary adenoma, traumatic brain injury, inflammatory diseases of the brain, long-term use of large doses of corticosteroids or ACTH, manifested by symptoms of hypercortisolism (uneven obesity, moon-shaped face, fat deposits in the neck, upper half of the body, skin trophic disorders, osteoporosis , increased blood pressure, amyotrophy in the proximal limbs, intracranial hypertension, pyramidal and brainstem symptoms);
Lawrence-Moon-Bardet-Biedl syndrome
13) Lawrence-Moon-Bardet-Biedl syndrome is a hereditary diencephalic-retinal pathology, which includes Lawrence-Moon syndrome (first described in 1866 by JZ Laurence and R. Ch. Moon) and Bardet-Biedl syndrome (first described by G. Bardet in 1920 and A. Biedl in 1922), the type of inheritance is autosomal recessive and polygenic determination, the main symptoms of Lawrence-Moon syndrome are mental retardation, pigmentary retinopathy, hypogenitalism, spastic paraplegia, Bardet-Biedl syndrome - mental retardation, pigmentary retinopathy, hypogenitalism, obesity, polydactyly.
1.General information
The importance of the endocrine system in the life of the body cannot be overestimated. In fact, it is the second (after the nervous system) executive regulator of all physiological and mental processes. Each endocrine gland produces several hormones, and each of them, in turn, is involved in a complex cross-system of neurohumoral regulation. To date, not all relationships and interdependencies in this system have been discovered and studied, which further complicates the treatment of hormonal disorders and diseases, which are already characterized by polymorphism, therapeutic resistance, systemic and persistent (persistent) nature.
The adrenal glands are a paired gland that, like other endocrine glands, produces several hormones of different composition and purpose. The adrenal medulla produces adrenaline and norepinephrine (catecholamines), sex hormones, somatostatin and some neuroactive peptides; adrenal cortex - hormones of the corticosteroid group: aldosterone, corticosterone, deoxycorticosterone (mineralcorticoids), cortisone and cortisol (glucocorticoids). In general, the secretory activity of the adrenal glands is a key element of neurohumoral regulation: this gland controls emotions and digestion, cardiac activity and nervous system reactivity, the body's anti-inflammatory response and allergic receptor hypersensitivity, metabolic processes and connective tissue production, blood sugar levels and the expression of secondary sexual characteristics .
Therefore, any deviations and disturbances in the functioning of the adrenal glands are a serious, severe, and sometimes catastrophic problem for the entire body, and an abnormal decrease in hormonal secretion is just as dangerous as hypersecretion.
Chronic adrenal insufficiency is a severe polysymptomatic disease, named Addison's disease in honor of the outstanding English scientist of the 19th century, the father of endocrinology, Thomas Addison. An acute, crisis variant of adrenal cortex failure is named after him, in which the secretion of corticosteroids drops so sharply and quickly that the body does not have time to even partially adapt to hormonal deficiency - a life-threatening condition develops that requires emergency intervention.
A must read! Help with treatment and hospitalization!
Impaired thermoregulation, hypothalamic syndrome with impaired thermoregulation
Violation of thermoregulation of hypothalamic origin most often manifests itself in the form of prolonged low-grade fever, against the background of which hyperthermic crises sometimes occur with an increase in body temperature to 38.0 - 38.5 - 39.0 degrees Celsius. Unlike an increase in temperature during infectious diseases (diseases), this hyperthermia has a number of features and differences: an increase in temperature in the morning and a decrease in the evening, its relatively good tolerance, no changes in the blood and urine, a negative amidopyrine test, a perverted thermoregulatory Shcherbak reflex (with normal thermoregulation rectal temperature increases by 0.5 degrees Celsius after immersing hands in water at a temperature of 32 degrees and gradually increasing it to 42 degrees). Violation of thermoregulation can also manifest itself as hypothermia and poor tolerance to drafts, weather changes, and low temperatures.
Regional crises
Regional crises correspond to localized disturbances in the blood supply to an organ or tissue, depending on the type of angiodystonia. Hypertension of the artery (artoriole), sometimes reaching the level of vasospasm, is characterized by tissue ischemia due to a sharp restriction or cessation of blood flow; hypotension of the arteries is expressed by excessive inflow (hyperemia, local increase in temperature; pathological opening of the AVA - tissue ischemia with normal or increased inflow (the phenomenon of shunt "stealing" of capillaries); hypotension of the veins - by their overstretching, local stagnation of blood in the capillaries and pericapillary edema of the tissue.
The most common regional vascular crises in clinical practice include attacks of hemicrania during migraine and other types of so-called vasomotor headaches (see Hemicrania, Migraine neuralgia, Migraine), attacks of digital ischemia during Raynaud's disease and syndrome (see Rebno's disease), erythromelalgia and reducing acrocyanosis in angiotrophoneurosis, the so-called variant angina (caused by spasm of the coronary artery - see Angina), cerebral vascular crises in hypertension (see Hypertensive crises).
Neurotrophic form
The neurotrophic form includes various trophic disorders due to damage to the hypothalamus: trophic ulcers, focal or diffuse edema of different parts of the body (especially in combination with vegetative-vascular crises), brittle nails, osteoporosis, osteodystrophy, some types of alopecia /hair loss/. In its pure form, the neurotrophic form is rare, and trophic disorders are included in the structure of other forms of hypothalamic syndrome, more often in the neuroendocrine-metabolic form.
Neuromuscular form, catalepsy, narcolepsy | Hypothalamic syndrome
The neuromuscular form is manifested by general weakness, adynamia, and transient atypical attacks of catalepsy. Catalepsy (affective adynamia, emotional asthenia, affective loss of muscle tone, Levenfeld-Enneberg syndrome) is a short-term, paroxysmal loss of muscle tone, which occurs more often with strong emotional influences and leads to the patient falling without loss of consciousness. Catalepsy is a symptom of narcolepsy. Narcolepsy (Gelino's disease) is a disease from the group of hypersomnias, characterized by attacks of irresistible drowsiness and falling asleep during the daytime. Neurologists and neuropathologists distinguish essential narcolepsy, which occurs without visible external influences, and symptomatic narcolepsy, which occurs after infections, epidemic encephalitis, traumatic brain injuries, tumors of the 3rd ventricle, pituitary gland, internal hydrocephalus. Attacks of drowsiness occur suddenly, often in inappropriate conditions: while eating, walking, talking, urinating. The attacks usually last for several minutes. Depending on the external manifestations, neurologists distinguish 2 forms of narcolepsy: monosymptomatic, which is manifested only by attacks of falling asleep, and polysymptomatic, which is manifested by attacks of falling asleep, catalepsy, night sleep disturbances, and hypnogogic hallucinations.
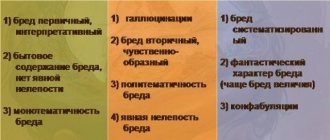
Hallucinations, Pickwissky syndrome, Kleine–Lewin syndrome
Hallucinations are false perceptions without a real object. Neuropathologists , neuropsychiatrists and psychiatrists distinguish between visual, auditory, olfactory, gustatory, tactile, and general senses. Hallucinations that occur while falling asleep are called hypnagogic. Hallucinations that occur upon awakening are called hypnopompic hallucinations. Movement disorders in the neuromuscular form of hypothalamic origin, they do not have a clear clinical picture and delineation, they are very variable, unstable, fragmented, and prone to paroxysmal progression. This same form includes some forms of phenocopies of neuromuscular diseases. Disturbances in sleep and wakefulness can be manifested by changes in the sleep formula (drowsiness during the day and insomnia at night), hypersomnia, narcolepsy, periodic hibernation syndrome, which is characterized by sleep attacks lasting from several hours to several weeks. At this time, muscle hypotonia, areflexia, arterial hypotension, and lack of control over the activity of the pelvic organs occur. More complex syndromes of sleep and wakefulness disorders may also be observed: Pickwickian syndrome , Kleine–Lewin syndrome. Pickwickian syndrome is a pathological condition of obesity in small people, manifested by shallow breathing, arterial hypertension (increased blood pressure), shortness of breath, drowsiness and general weakness. Kleine–Lewin syndrome is characterized by attacks of sleepiness with bulimia.
Clinical forms of hypothalamic syndrome rarely occur in isolated form. Thus, vegetative-vascular (vegetative-vascular) crises can be observed in neuroses, diseases of internal organs, vegetative-vascular dystonia (vegetative-vascular dystonia). Neuroendocrine metabolic disorders occur in other pathological processes of non-hypothalamic localization, as well as in primary endocrine diseases.
Symptoms of vascular crises
For a hyperkinetic crisis, its characteristics are especially important:
- This is the fastest type of crisis, characterized by a rapid rise in pressure to high levels;
- It is triggered by stress or strain;
- The main mechanism for the implementation of a crisis is vasospasm, which leads to an increase in pressure with a constant blood volume.
The approximate sequence of development of a hyperkinetic crisis is as follows:
- Initially, the patient experiences stress or performs physical work, which, by the way, is contraindicated for people with third degree somatoform autonomic dysfunction or arterial hypertension;
- The sympathetic nervous system is activated, the main effect of which is vasoconstriction;
- In parallel with this, there is an increase in heart rate. Against the background of coronary heart disease, this can lead to heart attacks, as well as vascular thrombosis;
- Due to the narrowing of the main blood vessels, a sharp increase in blood pressure is observed. Moreover, the volume of fluid in the vessels does not change, despite some expansion of peripheral vessels;
- The last stage is the main clinical manifestations and symptoms of dysregulation of blood pressure and vascular tone.
Hypokinetic crisis, also called water-salt crisis, develops in several stages.
- Accumulation of water due to chronic heart failure or chronic renal failure;
- Stretching of blood vessels and a slight increase in pressure;
- Compensatory increase in contraction of smooth muscles of arterial and venous vessels;
- Failure of compensation, depletion of the contractility of vascular smooth myocytes;
- Persistent dilation of blood vessels, further increase in pressure;
- Fluid effusion and the formation of edema of areas of the body with a gradual increase in pressure in the vascular bed;
- The formation of edema in the lower extremities, in the abdominal cavity, as well as in the brain in the hypothalamus;
- Activation of the vomiting center, formation of the main central symptoms of a water-salt crisis.
How to treat hypothalamic syndrome, how to get rid of hypothalamic syndrome!
Comprehensive differentiated treatment of patients with hypothalamic syndrome with the widespread use of effective techniques allows one to achieve good results even with severe symptoms.
At the first consultation, the doctor will tell you about the main factors and symptoms of the disease: what is hypothalamic syndrome in newborns, children, adolescents, adults (men and women), what is mild, moderate, severe hypothalamic pubertal juvenile neuroendocrine syndrome (neuroendocrine form) How the army, Wikipedia and obesity are related to hypothalamic syndrome.
Sign up for a consultation. There are contraindications. Specialist consultation is required. Photo: Dgm007 | Dreamstime.com\Dreamstock.ru. The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Depression, treatment of depression, how to get out of depression in Saratov
Phobia, fear, how to get rid of fear, how to overcome, treat and overcome fear, treatment in Saratov
Brain stroke: ischemic, hemorrhagic, treatment, rehabilitation, consequences
Obsessive neurosis: obsessive states, movements, treatment in Saratov, Russia
Urinary incontinence, treatment of women, men, children, adults, postpartum, neurogenic bladder, spina bifida
Comments ()
Sympatho-adrenal crises (panic attacks)
It is an uncontrollable, irrational, debilitating and very intense attack of panic and anxiety, which is accompanied by physical and psychological symptoms. The condition can affect cognition and behavior.
They are quite common in the population, in about 5% of cases and, most interestingly, they affect young working citizens from 20 to 40 years old, and women suffer from this disease 3 times more often.
Due to the huge number of similar symptoms, doctors of different specialties call panic attacks differently , but in general all these names are synonymous and very similar (therefore, in the text we will use all names):
- Vegetative crisis
- Sympatho-adrenal crisis
- Vegetovascular dystonia
- Cardiopsychoneurosis
- Cardioneurosis
I would like to immediately note that with adequate, timely, and most importantly comprehensive treatment of this problem, complete regression of symptoms , this will allow the patient to take control of mental processes and he will be able to continue to lead full life activities without compromising the quality of life. Unfortunately, if untreated , the disease can progress from rare, infrequent attacks to a chronic form , in which the frequency and severity of attacks constantly increases and can develop into more serious mental problems . Therefore, we advise you to make an appointment with our specialists - they very effectively treat panic attacks in Ust-Kamenogorsk at the Pulse center. Call and they will help you.
Before moving on to the manifestation of the disease, let us turn to a small classification for a better understanding.
There are 3 types of panic attacks.
- A spontaneous panic attack is the most unfavorable form of the disease, when the patient cannot identify a clear trigger factor after which the attack begins, and accordingly cannot prepare for it.
- Situational panic attack - has psycho-somatic “roots”, manifests itself in a specific traumatic situation or in anticipation of such a situation. Here are a few examples that our patients often tell: waiting for an exam, an imminent public speaking, a quarrel with loved ones, a premonition of conflict, stuffy spaces and even an unfamiliar environment.
- Conditional situational attack - in this case, a chemical or biological trigger is added to the psychological trigger. For example, drinking coffee, tea, alcoholic beverages, changes in hormonal levels, etc.
A little about the symptoms and pathogenesis of the disease.
What exactly happens to the body? What causes these symptoms? Why did this happen? These are the questions patients ask themselves and this is not surprising ! After all, the clinical picture of the disease can be very confusing and it is very difficult to understand it without the help of an experienced specialist.
The attacks are clearly somatic, i.e. physical and physical character, its symptoms are very reminiscent of a classic heart attack, accompanied by fear of death , etc., so patients may assume they have heart pathology (hence one of the names - cardiac neurosis). However, even the most severe manifestations of attacks are a consequence of an imbalance of the nervous and humoral systems. The main mechanism for the development of a crisis is the activation of the sympathetic nervous system and a powerful release of the “stress hormone” adrenaline - hence another name “sympatho-adrenal crisis”.
As we have already said, vegetative crises are characterized by an abundance of abruptly occurring symptoms. First of all, this is phobic anxiety , i.e. uncontrollable panic fear. As adrenaline is released, the heart rate pain in the chest and heart area may appear pressure rises. There is a chill, muscle tremors, the person sweats, the limbs turn pale, the mouth becomes dry, there is a lack of oxygen, it becomes difficult to breathe and the full picture ends with an unpleasant symptom - the fear of death appears.
Since the psyche is often involved, its short-term disorders can be observed: it seems to a person that all this is not happening to him, there is a feeling of the unreality of what is happening, one’s own mental processes are alienated, there is a fear of losing control of one’s behavior - such processes are called derealization and depersonalization.
The clinical picture and its severity have a wide range and vary greatly; there is even a so-called “ non-insurance ” form of panic attack or “panic without panic,” when physical disorders come to the fore.
Just like the symptoms, the duration of the attacks is variable. They can appear for a few minutes, or they can last for hours, but on average they last 15 – 30 minutes. The frequency of such attacks also does not have a clear relationship: for some it is once a month, for others it is 3 times a day.
Such crises, as a rule, are not isolated in nature. The experience of a terrible episode leaves an imprint on a person’s subconscious, because of this, a phenomenon called “fear of anticipation of an attack” is formed. This naturally creates a favorable background for more and more attacks. If a repeat of the crisis happens again and the conditions of the repeated attack are similar to the original ones, chronic panic disorder , and the patient develops “ avoidance behavior” - the person begins to consciously, independently avoid and limit his stay in potentially “panic situations.” All this can significantly complicate everyday life.
The causes of panic attacks as such are not fully understood, here are some possible ones:
- Violation of the circulatory system, in particular due to the vertebral arteries and pathological processes in the cervical spine.
- Hormonal imbalance, often involving the thyroid gland.
- Chronic somatic pathology, organic lesions of the central nervous system, recent infectious disease.
- Stress (positive and negative), being in an unfavorable environment (death of a loved one, frequent quarrels in the family, birth of a child).
- Improper upbringing, children's fears (excessive demands and criticism from parents).
- Peculiarities of mental functioning, personality traits, temperament.
- Genetic predisposition.
There is an interesting opinion that people who live in cities, who are intellectually developed, anxious and responsible by nature, are most often susceptible to the disease. There are practically no people with vegetative crises among residents of remote areas and villages.
Due to the multifactorial nature of the causes of the disease, only experienced specialists can . These are the doctors who see and successfully treat panic attacks at the Pulse Medical Center at the address: Ust-Kamenogorsk, Krasina St., 1.
Diagnostics.
This diagnosis can be established for the following objective reasons: repeated occurrence of an attack with an increase in peak at 10-15 minutes and the occurrence of at least 4 of the symptoms described above. But diagnosis is not so simple ; the difficulties lie in the fact that there are a large number of somatic diseases with a similar clinical picture. Many of them are potentially life-threatening and under-diagnosis would be a costly mistake. Here are some: bronchial asthma, angina pectoris, mitral valve prolapse, transient ischemic attacks, pheochromocytoma and others. Therefore, it is very important to consult a competent doctor who can rule out dangerous diseases and make a correct diagnosis. Our clinic successfully diagnoses panic attacks with the most confusing clinical picture and guarantees you highly qualified assistance.
How is panic attacks treated in Ust-Kamenogorsk?
After excluding other somatic pathologies and determining the cause of the disease, the turn of treatment comes. Since this disease affects the psycho-emotional sphere, we cannot do without rational psychotherapy . You should not be afraid of this, because in fact, the main therapeutic tool in such therapy is the use of reasoned logical influence on the distorted internal picture of the disease, the use of reason and thinking. With the help of a doctor, the patient learns to cope with his anxieties on his own and prevent crises from developing.
To restore the balance of excitation and inhibition processes in the nervous system, acupuncture , magnetic and laser therapy are used. Transcranial brain stimulation provides good results in the treatment of panic attacks.
If the cause is associated with hemodynamic disturbances at the level of the brachiocephalic arteries, then manual therapy, massage, and spinal traction are used.
The combined experience of our doctors, the ability to properly provide psychotherapeutic assistance, a large base of physiotherapy equipment and knowledge of reflexology allows us to successfully treat panic attacks in the Pulse center . In our clinic, any patient will be understood, supported and definitely helped. Make an appointment by calling 8-7