Facial nerve, anatomy
The facial nerve, nervus facialis , the 7th pair of cranial (cranial) nerves is a motor nerve.
The facial nerve innervates the facial muscles of the face (except for the musculus levator palpebre superioris), as well as the muscles of the auricle and skull, the posterior belly of the digastric muscle (musculus digastricus), the stylohyoid muscle (musculus stylohyoideus), the stapedius muscle (musculus stapedius), the subcutaneous muscle of the neck (musculus platysma).
The nucleus of the facial nerve is located on the border of the lower part of the pons with the medulla oblongata, outward and anterior to the nucleus of the abducens nerve. The axons of the cells of this nucleus rise in the dorsomedial direction to the bottom of the rhomboid fossa, then loop around the nucleus of the abducens nerve located here, forming the internal knee of the facial nerve in the area of the facial tubercle . The root of the facial nerve exits the base of the brain in the cerebellopontine angle between the pons and the medulla oblongata, lateral to the olive, then, together with its companions and the cochlear part of the 8th pair of cranial nerves, enters the internal auditory foramen (miatus acusticus internus), then the nerve and its companions enter facial canal (canalis facialis) of the pyramid of the temporal bone (fallopian canal). The canal initially has a horizontal direction (parallel to the apex of the temporal bone pyramid), then bends vertically. It then opens at the base of the skull with a stylomastoid opening (foramen stylomastoideum). The bend of the facial nerve in its canal is called the “external genu of the facial nerve.” In this place there is the knee ganglion (ganglium geniculi), where the cells of the first taste sensitivity neuron for the intermediate nerve are located. After emerging from the stylomastoid foramen, the facial nerve penetrates the parotid gland and divides into many terminal branches to innervate the corresponding muscles, forming the pes anserinus. The companions of the facial nerve in the canal are the parasympathetic lacrimal fibers - the greater petrosal nerve (nervus petrosus major) and the intermediate nerve (nervus intermedius), the 13th pair of cranial nerves, the Wriesberg nerve.
Parasympathetic lacrimal fibers originate from the secretory nucleus, which is located near the nucleus of the facial nerve. Together with the facial nerve, they enter the facial canal, then are the first to leave it as part of the nervus retrosus major, which innervates the lacrimal gland. Loss of function of the greater petrosal nerve is accompanied by the following symptoms - dry eye, eye irritation, lacrimation.
The intermediate nerve is mixed, consists of efferent parasympathetic salivary fibers for the sublingual and submandibular salivary glands, afferent taste fibers for the anterior 2/3 of the tongue. Salivatory fibers originate from the superior salivatory nucleus (nucleus salivatorius superior), leave the brain in the cerebellopontine angle and enter the facial canal next to the facial nerve, then leave the canal in its descending part as part of the chorda tympani (chorda tympani). Sensitive taste fibers begin from the cells of the knee ganglion, the dendrites of which go in the facial canal along with the facial nerve, then depart from it in the descending part of the canal, participate together with salivary fibers in the formation of the tympanic chord, then enter the system of the 3rd branches of the trigeminal nerve (nervus lingualis ) and reach the taste buds of the anterior 2/3 of the tongue. The axons of the cells of the knee bridle leave the pyramid of the temporal bone through the internal auditory foramen, pass through the cerebellopontine angle and end in the taste nucleus of the solitary tract (nucleus tractussoliterii), common with the glossopharyngeal nerve, located in the medulla oblongata. Damage to the intermediate nerve and the chorda tympani, which is its continuation, leads to hypofunction of the sublingual and submandibular salivary glands and impaired taste in the anterior 2/3 of the tongue. Between the two companions in the facial canal, motor fibers are separated from the trunk of the facial nerve, which form the stapedius nerve (nervus stapedius). The stapedius nerve penetrates the tympanic cavity and innervates the stapedius muscle, which provides a certain degree of fixation of the stapes and tension of the tympanic membrane, which creates conditions for the best audibility. Damage to the stapedius nerve is accompanied by a symptom such as hyperacusis. Hyperacusis is an increased unpleasant perception of sounds, especially low tones.
The first to leave the facial canal is the facial nerve's companion, the greater petrosal nerve. The second branch of the facial nerve to leave the facial canal is the stapedius nerve. The third to leave the facial canal is the companion of the facial nerve - the intermediate nerve in the form of the chorda tympani.
There are features of connections between the facial nerve and the cerebral cortex - the lower third of the precentral gyrus. The upper half of the nucleus, which provides innervation to the facial muscles of the upper part of the face, has a bilateral cortical representation due to the partial supranuclear decussation of the corticonuclear fibers. Fibers to the lower half of the nucleus, from which the facial muscles below the palpebral fissure are innervated, originate from the opposite hemisphere. This point is an important criterion in making a topical diagnosis.
Facial nerve: symptoms, lesion syndromes
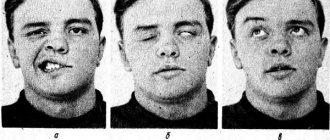
When the trunk of the facial nerve, the root of the facial nerve or the nucleus of the facial nerve is damaged, paresis of the facial muscles (muscle paresis) of the same half of the face develops - prosoplegia. Facial asymmetry occurs, which is pronounced even at rest. The entire affected side is motionless and mask-like. The forehead folds and nasolabial folds are smoothed. The palpebral fissure is widened. The corner of the mouth is downturned. Due to loss of function of the circular muscle of the eye (musculus orbicularis oculi), the eye does not close. This is lagophthalmos , or hare's eye. When you try to close your eyes, the eyeball on the affected side turns upward, the iris goes under the upper eyelid - Bell's symptom. With mild paresis of the orbicularis oculi muscle, the palpebral fissure closes, but less tightly than on the healthy side, the eyelashes remain visible (eyelash symptom). When the normal function of the lacrimal gland is preserved, lagophthalmos is usually accompanied by lacrimation, which is caused by difficulty in moving tears to the lacrimal canal due to insufficient adherence of the lower eyelid to the eyeball and impaired absorption due to displacement of the opening of the canal. Also, lacrimation is facilitated by the strengthening of the tear reflex due to the constantly open eye. Inflammatory phenomena, conjunctivitis, and keratitis often develop due to irritation of the eye membranes by air flow and dust.
The asymmetry of the face increases sharply when teeth are shown. The corner of the mouth is pulled back and it is skewed towards the healthy side - this is the phenomenon of the exclamation point, it is associated with paralysis of the musculus risorius. Due to the weakness of the orbicularis oris muscle, whistling and stretching of the lips into a tube are impossible. The patient often has difficulty speaking and eating. Liquid food on the affected side spills out of the mouth, thick food gets stuck between the cheek and teeth. When frowning and wrinkling the forehead, folds do not form on the side of paralysis, it is impossible to puff out the cheeks, and there is no tension on the musculus platysma of the neck. The brow reflex, nasopalpebral reflex, corneal reflex, and conjunctival reflex are lost or weakened. If damage to the facial nerve occurs in a child of the first year of life, then the sucking reflex, proboscis reflex, and search reflex are reduced. As with any peripheral paralysis, atrophy of the facial muscles is possible. When studying electrical excitability and myography, a degeneration reaction is noted.
Peripheral paralysis of the facial muscles is sometimes accompanied by pain in the face, ear, and mastoid process. The pain is associated with the phenomenon of repercussion. Repercussion is the irradiation of excitation from the motor branches of the facial nerve to the sensory branches of the trigeminal nerve.
Prolonged peripheral paralysis can lead to the development of contracture of the affected muscles, which is manifested by a narrowing of the palpebral fissure on the affected side and a pulling of the mouth when baring teeth towards the affected affected side. Symptoms of incipient contracture are often pathological synkenesis of the facial muscles - ocular synkenesis. They are characterized by the following symptoms. The closing of the eyes is accompanied by movement of the corner of the mouth or baring of the teeth. Baring your teeth causes the eye on the affected side to close.
In pathological processes that cause irritation of the nucleus or fibers of the facial nerve, facial hemispasm is observed - this is squinting the eye and pulling the mouth and tip of the nose to the affected side with simultaneous contraction of the chin muscles and tension of the subcutaneous muscle of the neck. Signs of irritation of the facial nerve are also tics of facial muscles and Chvostek's sign.
Intercostal neuralgia. Symptoms, diagnosis, treatment
Intercostal neuralgia, familiar to many of us firsthand, is designated by the medical term thoracalgia (from the Latin Thoracalgia chest pain), and is nothing more than compression and irritation of the spinal nerve roots.
Main symptoms: piercing acute pain, concentrated in the spaces between the ribs, encircling from the spine to the sternum, which intensifies with a deep breath, coughing, body movements, sometimes manifests itself in the back, neck, arm, under the shoulder blade, in the lower back. These symptoms are very similar to other, no less serious diseases, which is why it is so important to promptly contact a highly qualified specialist who can correctly make an accurate diagnosis.
In the chronic form, it is expressed in a constant pain syndrome, which can subside for an indefinite period of time, but always returns with greater force and consequences. To prevent the disease from becoming chronic, it is necessary to immediately seek help and begin proper treatment.
Why does the disease occur?
- wrong lifestyle;
- metabolic disease;
- spine pathologies;
- hormonal age-related changes, especially in women after 50 years;
- infectious diseases, including the herpes virus;
- physical activity on the upper body;
- hypothermia.
You should not make a diagnosis yourself and self-medicate, including folk remedies, but you should consult a neurologist as soon as possible. The Health Clinic employs highly qualified specialists; you can make an appointment with them at any time convenient for you.
It is important to understand that this disease will not subside on its own and will not disappear over time. If intercostal neuralgia is “neglected” and you do not receive qualified help from a competent neurologist in a timely manner, the pain syndrome will only intensify over time.
Consultation can be obtained by phone: +7(495) 961-27-67
Diagnosis of pathology
The symptoms of intercostal neuralgia are such that they can be signs of a number of other diseases, including cardiovascular diseases, so it is vitally important to get diagnosed by a specialized medical specialist, i.e. neurologist.
Mixed pain causes the greatest difficulties in diagnosis, because In this case, the patient has not one, but several reasons for complaints, and in order to identify the true cause, you need to have a reliable history, have a good laboratory base and the ability to use instrumental methods.
The Health Clinic has all the possibilities for this, since diagnosis is also our strength.
Diagnostic methods may include studies such as:
Standard set of laboratory blood tests;
- Electrocardiography;
- Ultrasound of the heart;
- Endoscopy;
- Gastroscopy;
- Chest X-ray.
- CT scan results may also be needed.
At the Health Clinic, if necessary, you can undergo any examination at a time convenient for you, using the most modern medical equipment, under the supervision of qualified specialists. A comprehensive examination will help the doctor make an accurate diagnosis and restore your health and freedom of movement. You can allow yourself the pleasure of a full life without pain.
Treatment with medications
Drug therapy is a mandatory part of a set of measures for recovery.
Products used:
- Anti-inflammatory – to relieve existing inflammation;
- Muscle relaxants – to relieve muscle spasms;
- Neuroprotectors – B vitamins aimed at protecting nerve cells;
- Chondroprotectors.
Complex treatment may include physiotherapy, massage, physical therapy, and manual therapy. Acupuncture (acupuncture) also gives very good results, a course of which can also be taken at
Competent treatment is the right path to recovery; it can only be prescribed by a good specialist with modern medical education, specialized qualifications and practical experience in treating this disease. Contact a neurologist at the Health Clinic, and your life will change for the better!
Application of physiotherapeutic methods
Physiotherapy is an effective treatment method that, in combination with drug therapy, gives excellent results with a correct diagnosis. This method is based on the use of physical phenomena such as ultrasound, magnetic fields, laser, and low-frequency currents. The most important advantage is the almost complete absence of contraindications.
Procedures included in the package of measures:
Laser. Laser physiotherapy has a beneficial effect on the blood circulation process, has an immunostimulating, anti-inflammatory, antispasmodic and analgesic, as well as a regenerative effect.
Magnet. Stimulates metabolic processes, blood circulation, synthesizes protein and some hormones, reduces blood pressure and muscle tone, has an analgesic and calming effect.
UHF – ultrasonic frequency. Activates the cellular reaction, enhances the body's protective properties. Has anti-inflammatory and analgesic effect.
DDT – diadynamic current. DDT helps activate local processes by stimulating lymphatic and blood circulation.
Electrophoresis. Administration of drugs through the skin and mucous membranes. Anesthetizes and regenerates.
Ultrasound. Ultrasound massage and phonophoresis (subcutaneous administration of drugs using ultrasound waves).
Forecast and prevention of the disease
The prognosis for the treatment of intercostal neuralgia is very favorable if the following conditions are met:
- A full examination to identify an accurate and comprehensive picture of the disease;
- A correct diagnosis must be made by an experienced, highly qualified medical specialist;
- Competently prescribed treatment, both medicinal and complex;
- Bringing complete treatment to the final result, i.e. patient's recovery.
Remember, intercostal neuralgia is not an incurable disease; it is important not to delay contacting a neurologist, otherwise, with a high probability, the disease will become chronic with an increase in pain until it is incompatible with a full-fledged lifestyle.
In order to prevent this disease, our experts recommend that you do not expose yourself to excessive physical exertion, give your body time to rest, consult a doctor for qualified help in case of any pain syndromes, if possible, protect yourself from stressful situations, and be attentive to your health during viral and infectious diseases. threats, avoid hypothermia.
Why are our neurologists better than others?
- The knowledge and experience of the doctors at our clinic allow us to achieve amazing success in the treatment of intercostal neuralgia.
- The Health Clinic has the most modern diagnostic equipment, which allows you to make an accurate diagnosis and begin treatment.
- Location in the very center of Moscow, within walking distance of two metro stations.
- Attractive prices
- Convenient time to visit a doctor.
We work to keep you healthy.
Consultation can be obtained by phone: +7(495) 961-27-67
Next.
article Prev. article
Diagnosis of the level of damage to the facial nerve
Isolated lesions of the nucleus of the facial nerve are observed quite rarely. It is manifested by total paresis of the facial muscles and occurs in the pontine form of polio.
More often, pathological foci localized in the pons are more common and lead to the involvement of the nucleus of the facial nerve, radicular fibers, and pyramidal tract in the process, which is manifested by alternating Millard-Hübler syndrome. Simultaneous damage to the nucleus of the abducens nerve is manifested by alternating Foville syndrome.
When the pathological process is localized in the cerebellopontine angle, the symptoms of damage to the facial nerve are combined with damage to its companions (the intermediate nerve and the greater petrosal nerve) and the vestibulocochlear nerve. Paralysis of facial muscles in these cases is accompanied by dry eyes - xerophthalmia, impaired taste in the anterior 2/3 of the tongue on the affected side. Xerostomia may be felt - dry mouth, but more often it does not occur due to the functioning of other salivary glands (parotid, sublingual, submandibular on the healthy side). Hyperacusis does not occur due to concomitant damage to the cochlear nerve. Hearing loss or deafness is more common. There may be signs of dysfunction of the trigeminal nerve and abducens nerve located in the immediate vicinity, as well as cerebellar disorders.
When the facial nerve is damaged in the facial canal above the origin of the greater petrosal nerve, dry eyes, taste disorders and hyperacusis develop simultaneously with paralysis of the facial muscles.
The lesion after the departure of the greater petrosal nerve is accompanied by increased lacrimation, taste disturbance, and hyperacusis.
When the facial nerve is damaged below the origin of the stapedius nerve, but above the origin of the chorda tympani, paralysis, lacrimation, and taste disturbance are observed.
Damage to the nerve in the bony canal below the origin of the chorda tympani or after exiting the stylomastoid foramen causes only paralysis with lacrimation.
When the process is localized in the area of the outer knee of the facial nerve with involvement of the knee node, Hunt's syndrome can be detected - this is paresis of the facial muscles (facial muscles), severe pain and herpetic rashes in the area of the auricle (ear).
Sometimes there are cases of bilateral damage to the facial nerve. Bilateral damage to the facial nerves is called diplegia facialis. The patient's face is mask-like, his eyes are half-open, it is impossible to form his lips into a tube or close his mouth.
Diagnosis of neuralgia
Our clinic has modern diagnostic equipment that allows us to make a diagnosis as accurately and quickly as possible.
| Type of neuralgia | Diagnostic tests |
| Trigeminal neuralgia | In typical situations it can be easily diagnosed by a neurologist. During the process:
To clarify the diagnosis, you may need:
|
| Intercostal neuralgia | For typical cases, the situation is the same as with trigeminal neuralgia: the diagnosis is made by a neurologist after examination, as well as based on the patient’s complaints. Diagnosis of intercostal neuralgia requires differentiating it from angina pectoris, ischemia, gastric ulcers and pancreatitis. For this, an ECG, fluoroscopy and magnetic resonance imaging of the thoracic spine are prescribed. |
| Neuralgia of the submandibular and sublingual nodes | The diagnosis is made based on the patient's complaints and the results of a neurological examination. Consultation with a dentist may be required. To clarify the diagnosis, a ganglion blockade is performed. |
Facial nerve: treatment in children
Damage to the facial nerve in children is more common than damage to other cranial nerves, which is due to its anatomical features. The facial nerve is supplied with blood from the external carotid artery system, therefore, when the head is hypothermic, spasm of the external carotid artery leads to nerve ischemia, swelling and compression of the facial nerve. Compression of the facial nerve develops especially easily when the process is localized in the narrow canal of the temporal bone pyramid. The facial nerve canal is connected to the tympanic cavity and the pneumatic cells of the mastoid process. The outflow of lymph from the trunk of the facial nerve occurs in the cervical lymph nodes. In childhood, damage to the cervical lymph nodes is often observed.
Treatment of the facial nerve at the Echinacea clinic
The treatment will be structured like this:
- Find and eliminate the factor that damaged the nerve (viruses, for example);
- Stimulate nerve regeneration.
If you neglect the first point, the chances of restoring the nerve are reduced, and the risk of facial contracture increases. The average duration of treatment is 2 months; you can complete most of the course at home on your own.
The planned result is restoration of the functioning of the facial muscles. Possible difficulties are advanced disease, significant narrowing of the facial nerve canal, damage to the myelin sheath of the nerve, leading to the appearance of a nervous tic of the eye, which to some extent complicates the treatment process. Read more about the causes and treatment of nervous tics.
Facial nerve: causes of damage, causes of neuritis, neuralgia, neuropathy, paresis, paralysis
The main causes of damage to the facial nerve a are inflammatory diseases (diseases) leading to primary damage to the facial nerve and its involvement in the process secondary to pathological changes in adjacent formations. Meningitis, arachnoiditis of the cerebellopontine angle, inflammatory processes in the area of the eustachian tube (eustacheitis) and mastoid process (mastoiditis), inflammation of the ear (otitis), jaw arthritis, lymphadenitis, mumps can cause the development of neuritis, paresis, paralysis, inflammation of the facial nerve. Also the cause of damage to the facial nerve are primary and secondary polyradiculoneuritis. Traumatic damage to the facial nerve occurs during traumatic brain injury with a fracture of the base of the skull in the area of the temporal bone, during surgical operations on the ear. The cause of paralysis and paresis of the facial nerve in children can be birth trauma, the application of obstetric forceps, or facial presentation. The facial nerve suffers from various tumors of the cerebellopontine ganglion region. Neuroma of the facial nerve, Recklinghausen's neurofibromatosis, tumor of the parotid salivary gland, infiltration due to leukemia are also causes of damage to the facial nerve.
In rare cases, congenital aplasia of the facial nerve nucleus and congenital narrowness of the facial nerve canal occur.
Neuralgia: causes
Most often, neuralgia affects nerves passing through canals and through openings that have a small diameter. She may be:
- Primary – appeared independently, not against the background of other diseases;
- Secondary – developing against the background of inflammation, tumor or other abnormal processes that negatively affect the nerve.
| Type of neuralgia | Initiating factors of development |
| Trigeminal neuralgia | In 95% it is initiated by compressive pressure on the trunk and branches of the nerve. The reasons for the development are the following:
|
| Intercostal neuralgia | The causes of intercostal neuralgia, which initiate compression of the nerve roots, are as follows:
|
| Neuralgia of the submandibular and sublingual nodes | The causes of intercostal neuralgia, which initiate compression of the nerve roots, are as follows:
|
Central palsy - facial nerve
Central paralysis of the facial muscles (facial muscles) is observed as a result of damage to the corticonuclear fibers going to the nucleus of the facial nerve. Central paralysis is characterized by dysfunction of the muscles of the lower half of the face, which have unilateral cortical innervation. The main symptom of central paralysis is the smoothness of the nasolabial fold on the side opposite to the lesion. In some patients with central paralysis of the facial muscles, mild deficiency of the orbicularis oculi muscle can be detected. Central paresis of the facial muscles is usually observed in combination with central hemiparesis, or hemiplegia. In contrast to peripheral paralysis, with central paralysis of the facial muscles, the conjunctival reflex, brow reflex, and corneal reflex are preserved, and there is no degeneration reaction.
Primary neuritis of the facial nerve
Primary facial paralysis is caused by herpes viruses, mumps, enteroviruses, and adenoviruses. Bell's palsy can develop with general or local hypothermia of the face. Bell's palsy is characterized by acute development within 3 to 24 hours. The leading role in the development of Bell's palsy belongs to ischemia, which develops due to vasospasm, or vasodilation with the development of swelling of the facial nerve and compression of the nerve.
Often, neuritis of the facial nerve occurs for no apparent reason against the background of absolute complete health. Sarklinik observed many cases where the first symptoms of facial neuritis appeared after a person slept, at the moment of awakening. This may be due to the activation of chronic infection with weakened immunity, the development of various allergic reactions.
Neuritis of the facial nerve secondary
Secondary neuritis of the facial nerve is most often of otogenic origin, observed after or during otitis, mastoiditis, eustacheitis. In these cases, reactive inflammation of the nerve trunk develops. Also, the inflammatory process can penetrate directly into the facial nerve itself due to the penetration of infectious agents into it. This is often observed with purulent epidemic partitis, lymphadenitis of the stylomastoid area. Secondary neuritis of the facial nerve can occur with infectious mononucleosis, toxoplasmosis, typhus, tuberculous meningitis, acute leukemia, cranial polyneuritis, polyradiculoneuritis.
Neuritis of the facial nerve occurs with fractures and cracks of the base of the skull passing through the pyramid of the temporal bone (post-traumatic neuritis of the facial nerve). Hereditary factors and congenital developmental anomalies play a major role in the occurrence of paresis of the facial muscles. There are aplasia of the facial nerve trunk and aplasia of the nucleus of the facial nerve. In this case, there may be unilateral and bilateral violations.
The occurrence of neuritis of the facial nerve is facilitated by a narrowing of the fallopian canal and an increase in the size of the styloid process.
Damage to the facial nerve can be one of the signs of such syndromes as Melkersson-Rosenthal syndrome, Mobius syndrome.
Neuritis of the facial nerve diagnosis
Diagnosis of facial nerve neuritis is based on an analysis of the symptoms preceding and accompanying diseases of the nerve damage. Neurologists, neuropathologists, and reflexologists distinguish such forms of damage as neuritis of the facial nerve and neuropathy of the facial nerve. According to pathogenesis, neuritis is divided into primary and secondary.
Neuritis of the facial nerve must be differentiated from isolated damage to the motor nucleus of the nerve, a variety of common pathological processes in the area of the cerebellopontine angle. Damage to the nucleus of the facial nerve is accompanied by isolated paresis of the facial muscles of the same half of the face without autonomic and sensory disorders, which occurs mainly in the pontine form of poliomyelitis or poliomyelitis-like diseases, tick-borne encephalitis.
When the lower parts of the bridge are damaged, which occurs with tumors, encephalitis, vascular diseases, along with the nucleus of the facial nerve, the pyramidal tract is involved in the pathological process. In such cases, peripheral paresis of the facial muscles is combined with central hemiparesis of the opposite side (Millard-Hübler syndrome). If the nucleus of the abducens nerve is affected, then paresis of the external rectus muscle of the eye (Fauville syndrome) is added to the above symptoms.
Isolated neuritis of the facial nerve is differentiated from processes in the area of the cerebellopontine angle, which develop, for example, with arachnoiditis, tumors of the vestibulocochlear nerve, which is manifested by decreased hearing, deafness, paresis of the facial muscles, sometimes dysfunction of the trigeminal nerve, contralateral spastic hemiparesis.
Polyneuritis and polyradiculoneuritis often involve lesions of the facial nerve. Usually the lesion in these cases is bilateral, often asymmetrical, accompanied by limited or diffuse damage to other parts of the human peripheral nervous system.
Neuralgia: symptoms
Clinical manifestations of neuralgia include pain symptoms. It manifests itself in attacks and affects the area of innervation. In addition, the patient may suffer from redness of the skin in the affected area, lacrimation, and convulsive muscle contractions.
| Type of neuralgia | Clinical manifestations |
| Trigeminal neuralgia | The syndrome is characterized by attacks of severe shooting pain along the line of the trigeminal nerve on the left or right. They can be short-term (lasting up to two minutes) or long-term burning pain (lasting up to three days). This symptom most often affects one side of the face. In addition, a spasm or tic of the facial muscles may develop. The pain may involve the eyes, jaws and ears. |
| Intercostal neuralgia | Symptoms of intercostal neuralgia are as follows:
|
| Neuralgia of the submandibular and sublingual nodes | It is characterized by the sudden development of pain symptoms affecting the submandibular area on one side. The anterior two thirds of the tongue hurt; the attack can last from a couple of minutes to one hour. In this case, irradiation to the neck, occipital and temporal regions is possible. Against this background, swelling of the tongue and the area under the lower jaw is possible, and there are disturbances in salivation. |