Paresis is an acquired or congenital defect of the nervous system.
Due to damage to the brain or spinal cord, a person is limited in professional and everyday activities. The main prerequisites for the appearance and transformation of paresis are hemorrhage or ischemia of the vessels of the spinal cord and brain. Limb paresis is a progressive, long-term disease. Without adequate treatment, it can result in serious complications, including complete loss of the ability to move. Therefore, it is important to contact a specialized clinic as soon as possible, identify paresis and treat it correctly.
Causes of paresis.
There are 2 types of neurophysical specific manifestations: organic and functional. With paresis of an organic nature, the physical relationship between the muscles and the brain is broken, which reduces the mobility of the limbs. For functional paresis, a distinctive feature is the identified destruction of the gray matter substance.
Depending on the area of influence and severity of the disease, they are classified by type of localization:
Tetraparesis: leads to weakening of muscles. It is expressed by increased tone, as a result of which the patient cannot move.
The formation of this type can be facilitated by chronic diseases, circulatory disorders, and the presence of injuries after neurosurgical treatment.
Weakening of all limbs occurs due to deterioration of the blood supply to the nerve fibers. Sometimes there is a deterioration in metabolism in the neural pathways of the gray matter.
Paraparesis: Affects the arms or legs on both sides of the body simultaneously, affecting the brain. It is provoked by tumors: they are also derivatives of osteochondrosis and spondylosis.
Hemiparesis: In this type, only half of the body fails. Then the power decreases: a defect in the muscles of the upper and lower extremities takes its place.
Hemiparesis tends to increase under the influence of diseases such as hemorrhage, tumor, head injury, and diabetic encephalopathy.
Monoparesis: with this disorder, attenuation of muscle activity in one of the limbs occurs. A similar type of disorder is caused by Brown-Séquard syndrome.
The causes of destruction of this type are inflammation of intracranial substances, botulinum toxin poisoning, damage to the skull, spine, abscess, stroke.
Why does muscle weakness occur?
Causes of weakness in the limbs
When considering the origin of skeletal muscle weakness, it is worth separating the concept of paresis associated with damage to nerve pathways and symptoms caused by defects in synaptic transmission and muscle damage. Often we are talking about blockade or increased destruction of acetylcholine, primary or secondary muscle pathology, reflex syndromes. Among the most well-known causes of weakness are the following:
- Myasthenia.
- Myasthenic syndromes:
Lambert-Eaton associated with slow closure of ion channels, familial infantile myasthenia. - Hereditary paroxysmal myoplegia:
hyper-, hypo- and normokalemic, Andersen-Tawil syndrome. - Infections:
botulism, tick-borne encephalitis. - Endocrine pathology:
hyper- and hypothyroidism, Conn's syndrome, Addison's disease. - Myopathies:
inflammatory (acute myositis, polymyositis, dermatomyositis), metabolic (including storage diseases), mitochondrial. - Muscular dystrophies:
progressive (Duchenne, Becker, Emery-Dreyfus), non-progressive (myotubular myopathy). - Diseases of the musculoskeletal system:
arthrosis, tendonitis, injuries. - Vascular pathology:
obliterating endarteritis, varicose veins of the lower extremities, Takayasu's disease. - Poisoning:
organophosphorus compounds, carbon monoxide, cyanides, aromatic hydrocarbons (toluene, benzene), plants (hemlock), nicotine, cocaine. - Taking medications:
D-penicillamine, antibiotics, antitumor drugs, statins, cortisone, colchicine, chloroquine.
Weakness in the muscles of the whole body is provoked by various systemic diseases and intoxications. It is noted in acute and chronic infections, autoimmune pathology, and malignant tumors. Low motor activity in older people, with immobilization, prolonged bed rest are common causes of widespread limb weakness.
Causes of facial muscle weakness
The facial muscles are innervated by the facial nerve (VII pair). Any pathology that disrupts the conduction of impulses along motor fibers - from the corticonuclear pathway to the peripheral part - can cause muscle weakness. It is also worth considering the direct damage to the muscles themselves. The list of probable pathologies includes the following conditions:
- Neuritis of the facial nerve (Bell's palsy).
- Facioscapulohumeral myodystrophy of Landouzy-Dejerine.
- Degenerative diseases:
progressive bulbar palsy, syringobulbia. - Tumors:
base of the skull (Garcin's syndrome), cerebellopontine angle, temporal bone and middle ear. - Hemorrhages and infarctions of the pons area.
- Congenital anomalies:
Chiari malformation, Klippel-Feil syndrome. - Infections:
herpetic ganglionitis of the geniculate ganglion (Ramsay-Hunt syndrome), polioencephalitis, Lyme disease, syphilis. - Meningitis:
bacterial, tuberculous, fungal. - Systemic pathology:
sarcoidosis, periarteritis nodosa, Behcet's disease. - Consequence of injuries, facial surgery, installation of a cochlear implant.
- The effect of chemotherapy drugs.
The facial nerve is often damaged by inflammatory processes in the ear and parotid salivary glands. Compression or rupture of its fibers is observed in TBI with a fracture of the base of the skull. The risk of facial nerve paresis increases in older people, with a long history of smoking, and the presence of concomitant pathologies (diabetes mellitus, arterial hypertension).
Causes of paresis
The upper or first neuron of the motor pathway begins in the motor cortex of the precentral gyrus, goes as part of the pyramidal tract through the internal capsule and trunk, ending in the anterior horns of the spinal cord. There, the impulse is transmitted to the second motor neuron, the axons of which make up the roots and peripheral nerves. Damage to these structures at any length is accompanied by paresis, which is typical for various pathologies of the nervous system:
- Strokes:
hemorrhagic, ischemic, subarachnoid hemorrhage. - Tumors and traumatic brain injuries.
- Demyelinating diseases:
leukodystrophies, multiple sclerosis, Devic's opticomyelitis. - Motor neuron diseases:
amyotrophic lateral sclerosis, spinocerebellar and bulbospinal atrophy. - Cerebral palsy.
- Neurodegenerative processes:
Wilson-Konovalov's disease, Shtrumpel's disease, Refsum's disease. - Myelopathy:
compression, spinal cord ischemia, transverse myelitis. - Damage to peripheral nerves:
polyneuropathies (metabolic, toxic, hereditary), tunnel syndromes, plexopathies. - Acute polyradiculoneuritis:
diphtheria, Guillain-Barré syndrome, ascending Landry's palsy. - Infections:
polio, meningococcal meningoencephalitis, rabies. - Vertebrogenic pathology:
intervertebral hernia, osteochondrosis, scoliosis. - Intoxication:
nerve poisons, salts of heavy metals (thallium, lead, arsenic).
Disturbances in spinal conduction are often caused by spinal cord injuries, which entail compression, ischemic damage, and swelling of the nervous tissue. There are also direct wounds - gunshots, bone fragments from fractures. Typically, the cervical spine is susceptible to such damage; the thoracic and lumbar spine are affected much less frequently. In case of concussion of brain tissue, the changes are transient in nature, in other cases they are more persistent.
Metastatic tumors (lung, breast or prostate cancer) are a common cause of compression of the spinal cord; lymphoma, multiple myeloma, and epidural hematomas are less common. If weakness appears in the arms or legs, tuberculous spondylitis, rheumatoid arthritis with subluxation of the atlantoaxial joint, and spinal vascular malformations are excluded.
Paresis of the feet.
Appears when trying to bend the knee. Difficulties in the flexion-extension functions of the femur and lower leg are visible to the naked eye. This is due to the weakness of certain muscle groups with normal dynamics in the distal sections. Traumatic factors affecting the integrity of the thigh fibers often cause peripheral proximal unilateral paresis.
With mononeuropathy of the femoral nerves, there may be a loss of sensation on the outer surfaces of the leg, as well as the front of the lower leg. The muscles become very tense, which limits their mobility. Extension of the lower leg is difficult.
As this type of paresis progresses, the personal or tibial muscle group is affected. It is impossible to move the foot, and after peroneal nerve dysfunction it is difficult to walk. By stepping on the heel, the patient is deprived of the ability to abduct the foot and raise its outer edge. The acuity of sensory perception on the inner side decreases. Due to the lack of timely qualified treatment, a “cock gait” develops.
Serious traumatic consequences can lead to significant problems in relation to the tibial nerve. Symptoms include difficulty flexing the sole, foot and hand. A person cannot stand on his toes; the Achilles reflex disappears. As paresis progresses, trophic ulcers may appear. Sensory sensitivity is also impaired in the plantar part, as well as in the area of the outer edge of the sole.
Sciatic nerve disease is often the result of injury. If the area and depth of the damage is large, then it is difficult to avoid loss of the hip bone. As a result of destruction, mononeuropathy of the sciatic nerve progresses. With complete loss of nerve fiber endings, absolute immobility can occur. However, the outer femoral surface remains intact and sensitive. The ability to perceive tactile stimuli on the back surface, as well as the sole, is significantly reduced.
How is paresis different from plegia?
Paresis is a decrease in muscle strength with partial loss of motor functions . Plegia is a complete loss of the ability to make purposeful movements of the affected limb or limbs and a lack of muscle strength. A synonym for plegia is paralysis . Paralysis can be considered the most severe form of immobility.
The causes and classification of plegia are the same as for paresis. The only difference is the severity of neuronal damage. Paresis can turn into plegia and vice versa.
Clinical picture of arm paralysis.
As paresis deepens, the variability and dynamic level of motor activity decreases, which is easily determined by a simple handshake. Often, a violation of muscle motility manifests itself without any specific underlying causes. The acute course of the disease signals trouble with a pronounced pain syndrome. Diseases in which nerve fibers rupture are often the result of a traumatic complication.
Failure in the distal region is called “Dejerine-Klumpke palsy.” Questions of this kind may arise due to injury to the child’s shoulder joint at the time of birth. With such stress, immobilization extends to the hands. The victim is unable to clench his fist normally, fold and open his palm, because... small soft structures of the hand disintegrate.
In case of paresis due to rupture of the ulnar fibers, acute pain in the muscles involved in straightening the hand and abduction towards the elbow is disturbed, and performance is lost. The little finger is immobilized.
If treatment is not timely, this can lead to atrophy and hypothenar.
In appearance, the hand resembles a clawed paw. In the main phalanges, the fingers are in an extended state, and in others they are bent; the paralyzed muscles dominate.
The manifestation of the disease is accompanied by a pronounced progression of polyneuropathy (nerve damage).
Symptoms
Newborns with paresis often have cerebral disorders: tremor, decreased muscle tone, increased excitability, suppression of unconditioned reflexes. All disorders are associated with the complex effect of birth trauma and asphyxia on the newborn’s body. These changes are transient in nature and quickly smooth out, which indicates a connection with impaired cerebrospinal fluid circulation and cerebral circulation.
The course of paresis depends on the severity of the lesion. With a small degree of damage, hand functions are restored starting from the first days of life and within 2-5 months active movements become full. In some cases of injury, muscle weakness may remain for a long time. It becomes more noticeable when the child begins to move to a vertical position, that is, sit or stand. Insufficient hand function is detected when the hand is raised above a horizontal position or the hand is pulled back. A decrease in muscle strength can be noticed when a child begins to reach for a toy.
In cases of moderate to severe lesions, recovery of arm function is slower and may be incomplete due to muscle atrophy, contractures and degeneration of nerve fibers. In cases of severe spinal cord injury, separation of roots from the spinal cord, rupture of the brachial plexus, restoration of arm function is minimal, atrophy and muscle contractures develop, and a tendency to dislocation in the shoulder joint is noted.
Diagnosis of paresis.
If symptoms appear that even remotely resemble paresis of the upper or lower extremities, only a specialist with extensive clinical experience can help.
The study may consist of collecting anamnesis and establishing a tendency to certain psychogenic reactions.
During the period of diagnosing the disease, the patient needs to answer the questions: how long ago did he first feel a narrowing of physical capabilities, does he have a history of benign or malignant brain tumors, purulent abscesses, poisoning (or a similar picture occurred in any of the close family members) .
An examination is required in which it is possible to find out the number of points scored during the assessment of muscle quality (0 - 3 points means strength is below normal).
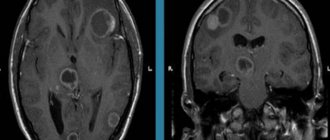
To detect possible inflammation, an additional general blood test is performed. To compile an anamnesis, the sick person receives a referral for toxicological analysis. It is important to evaluate electrical activity: for this, the doctor prescribes electroencephalography. To study the structures in detail, identify the specifics of diseases, and also determine the presence of abscesses, hemorrhages, neoplasms of various etiologies, you need to undergo computed tomography and magnetic resonance imaging and start normal treatment.
Types of paresis and trigeminal neuralgia
Despite the fact that cases of neuralgia and paresis of nerve bundles on the face were first identified and described more than 200 years ago, some questions about the etiology, development and treatment of the disease still remain open. In particular, doctors do not agree on what types of neuropathy can be divided into. But most experts are inclined to this classification:
- primary paresis: idiopathic, typical, effective. Develop independently of earlier diseases.
- secondary: symptomatic. They develop as a complex of symptoms caused by the primary disease and its complications.
Osteopathic methods.
Osteopathy views the body as an integral system capable of self-regulation and self-healing.
The healer’s task is to launch a mechanism that activates hidden reserves.
Due to the pronounced regression of paresis, all methods of osteopathy are involved in correction and treatment.
Structural:
the doctor uses it if there are issues related to the bones and ligamentous system. An osteopath uses various techniques that are similar to manual therapy.
Fascial:
works with soft tissues of the extremities. The organs affected by the pathology are restored through their synchronization, and blood flow improves.
Craniosacral:
harmonizes impulses of the brain and spinal cord in accordance with the biological rhythm. Used in the regulation of neurophysiological problems of the limbs.
Regenerative gymnastics.
An auxiliary section of the osteopathic method is physical therapy. It is indicated for any severity of paresis (even if the symptoms are such that the muscle problem prevents normal movement).
Exercises support the functioning of the vestibular apparatus, heart, blood vessels, normalize the musculoskeletal system, tendon-ligament structures, and joints.
It is important for the doctor to select a set of exercises to simultaneously use both arms and legs. It makes no difference whether the stiffness is unilateral or bilateral.
An osteopathic doctor selects the most effective methods of treatment, both modern and ancient. To formulate a more extended recovery course, it is necessary to keep in mind different approaches. Acupuncture – acupuncture therapy; Su Jok (translated as “hand and foot”) is a technique for influencing reflex zones; taping – fixation of joints using special plasters (kinesio tapes are used – a plastic material for joint regeneration, allowing flexion and extension of fixed joints).
Massage.
Massage is an auxiliary conservative osteopathic treatment that provides restorative measures by influencing organs through the surface of the body. With the help of special manipulations, it is possible to normalize the blood supply to cells and alleviate the condition of spasms. The person feels better. The procedure performed by an experienced specialist prevents degenerative-dystrophic prospects. To maximize the effect of the manipulations, sometimes additional vitamin preparations are prescribed.
Treatment is carried out in courses. Massage is performed on both sides - the healthy one and the one that needs to be treated. The specialist gently massages each one from bottom to top.
A person suffering from this disorder can independently relax the spasming muscles. These skills can be learned in the clinic.
To reduce muscle spasms, you need to gently roll the roller with your foot. Gentle movements will help relieve symptoms. The amplitude needs to be increased little by little.
It is important to take into account that in this case the treatment is carried out comprehensively with the use of reserve reserves of the whole organism.
It is a mistake to limit yourself to just massage or sports without the supervision of a doctor: you still won’t be able to get the expected therapeutic effect.
Facial nerve paresis: treatment in Moscow
Facial nerve palsy must be treated immediately. Otherwise, the pathology will progress and have a negative impact on the organs of vision (even blindness), and lead to irreversible damage to the nerve fiber. In Moscow, treatment of facial nerve paresis is performed at the Yusupov Hospital. Neurologists work in tandem with rehabilitation specialists and select the most optimal comprehensive treatment for maximum elimination of the disease. Teamwork of doctors, the latest diagnostic and treatment equipment contribute to high-quality treatment of facial nerve paresis.
Complex treatment will consist of the following elements:
- drug therapy (painkillers, vasodilators, decongestants are selected individually by neurologists at the Yusupov Hospital);
- physiotherapy (UHF, phonophoresis, paraffin therapy and other methods are performed in the rehabilitation clinic under the supervision of experienced rehabilitation specialists);
- massage (performed by professional massage therapists at the Yusupov Hospital, specializing in the elimination of neurological diseases);
- surgical intervention (used in complex cases).
Treatment of facial nerve paresis is recommended in a hospital. In this case, doctors can regularly monitor the body's response to the therapy used and quickly make adjustments to achieve better results. The inpatient unit at the Yusupov Hospital is equipped with everything necessary for a comfortable stay for the patient: comfortable beds, a bathroom with an individual hygiene kit, a wide-screen TV, wireless Internet, air conditioning, etc. A course of therapy at the Yusupov Hospital helps improve a person’s health and returns them to a full life.
You can make an appointment with neurologists, rehabilitation specialists, physiotherapists, massage therapists and other clinic specialists, get information about the work of the neurology clinic, rehabilitation, or clarify other questions of interest by calling the Yusupov Hospital.