Post-puncture syndrome
The symptoms of this syndrome are not caused by the extraction of cerebrospinal fluid during the puncture itself, but are the result of damage to the dura mater, which forms after insertion of the needle.
The entry of cerebrospinal fluid into the epidural space of the spinal cord contributes to the displacement and expansion of the dural sinuses and intracranial vessels. It forms several hours after lumbar puncture and has three degrees of severity:
- light;
- average;
- heavy.
This manifests itself as a headache in the occipital or frontal region, and in more severe cases, nausea and vomiting. Postpuncture syndrome lasts about four days, less often up to two weeks, and even more rarely more than two weeks. The use of needles of a smaller diameter or sharp disposable needles, turning the needle 90° during lumbar puncture (the bevel of the needle runs parallel to the fibers of the dura mater), and avoiding excessively accelerated flexion can reduce the incidence of post-puncture syndrome.
Chronic post-puncture syndrome is treated by injecting 10 ml of autologous blood into the epidural space, which promotes forced closure of liquorrhea. If conservative treatment is ineffective, direct surgery is indicated, in which the defect is closed with two special Cushing clips.
Ovechkin A.M.
Moscow Medical Academy named after. THEM. Sechenov
Osipov S.A.
Russian Medical Academy of Postgraduate Education
Judgments about the safety of anesthesia are based on data obtained from large retrospective studies, as well as individual reports of certain complications resulting from a particular method of anesthesia. When considering complications identified in the postoperative period, it is necessary first of all to establish their cause-and-effect relationship with anesthesia. There are known data obtained by Marinacci back in 1960 when analyzing the causes of neurological complications in 542 patients operated on under spinal anesthesia (SA). It was found that neurological deficit was a consequence of SA only in 4 (!) cases (Marinacci A., 1960). In the remaining patients, complications were caused by incorrect position on the table, the application of tourniquets with ischemia of the nerve trunks, direct surgical trauma, etc.
Epidemiology of complications of spinal anesthesia.
There are a number of key multicenter studies that determine the true picture of complications of SA. One of the most famous was completed in France in 1997 and included an analysis of the outcomes of 40,640 spinal anesthesia procedures performed over 5 months (Auroy Y., 1997).
Table 1
| anesthesia method | asystole | death | convulsions | spinal cord or root injury | radiculopathy | cauda equina syndrome | paraplegia |
| Spinal anesthesia (n=40,640) | 26 (0,06%) | 6 (0,01%) | 0 | 24 (0,06%) | 19 (0,05%) | 5 (0,01%) | 0 |
The study demonstrated an extremely low incidence of serious complications of SA. In particular, irreversible cardiac arrest was noted in 0.01% of cases.
An analysis of complications, which included more than 500,000 patients operated on under CA conditions, showed that the incidence of cardiac arrest varies from 0.04 to 1 case per 10,000 anesthesia (Aromaa U., 1997). Another large retrospective study identified 2 similar cases in 1881 patients operated on under SA conditions (Tarkkila, 1991).
A retrospective analysis of the incidence of cardiac arrests during anesthesia at the Mayo Clinic over 20 years (1983-2003) identified 26 asystoles during neuraxial anesthesia and 29 during general anesthesia (Kopp S., 2005). The incidence of this complication with neuraxial anesthesia was 1.8 per 10,000 patients, and was more common during SA than with epidural anesthesia (2.9 versus 0.9 per 10,000; P = 0.041). In 14 patients (54%) out of 26, asystole was directly related to the anesthesia technique (high upper level of sympathetic block, respiratory depression caused by the administration of sedatives), in the remaining cases (12 patients, 46%) it was caused by surgical factors (reaction to bone cement for joint replacement, manipulation of the spermatic cord, etc.). It is interesting to note that resuscitation efforts were more effective in cases where asystole occurred during neuraxial anesthesia (65% successful resuscitation compared with 31% with general anesthesia; P = 0.013).
Quite interesting are the data from an analysis of SA complications in 5 African countries (Senegal, Chad, Central African Republic, Niger and Madagascar), performed by French researchers (Carpentier J., 2001). In 2,703 CAs, only 40 complications (1.5%) were recorded, of which 5 were fatal (0.2%). The main cause of death in patients was asystole (4 out of 5). Most serious complications were noted during emergency cesarean sections performed against the background of severe hypovolemia. The authors consider the main reasons to be the low level of equipment of the clinics and low qualifications of the staff (a number of anesthesia procedures were performed by nursing staff).
In Sweden, all insurance claims from patients for the period 1997-1999 regarding SA were studied (Moen V., 2000). The incidence of neurological complications was 1:13,000 spinal anesthesia cases. There were 5 cases of meningitis (1:40,000).
Cardiac arrest during spinal anesthesia.
What are the key mechanisms of asystole during SA? What are the main risk factors? Old age and severe ASA status of patients play a negative role, but are not decisive.
Obviously, one should look for other causes of this formidable complication, associated, for example, with the peculiarities of the influence of SA on hemodynamics. Most of these effects are directly or indirectly caused by blockade of sympathetic efferents due to SA. It is known that the upper level of the sympathetic block is always 3-4 segments higher than the level of the sensory block, therefore, in a patient with a sensory block at the T4 level, the cardiac accelerating fibers coming from the T1-T4 segments will be almost completely blocked. Blockade of these fibers can cause severe bradyarrhythmia.
Even more important, SA-induced sympathetic efferent blockade is associated with decreased venous return to the heart. At the same time, the vagal influence on the heart increases significantly. It is known that at a low level of sympathetic block (below T4), the pressure in the right atrium can decrease by 36% of the original, and at a higher level of block - by 53% (Sansetta, 1952). Against the background of concomitant hypovolemia, these effects will be even more pronounced. In particular, with blood loss of 10 ml/kg of weight, the reduction in central venous pressure reaches 60-65%.
A decrease in preload activates reflexes that cause severe bradycardia. The first of these reflexes is associated with inhibition of the activity of centers of cardiac automatism, which increase the frequency of discharges depending on the stretching of the right atrium. Decreased venous return leads to a slower heart rate. The second reflex is determined by the activity of low pressure baroreceptors in the right atrium and vena cava. The third is the Bezold-Jarisch paradoxical reflex, the essence of which is the stimulation of the mechanoreceptors of the left ventricle, leading to bradycardia.
A decrease in preload can cause not only classic vagal symptoms (sweating, nausea, loss of consciousness), but also cardiac arrest. In this regard, patients with initially high vagal tone should be considered at risk for cardiac arrest during SA. The term "vagotonia" can be applied to patients with bradycardia at rest, atrioventricular block of varying degrees, or complete atrioventricular block. About 7% of the population belong to vagotonics; any procedure that stimulates vagal activity can cause asystole in them.
Severe bradycardia (<50 beats/min) against the background of SA develops in 9-13% of patients. Bradyarrhythmia is most often observed at a level of sympathetic block of T4 and above. In this case, 1st degree AV blockade may progress to 2nd degree blockade, and sick sinus syndrome may develop. Preoperative identification of risk factors is important. In particular, an initial pulse <60 beats/min is associated with a fivefold increase in the risk of developing severe bradycardia against the background of SA. Young patients are usually more prone to vagotonia, so their risk of developing bradycardia is three times higher. All risk factors for severe bradycardia (<50 beats/min) during SA are summarized below:
- initial heart rate <60 beats/min;
- taking b-blockers;
- sensory block level above T6;
- age < 50 years;
- prolonged PQ interval on the ECG.
When choosing an anesthesia method for each individual patient, these factors must be taken into account and analyzed. Quite often, two or even more of them occur in women in labor who are scheduled for SA during cesarean section. However, the physiological changes that occur in the body during pregnancy explain the low incidence of cardiac arrests during CA in obstetrics. Pregnancy is associated with changes in the autonomic control of heart rate, in particular, an increase in heart rate to 90-95 beats per minute is quite typical. This may be due to decreased parasympathetic tone during pregnancy.
Reducing the risk of asystole during SA can be achieved, first of all, by careful assessment of risk factors and appropriate patient selection. The second important point is infusion preload. Often it does not allow for rapid correction of developed hemodynamic disorders. In these cases, it is very important to notice and eliminate bradycardia in time. The first-line drug is atropine (0.4-0.6 mg), if necessary, ephedrine (25-50 mg) or adrenaline (0.2-0.3 mg).
Neurological complications in SA.
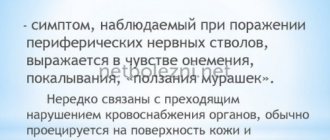
A retrospective study of 4767 patients who underwent SA found that 298 of them (6.3%) experienced paresthesia during subarachnoid puncture (Horlocker T., 1997). In the aforementioned Auroy study, two thirds of patients with neurological complications experienced pain with LA puncture or insertion. In all cases, neurological deficits developed in those innervation zones where paresthesia was felt. In this regard, it is believed that the presence of paresthesia during puncture is a risk factor for the development of persistent postoperative paresthesia. On average, the frequency of paresthesia during puncture of the subarachnoid space is 13-15%.
Post-puncture headache (PDPH). For many years, PDPH has been a fairly common complication of dural puncture and one of the main arguments of opponents of SA. Currently, its frequency has decreased significantly and averages about 3%, but varies significantly depending on a number of reasons.
In particular, the likelihood of developing PDPH increases in children over 10 years of age, peaks at age 15, and decreases significantly in patients over 50. In general, the incidence of PDPH is higher in women, and it especially increases during pregnancy. The most significant risk factor for PDPH is the diameter of the spinal needle and its type. Moreover, the type of needle (preferably needles with a tip in the form of a sharpened pencil, such as “pencil-point”) is more important than the diameter. Passing through the dura mater, such needles push its fibers apart to a greater extent than cross them, which facilitates rapid closure of the defect. Spinal needles of the “pencil-point” type and a diameter of 25-27G are optimal for SA.
Typically, PDPH develops within 12-48 hours after puncture and in 50% of cases resolves spontaneously within 5 days. By day 10, residual headaches persist in no more than 10% of patients who felt them on the first day after surgery. PDPH is quite intense and has a symmetrical nature (usually the forehead and back of the head). PDPH is often accompanied by nausea and vomiting. Sometimes there is decreased hearing, diplopia, and pain in the neck muscles. The pain intensifies when the patient is in an upright position and weakens in a horizontal position.
Mechanisms of occurrence of PDPH. Ideas about the mechanisms of PDPH are quite contradictory. Most often, its occurrence is explained by a decrease in subarachnoid pressure due to leakage of CSF through a puncture defect in the dura mater. If the flow of cerebrospinal fluid occurs at a rate exceeding its production (0.3 ml/min), there is a possibility of displacement (“sagging”) of intracranial structures with tension in the meninges and blood vessels rich in nociceptors, which is especially significant when the patient moves to a vertical position. The pain impulses that arise in this case are carried along the trigeminal nerve to the forehead, along the glossopharyngeal nerve, branches of the vagus nerve and cervical nerves - to the back of the head and neck. Some studies have confirmed a correlation between a decrease in subarachnoid pressure and the occurrence of headaches (Benzon H., 1996).
In some cases, patients with PDPH report some hearing loss. This effect is considered to be a consequence of changes in intracranial endolymphatic pressure and tension of the VIII pair of cranial nerves due to displacement of intracranial structures. The intensity of hearing loss correlates with the amount of CSF loss. Usually, hearing is completely restored after PDPH is relieved.
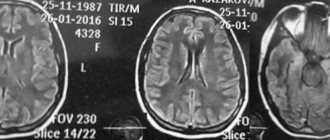
It is known that the introduction of autologous blood into the epidural space in most cases leads to relief of headaches. It is generally accepted that the therapeutic effect is due to an increase in both epidural and subarachnoid pressure, which normalizes the pressure gradient between the CSF, blood vessels and other intracranial structures. However, in reality, pressure increases only for a short period (a few minutes after epidural injection), therefore, normalization of CSF pressure is not the dominant mechanism for treating headaches. It is now established that the total volume of CSF loss does not correlate with the intensity of PDPH. It has been shown that in different patients with the same intensity of PDPH, the amount of fluid lost can vary from 10 to 110 ml (Iqbal, 1995).
There is an assumption that an acute change in CSF volume is only the primary initiating mechanism of PDPH (Raskin, 1990). Loss of CSF and changes in the pressure gradient along the intracranial venous vessels lead to their dilation. This fact is confirmed by the fact that compression of the jugular vein increases the intensity of pain (compression of the jugular vein causes venous dilatation).
In an experiment on monkeys, it was found that gradual removal of CSF leads to a decrease in CSF pressure and an increase in cerebral blood flow (Hattingh J., 1978). The compensatory dilatation of intracranial veins that develops in this case is obviously the main mechanism of PDPH. Low CSF pressure contributes to the development of PDPH, but is not the main cause. Cerebral vasoconstrictors such as caffeine and sumatriptan (used to treat migraines) are effective treatments for PDPH in most cases.
The dura mater is rich in adrenergic, cholinergic and peptidergic fibers, and the effect of xanthines on these systems is well known. Blockade of brain adenosine receptors by caffeine and theophylline leads to vasoconstriction. A sharp increase in epidural and subarachnoid pressure during filling with saline or autologous blood can deactivate adenosine receptors, which also leads to pain relief.
Thus, PDPH is based on several mechanisms; their combination with the predominance of certain factors can be variable and specific to each individual patient. Hence the varying effectiveness of standard treatments for PDPH.
Treatment of PDPH. Typically, conservative treatment of PDPH includes bed rest (2-3 days), oral or intravenous administration of analgin (500-1000 mg), caffeine (300-500 mg every 4 hours), sumatriptan. The effectiveness of caffeine therapy is estimated at 75-90%. If ineffective, the epidural space is sealed with saline or autologous blood. It is recommended to inject 8-10 ml of autologous blood one segment below the level of the previous puncture. The effectiveness of filling with autologous blood in the treatment of PDPH is estimated at 75-85%. A side effect of this technique is the occurrence of radicular back pain in approximately 50% of patients (usually resolves within a few days after filling). In this regard, to achieve the same effect, it is safer to use a similar injection of 10-20 ml of saline solution.
Toxic effects of local anesthetics.
Neurological complications in SA may be a direct consequence of LA neurotoxicity. According to histopathological, electrophysiological and experimental studies, lidocaine and tetracaine in clinical concentrations are more neurotoxic than bupivacaine and ropivacaine.
The aforementioned Auroy study found that 75% of neurological complications in SA occurred in patients who received high doses of hyperbaric lidocaine. One of the most striking manifestations of MA neurotoxicity is transient neurological syndrome. Transient neurological syndrome (TNS) was first described in 1993, when Schneider reported intense radicular back pain that developed in 4 patients after spinal anesthesia with hyperbaric lidocaine (Schneider, 1993). All these patients were in the lithotomy position on the operating table. Schneider called the pain described by patients “nerve root irritation syndrome.” Later, the current term - TNS - was proposed.
After activating patients in the postoperative period, there is usually a clear period of 2 to 5 hours, during which patients do not experience any pain. Then dull aching or shooting pains appear in the buttocks and lower extremities. The development of the syndrome is not accompanied by sensory or motor disorders, or dysfunction of the sphincters. The intensity of pain can be high (in 30% of cases > 8 points on VAS). According to one study, 14 out of 16 patients with TNS stated that the intensity of back pain was higher than pain in the postoperative wound (Pollock J., 1996). The duration of the pain syndrome can reach several days, rarely it lasts more than a week.
Epidemiology and risk factors. The frequency of TNS varies from 0.2 to 40% and depends on a number of circumstances. Risk factors for TNS were examined in a large multicenter epidemiological study that included 1863 patients (Freedman, 1998). It was found that the incidence of TNS when lidocaine is used for spinal anesthesia is an order of magnitude higher (11.9%) than that for bupivacaine (1.3%). The incidence of TNS is higher after operations performed on an outpatient basis, in obese patients, and in patients operated on in a lithotomy position (24.3%). Risk factors include early activation of patients after operations performed under SA.
Reducing the concentration of lidocaine to 0.5% is characterized by a slight decrease in the likelihood of developing TNS, although it is known that even 40 mg of lidocaine can cause this complication. Specifically, the same Freedman study noted that different doses of lidocaine (<50 mg, 50–70 mg, and >75 mg) were associated with similar rates of TNS.
Etiology of TNS. The mechanisms of TNS remain unknown. It is possible that it is the foot of the “pyramid” of MA neurotoxicity, the top of which is cauda equina syndrome.
It is not yet clear whether it is due to the direct neurotoxic effect of LA, a violation of the distribution of LA with the accumulation of its excess amount around certain neuronal structures, small hemorrhages, infection, direct trauma to the nerve root during puncture or during early mobilization.
It can be assumed that the lithotomy position is a factor that increases the neurotoxicity of lidocaine by tightening the cauda equina, reducing tissue perfusion and increasing the permeability of nerve fibers to the anesthetic. In addition, in the lithotomy position the lumbar curvature is straightened, thus creating a maximum concentration of LA around the sacral roots. During knee arthroscopy, the non-operated leg is usually flexed and fixed while the operated leg is manipulated. Both lithotomy position and manipulation during arthroscopy cause tension on the lumbosacral nerves. There are other assumptions regarding the etiology of TNS: direct neurotoxic effect, parallel administration of drugs such as cimetidine, metronidazole, the theory of hemolysis of blood entering the subarachnoid space, etc.
Prevention and treatment of TNS. Data from randomized trials indicate that symptoms of TNS develop in the vast majority of cases with the use of lidocaine and very rarely with the use of other MAs, especially bupivacaine (Hampl K., 1996, Pollock J., 1996; Ligouri G., 1998). At recent international forums devoted to the problems of regional anesthesia (I World Congress on Regional Anesthesia and Pain Treatment, Barcelona, 2002; XIII Congress of the European Society of Regional Anesthesia, Athens, 2004), symposiums were held under the motto: “Lidocaine should be banned √ for and against." Various opinions were expressed, resulting in the conclusion that the use of lidocaine for SA should be excluded in cases where there are risk factors for the development of TNS (outpatient anesthesiology, arthroscopic operations, overweight patients, etc.).
In cases where TNS does develop, non-steroidal anti-inflammatory drugs are used quite effectively to treat it.
Epidural hematoma.
The anatomy of the epidural space contributes to the development of complications associated with hemorheological disorders. The presence of large veins, which are often damaged by spinal needles, and the limited volume of the ED create conditions under which even a small hematoma puts pressure on the spinal cord and spinal roots. When this pressure exceeds the perfusion pressure providing blood supply to the spinal cord and/or pressure in the venous system of the spinal cord, ischemic damage to the spinal cord develops quite quickly. Epidural hematoma usually develops covertly; clinical signs may appear 3 days after ED puncture. More often, dysfunction of the pelvic organs, sensory disturbances and muscle weakness in the lower extremities develop primarily; pain occurs in no more than 50% of patients.
The true incidence of neurological complications caused by hemorheological disorders remains unknown. According to the literature, it averages 1:220,000-320,000 spinal anesthesia (Tryba M., 1993, Nociti J., 2002). The critical moment for restoring normal functions of the nervous system is the timing of decompression (laminectomy), which must be performed no later than 8 hours after the hematoma is diagnosed.
Risk factors and features of regional anesthesia.
The main risk factors are: initial disorders of the coagulation system, patients taking anticoagulant drugs for therapeutic or prophylactic purposes, the traumatic nature of puncture of the subarachnoid space (repeated attempts, injury to the vessels of the epidural space with a needle).
Features of anesthesia in patients receiving standard heparin. Short-term administration of heparin usually does not pose a risk for patients undergoing surgery under neuraxial anesthesia. Intravenous heparin should be delayed for at least 1-2 hours after subarachnoid puncture. In cases where the patient received heparin for several days before surgery, an aPTT study is advisable. Intravenous heparin infusion should be interrupted 2-4 hours before performing SA. There was not a single case of spinal hematoma in more than 5000 patients who received subcutaneous heparin to prevent thromboembolic complications (Schwander, Bachmann, 1991).
Features of anesthesia in patients receiving low molecular weight heparins (LMWH). Over the past 15-20 years, when LMWH became widely used in Europe for the prevention of thrombo-embolic complications, there was no increase in the number of spinal hematomas in patients operated on under neuraxial anesthesia. Although the true incidence of spinal hematomas during administration of LMWH and spinal anesthesia is difficult to determine, on average it is estimated to be 1 in 41,000.
Simultaneous SA is a fairly safe technique in patients receiving prophylactic doses of LMWH. It is recommended to perform a spinal puncture no earlier than 10-12 hours after the last LMWH injection. Those. A prophylactic injection of LMWH should be given the evening before surgery. In patients receiving therapeutic doses of LMWH, a longer delay is required to perform SA (24 hours). It is recommended to abandon SA if the patient received an LMWH injection 2-3 hours before surgery, since in this case the moment of puncture will coincide with the peak of the anticoagulant activity of the drug. In cases where the prevention of thrombo-embolic complications begins in the postoperative period, one-stage SA is an absolutely safe method of anesthesia. In this case, the first dose of LMWH should be administered no earlier than 10-12 hours after the end of the operation.
Thrombocytopenia. SA is considered safe when the platelet count is more than 100,000. It is undesirable to perform central blockades for thrombocytopenia < 50,000. When the platelet count is from 50,000 to 100,000, the issue is decided individually, taking into account all the positive effects of SA and the relative risk.
Non-steroidal anti-inflammatory drugs and aspirin. A number of studies have demonstrated the safety of performing neuraxial blocks while taking NSAIDs. In particular, a safety analysis of EA and SA in 1013 patients, 39% of whom were taking NSAIDs, did not reveal a single case of epidural hematoma (Horlocker, 1990).
Infectious complications of neuraxial anesthesia.
Infectious complications of spinal anesthesia include meningitis. In general, this complication occurs quite rarely. In a series of studies that included more than 65,000 SAs, 3 cases of meningitis were noted (Wheatley R., 2001).
Most often, meningitis is manifested by fever, intense headaches, meningeal signs, and impaired consciousness. Mortality reaches 30% even with adequate antibacterial therapy. For a long time it was believed that puncture of the dura mater was a risk factor. The mechanisms of this complication remained unknown, but it was believed that they were based on a violation of the integrity of the blood-brain barrier, as well as the entry of infected blood into the subarachnoid space during puncture. At the same time, it is known that diagnostic subarachnoid puncture is often performed in febrile patients with an infection of unknown etiology. In this case, there would have to be clear clinical evidence of the relationship between bacteremia and the incidence of postdural meningitis.
It is known that local anesthetics themselves have a bacteriostatic, and according to some data, a bactericidal effect. However, there is an opinion that neuraxial anesthesia should be avoided in patients with confirmed bacteremia who are not receiving antibiotics (and, in fact, is this possible in clinical practice?). SA can be safely performed in patients with signs of systemic infection if antibiotic therapy is started before puncture.
The source of infection may be exogenous or endogenous. The source of infection may be the oral mucosa of the anesthesiologist. The literature describes 4 cases of iatrogenic meningitis identified over a 4-year period in patients operated on under SA conditions (Schneeberger, 1996). In all cases, anesthesia was performed by the same doctor, who suffered from chronic pharyngitis and did not wear a mask during the procedure.
Thus, spinal anesthesia today is not only a highly effective, but also a fairly safe method of anesthesia, which is confirmed by evidence-based medicine. Basic safety conditions include: a) refusal to perform SA in the presence of absolute contraindications; b) strict adherence to aseptic rules; c) use of 0.5% spinal marcaine for SA, as the only drug recommended for this purpose.
Literature
1. Aromaa U., Lahdensuu M., Cozanitis D. Severe complications associated with epidural and spinal anaesthesias in Finland 1987-1993: a study based on patient insurance claims. Acta Anaesth.Scand. 1997, V.41: 445-452.
2. Auroy Y., Narchi P., Messiah A. Serious complications related to regional anesthesia. Anesthesiology. 1997, V.87: 479-486.
3. Benzon H., Nemickas R., Molloy R. Lumbar and thoracic epidural blood injections for the treatment of spontaneous intracranial hypotension. Anesthesiology. 1996, V.85: 920-922.
4. Carpentier J., Banos J., Brau R. Practice and complications of spinal anesthesia in African tropical countries. Ann.Fr.Anesth.Reanim. 2001, V.20: 16-22.
5. Freedman J., Li D., Drasner K. Transient Neurologic Symptoms after Spinal Anesthesia: An Epidemiologic Study of 1,863 Patients. Anesthesiology. 1998, V.89: 633-941.
6. Hampl K., Schneider M., Pargger H. A similar incidence of transient neurologic symptoms after spinal anesthesia with 2% and 5% lidocaine. Anesthesia.Analg. 1996, V.83: 1046-50.
7. Hattingh J., McCalden T. Cerebrovascular effects of cerebrospinal fluid removal. S. Afr. Med.J. 1978, V.54: 780-781.
8. Horlocker T., Wedel D., Offord K. Does preoperative antiplatelet therapy increase the risk of hemorrhagic complications associated with regional anesthesia? Anesth. Analg. 1990. V.70: 631-634.
9. Horlocker T., McGregor D. A retrospective review of 4767 consecutive spinal anesthetics: central nervous system complications. Anesthesia.Analg. 1997, V.84: 578-584.
10. Iqbal J., Davis L., Orrison W. An MRI study of lumbar puncture headaches. Headache. 1995, V.35: 420-422.
11. Kopp S., Horlocker T., Warner M. Cardiac arrest during neuraxial anesthesia: frequency and predisposing factors associated with survival. Anesthesia.Analg. 2005, V.100: 855-865.
12. Ligouri G., Zayas V., Chisholm M. Transient neurological symptoms after spinal anesthesia with mepivacaine and lidocaine. Anesthesiology. 1998, V.88: 619-623.
13. Marinacci A. Neurological aspects of complications of spinal anesthesia with medico-legal implications. Bull. Los Angeles Neurol. Soc. 1960, V.25: 170-192.
14. Moen V., Irestedt L., Raf L. Review of claims from the Patient Insurance: spinal anesthesia is not completely without risks. Lakartidningen. 2000, V.97: 5769-5774.
15. Nociti J. The anticoagulation controversy continues: how big is the problem? Highlights in regional anesthesia and pain therapy. Special Edition World Congress on Regional Anaesthesia and Pain Therapy - Barselona, Spain, 2002: 192-195.
16. Pollock J., Neal J., Stephenson C. Prospective study of the incidence of transient radicular irritation in patients undergoing spinal anesthesia. Anesthesiology. 1996, V.84: 1361-1367.
17. Raskin N. Lumbar puncture headache: A review. Headache. 1990, V.30: 197-200.
18. Sancetta S., Lynn R., Simeone F. Studies of hemodynamic changes in humans following induction of low and high spinal anesthesia. Circ. 1952, V.6: 559-571.
19. Schneeberger P., Janssen M., Voss A. Alpha-hemolytic streptococci: a major pathogen of iatrogenic meningitis following lumbar puncture: case report and a review of the literature. Infection. 1996, V.24: 29-35.
20. Schneider M., Ettlin T., Kaufman M. Transient neurologic toxicity after hyperbaric subarachnoid anesthesia with 5% lidocaine. Anesthesia.Analg. 1993, V.76: 1154-1157.
21. Schwander D., Bachmann F. Heparin and spinal or epidural anesthesia: decision analysis (review). Ann Fr. Anesthesia Reanimation. 1991, V.10: 284-296.
22. Tarkkila P., Kaukinen S. Complications during spinal anesthesia: a prospective study. Reg. Anesth. 1991, V.16: 101-106.
23. Tryba M. Epidural regional anesthesia and low molecular heparin. Anasth. Intesivmed. Notfallmed. Schmerzther. 1993, V.28: 179-181.
24. Wheatley R., Schug S., Watson D. Safety and efficacy of postoperative epidural analgesia. Brit. J. Anaesth. 2001, V.87: 47-61.
Regimen after lumbar puncture
Some doctors believe that bed rest does not prevent the development of post-puncture syndrome, and therefore they are allowed to walk immediately after a lumbar puncture. However, most of the authors conclude that bed rest has a positive effect, and the position of the patient and the duration of bed rest are discussed (most stopped at 3-4 hours). The patient should be in a horizontal position, lying on his stomach. After a lumbar puncture, general cerebral symptoms may occur (nausea, vomiting, headache, dizziness), in combination with the body’s autonomic reaction, it has a characteristic feature - deterioration when trying to get up. The patient needs to create peace, lower his head, offer plenty of warm drinks and (or) intravenous administration of plasma substitutes. When contrast agents or oxygen (air) are administered, bed rest can last up to three days.
What is a spinal tap?
A spinal tap, or lumbar puncture, is a minimally invasive, image-guided diagnostic procedure that removes a small amount of cerebrospinal fluid surrounding the spinal cord and brain or injects drugs or other substances into the lumbar spinal canal.
Cerebrospinal fluid (CSF) is a clear, colorless fluid that cushions the spinal cord and brain and delivers nutrients to them.
Up
To examine the thyroid gland, it is necessary
- Undergo an ultrasound examination of the thyroid gland. You should know:
with a small size nodule (cancer or nodule) there are no symptoms. - Nodules measuring 1 cm or more are subject to mandatory fine-needle aspiration biopsy (FNA) to determine further treatment tactics. Nodules measuring less than 1 cm can also be punctured, but after preliminary consultation with an endocrine surgeon.
- Further tactics are determined jointly by the endocrine surgeon or endocrinologist and the patient. It depends on the identified clinical picture, ultrasound and biopsy data (FNA), that is, on the exact diagnosis.
Our doctors - endocrinologist of the highest category Dublic Tatyana Gennadievna and endocrinologist of the first category Skuratova Olga Vladimirovna - individually select modern treatment tactics for each patient.
How should you prepare for research?
As a rule, before the procedure, a series of blood tests are performed to assess the function of the liver and kidneys, as well as the functioning of the blood coagulation system.
Often, a spinal tap reveals signs of increased intracranial pressure, for example, with hydrocephalus. Therefore, the patient may be given a CT scan before the study, which helps detect swelling of the brain or fluid accumulation around it.
It is very important to inform the doctor about all medications the patient is taking, including those of herbal origin, as well as any allergies, especially to local anesthetics, anesthesia drugs, or iodinated contrast materials. Some time before the procedure, you should stop taking aspirin or other blood thinners, as well as non-steroidal anti-inflammatory drugs.
It is important for the doctor to know about taking blood thinning drugs such as warfarin, heparin, clopidogrel, etc., as well as painkillers and anti-inflammatory drugs: aspirin, ibuprofen, naproxen, etc.
You should also tell your doctor if you have any recent illnesses or other conditions.
In addition, you should stop eating and drinking 12 hours before the procedure.
You should check with your doctor about what medications you can take in the morning.
It is advisable to come to the hospital with a relative or friend who will help the patient get home.
You must wear a special hospital gown during the procedure.
Women should always inform their doctor and radiologist of any possibility of pregnancy. As a rule, studies using x-rays are not carried out during pregnancy to avoid negative effects on the fetus. If x-rays are necessary, every effort should be made to minimize the effects of radiation on the developing child.
During a spinal puncture, a child is allowed to stay with one of the parents in the treatment room with prior agreement with the doctor.
Up
What are the benefits and risks of a spinal tap?
Advantages:
- After completion of the examination, no radiation remains in the patient’s body.
- When used for diagnostic purposes, X-rays do not cause any side effects.
Risks:
- Any procedure that involves violating the integrity of the skin carries a risk of developing infection. However, in this case, the chance of developing an infection that requires antibiotic treatment is less than 1 in 1000 cases.
- After a spinal puncture, bleeding with the formation of an epidural hematoma or subarachnoid hemorrhage is possible.
- In rare cases, a spinal tap is accompanied by compression of the spinal cord stem, caused by increased intracranial pressure, a brain tumor, or other lesion. The presence of high blood pressure can be determined by CT or MRI performed before the spinal puncture.
- With excessive exposure to X-ray radiation on the body, there is always an extremely small risk of developing malignant tumors. However, the benefits of accurate diagnosis significantly outweigh this risk.
- A woman should always tell her doctor or radiologist about the possibility of pregnancy.
A few words about reducing the effects of radiation on the body
During an X-ray examination, the doctor takes special measures to minimize exposure to radiation to the body while trying to obtain the best quality image possible. Experts from international radiological safety councils regularly review radiology standards and produce new technical recommendations for radiologists.
State-of-the-art X-ray machines allow you to control the dose of X-ray radiation and provide filtration, which minimizes beam scattering. In this case, the patient’s organs and systems that are not examined receive a minimal dose of radiation.
Up