Causes of headaches with normal blood pressure
If after measurement it turns out that the pressure is normal, but the head hurts, the symptom indicates various conditions and diseases. Often the pain goes away on its own after proper rest. If they occur frequently or are characterized by high intensity, they may be the first sign of dangerous diseases and require timely treatment.
Tension headaches
One common cause is tension headaches. They are symmetrical, begin in the frontal or temporal region, and then spread to the entire surface of the head. The pain is intense, pressing, and is sharply accompanied by additional symptoms such as nausea and increased sensitivity to light. Their reasons are:
- vascular spasms, as a result of which blood flows to the brain in limited volumes;
- tension in the muscles of the cervical spine, which also block the movement of blood;
- insufficient mobility of the neck and head during the day.
Tension headaches are often caused by stress, insomnia, and disruption of the daily routine. Antispasmodics, as well as proper rest, massage and gymnastics are recommended as treatment.
Infectious diseases
A common cause of headaches with normal blood pressure is viral diseases. During the cold season and in the off-season, there is a decrease in immunity, so outbreaks of ARVI and influenza often occur. At the initial stage, these diseases can manifest themselves as headaches, then characteristic symptoms increase:
- weakness, deterioration of health;
- increased body temperature;
- sore throat, cough, runny nose, difficulty breathing.
The main treatment method for viral diseases remains bed rest and drinking plenty of fluids. Additionally, vitamins, antiviral and symptomatic drugs are prescribed. Antibiotics may be required to prevent bacterial infection.
Allergy
If you have a constant headache, but your blood pressure is normal and other symptoms do not appear, this may be a symptom of an allergy. It is an increased sensitivity of the immune system to certain agents that normally do not cause rejection. Proteins that come from outside activate the immune system, and the body begins to fight them. This process is often manifested by a deterioration in health, headache, and swelling of the mucous membranes. Allergens can be foods, plant pollen, household dust, animal hair, and various chemicals. To eliminate symptoms, it is recommended to limit contact with confirmed allergens. If this is not possible, the patient must take antihistamines.
Diseases of the cervical spine
The cervical spine contains nerves and vessels that lead to the brain. Various anomalies of its structure, acute and chronic diseases cause disruption of the blood supply and innervation of the head, which is accompanied by intense pain. If your blood pressure is normal and your head hurts, you should undergo a cervical spine diagnosis to determine the following diseases:
- osteochondrosis is a chronic disease in which there is a decrease in strength, and then deformation of intervertebral cartilage;
- curvature of the cervical spine;
- protrusion and herniation of intervertebral discs;
- spondylosis – pathological immobility, fusion of adjacent vertebrae due to injuries and chronic diseases.
Diseases of the cervical spine require urgent treatment as they can progress with age. Tissues become less durable and elastic, inflammatory and degenerative processes worsen. However, proper treatment will stop the disease and prevent its further development.
Vascular diseases
Atherosclerosis is a dangerous chronic disease of the arteries. It is associated with impaired metabolism of fats, proteins and carbohydrates. Cholesterol and some fractions of lipoproteins accumulate in the blood. These compounds permeate the walls of blood vessels and are deposited on their inner surface, subsequently forming plaques. They interfere with the normal flow of blood through the arteries, so certain areas of the brain may experience chronic ischemia - oxygen starvation.
Typical symptoms of atherosclerosis depend on the site in which it develops. If it affects the vessels of the neck and head, the patient is bothered by constant headache, weakness and dizziness, hearing and vision impairment. Blood pressure indicators remain within normal limits. To treat atherosclerosis, a special diet and medications are prescribed that help eliminate excess cholesterol and harmful lipoproteins. Surgery may be required to remove large plaques that are dangerous.
Other reasons
Headaches can develop as a reaction of the body to any internal or external stimuli. At home, it is difficult to determine its cause unless other characteristic symptoms occur. Based on the results of the examination, it will be possible to understand how dangerous it is and choose the appropriate treatment.
There are several reasons why you have a headache if your blood pressure is normal:
- Intoxication is the accumulation of poisons and toxins in the blood and internal organs, including brain tissue. Poisoning can be caused by poor-quality food, medicines, toxic fumes from chemicals, animal and insect bites. Antidotes are used for treatment; if they are not available, gastric lavage, drip administration of electrolyte solutions and other detoxification methods are prescribed.
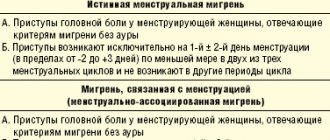
- Migraine is a chronic disease that manifests itself as headache attacks. Its exact cause has not been established, but a relationship with vascular disorders and hereditary predisposition has been proven. Before headache attacks, patients note a complex of characteristic symptoms, which includes dizziness, hearing and vision impairment, short-term memory loss, and loss of motor coordination.
- The consequences of injuries can manifest themselves even after many years. Traumatic brain injuries, including concussions and contusions, are accompanied by intense headaches. In the future, they worsen after physical and mental stress, in response to changes in atmospheric pressure and other factors.
Headaches with normal blood pressure often occur when work and rest schedules are disrupted. Stress, tension, insomnia, and night shift work lead to general fatigue and depletion of energy reserves. Doctors at the Clinical Brain Institute recommend timely prevention of diseases, normalizing your daily routine, and avoiding stressful situations.
Where does your head hurt and what does it mean?
- Where does it hurt: the whole head.
- What: Tension headache.
Monotonous, pressing, dull pain throughout the head. Tension headaches are accompanied by fatigue, weakness, nervousness, sleep and appetite disturbances, and increased sensitivity to bright light and loud sounds. The headache usually worsens in the evening.
The main causes of such pain are mental stress and prolonged muscle tension (sitting behind the wheel of a car, sitting at a computer monitor, reading a book, etc.).
What to do: take a hot bath and a sedative, watch a light movie, go for a walk, go to the pool or gym.
- Where it hurts: in the eye area, sinuses.
- What: sinusitis, nasal congestion.
When bending or suddenly moving the head, the pain intensifies. Often accompanied by an increase in temperature.
What to do: rinse and warm your nose, if necessary (sinusitis), take antibiotics prescribed by your doctor.
Sinusitis: causes, symptoms and types of inflammation Read more
- Where it hurts: headache in the back of the head.
- What : high blood pressure.
Pressing pain, accompanied by spots before the eyes, dizziness, and ringing in the ears. Occurs due to high blood pressure.
What to do: measure your blood pressure. Depending on the tonometer readings, either call a doctor, or an ambulance, or reduce the pressure using usual means.
Article on the topic
Brain catastrophe. What leads to a stroke?
- Where does it hurt : half of the head
- What : stroke
Acute growing pain in one half of the head is a serious sign of a stroke. Try smiling, raising your hands and saying your name. If you manage to smile with half your mouth, you can only raise one hand, there is porridge in your mouth, you need the help of a doctor.
What to do: Call an ambulance immediately! Remember that the therapeutic window for stroke (the time when medical care has the maximum effect) is about 4 hours.
- Where does it hurt : the whole head.
- What : hangover.
If you took a large amount of alcohol the day before, and the next morning you have a dull throbbing pain in your head, this is a hangover headache.
What to do: The best way to survive a hangover is to go to bed. If this is not possible, take a contrast shower, drink more, go out into the fresh air. As a last resort, you can take hangover medicine.
Sorry, I drank too much! How to relieve a hangover Read more
- Where it hurts: in the crown area.
- What : infections and viruses.
Headache is accompanied by nausea, dizziness, photophobia, tinnitus, and often fever. If there is no “accompaniment”, pain in the crown area may be a manifestation of cervical osteochondrosis.
What to do: keep bed rest, drink more (mineral water, green tea), in case of high temperature, take an antipyretic.
- Where it hurts: in the temple area.
- What : migraine.
Throbbing, increasing pain lasts from several hours to several days. In this case, a person reacts sharply to smells, light and loud sounds.
Migraines often occur after drinking red wine, aged cheese, or smoked meats. To achieve lasting improvement, it is enough to exclude these foods from your diet.
Question answer
Can perfume cause asthma and migraines?
What to do: Depending on the intensity of the pain, either use home remedies or consult a doctor.
Diagnostic methods
It is important to determine exactly why a headache occurs with normal blood pressure. It is impossible to conduct an examination at home. To accurately understand the cause of deterioration in well-being, additional techniques are prescribed:
- clinical and biochemical blood tests to assess the functioning of internal organs and the immune system, as well as additional studies to determine the level of hormones and microelements;
- examination of blood vessels using ultrasound with the addition of a contrast agent (Dopplerography);
- MRI of the brain is a method for detecting tumors, hematomas, areas of ischemia and other pathologies;
- examination of the cervical spine using radiography and MRI.
Diagnosis of headaches at the Clinical Brain Institute is fast and accurate. This is possible thanks to modern equipment, which allows you to get the most informative results in the shortest possible time.
Cardiovascular disease and anemia
The number of deaths from cardiovascular diseases (CVD) continues to rise worldwide. The conclusion that coronary heart disease (CHD) “... is the leading cause of death worldwide, its level is constantly growing and has now reached the proportions of a pandemic that knows no borders,” appeared on the website of the World Health Organization (WHO) in 2009 ., is perceived as increasingly relevant. In 2011, IHD caused the death of 7.3 million people [1, 2].
According to WHO estimates, 1.62 billion people suffer from anemia in the world [3]. The incidence of anemia, as well as coronary artery disease, increases significantly with age. More than 10% of people over 65 years of age and up to 50% of elderly patients with chronic diseases living in nursing homes have signs of anemia [4].
In the practice of general practitioners and cardiologists, a combination of cardiovascular pathology and anemia is often encountered. Anemia is detected in 25–40% of patients with chronic heart failure (CHF) and 10–20% of patients with coronary artery disease [5–7].
European and American recommendations for the management of patients with stable angina, issued in the last two years, require mandatory determination of hemoglobin levels in all patients and consider anemia as a factor provoking coronary insufficiency [8, 9]. In the latest recommendations for the diagnosis and treatment of patients with CHF, American and European experts note that anemia not only increases the symptoms of CHF, worsens the quality of life of patients, reduces exercise tolerance, and can cause the development of acute decompensation of CHF and an increase in the frequency of hospitalizations, but also an independent negative predictor of prognosis [10, 11]. The risk of death in CHF in patients with anemia is twice as high as without it, even when taking into account additional variables (renal dysfunction, severity of CHF, and others) [13]. Already latent iron deficiency can have a negative impact on the prognosis of CHF [14], which makes it advisable to determine its markers in all patients with CHF.
In acute coronary syndrome, the presence of anemia can quadruple the likelihood of death in patients and is considered an independent predictor of the risk of adverse clinical outcomes [15, 16]. Even chest pain syndrome in women, when combined with anemia, turns out to have a more unfavorable prognosis (the risk of death doubles) [17].
Preoperative anemia during cardiac surgery determines a high risk of subsequent blood transfusion and worse treatment results, which makes the task of early detection of anemia and high-quality, timely treatment urgent [18].
The role of anemia as an independent risk factor for poor prognosis in atrial fibrillation in elderly and senile people has been proven [19].
As shown by the analysis of the effect of the combination of anemia and impaired renal function on coronary artery disease in the population-based ARIC study (The Atherosclerosis Risk in Communities Study), anemia occurs in individuals with a slight and moderate decrease in renal function much more often than expected. And the combination of anemia and renal dysfunction significantly increases the risk of developing coronary artery disease, even after taking into account known risk factors such as diabetes mellitus, blood lipid levels, blood pressure and the use of antihypertensive therapy. The findings highlight the need for timely identification and treatment of anemia to improve patient prognosis [20].
The unfavorable mutual influence of CHF, anemia and renal dysfunction gave rise to the identification of new syndromes: “cardiorenal anemia syndrome”, “cardiorenal iron deficiency syndrome” and even “cardiorenal anemia and iron deficiency syndrome”. The latter terms emphasize the importance of iron deficiency as an independent risk factor for poor prognosis in CHF. The possibility of a direct effect of iron deficiency on diastolic function, hypertrophy, fibrosis and dilatation of the myocardium, the level of circulating erythropoietin, molecular signaling pathways and activation of inflammation has been proven in animal experiments [21]. This wide range of negative effects of iron deficiency is likely related to the role of iron in the body. It is not only part of hemoglobin and myoglobin, but is also found in enzymes involved in the conversion of adenosine triphosphate into adenosine diphosphate, promotes electron transport in mitochondrial chains, determines tissue metabolism and the absorption of free radicals [19]. Iron is involved in immune reactions and is necessary for the myelination of nerve fibers and DNA synthesis [22, 23].
Anemia in people with cardiovascular disease may have the same etiological factors as in the general population. An additional role in the development of anemia in cardiovascular pathology may be played by the older age of patients, which is itself associated with a lower hemoglobin value, the increasing incidence of chronic kidney disease, and the high prevalence of diabetes mellitus. It is assumed that the development of anemia in pathology of the cardiovascular system is contributed by: a chronic inflammatory process (increased synthesis of pro-inflammatory cytokines - tumor necrosis factor alpha, interleukin-6), ischemic depression of bone marrow hematopoiesis, decreased synthesis of endogenous erythropoietin due to renal dysfunction. In CHF, hemodilution with sodium and water retention and impaired absorption of iron and vitamins in the intestine may play a role in the formation of anemia. An additional factor for the development of anemia may be ongoing drug therapy that causes blood loss (when taking Aspirin, anticoagulants), a decrease in the production of erythropoietin and the sensitivity of the bone marrow to it (when using blockers of the renin-angiotensin-aldosterone system), etc.
The relevance of the issue of early diagnosis of anemia in patients with cardiovascular pathology is determined by the fact that its late detection leads to a delay or absence of the necessary intervention in relation to a potentially correctable condition.
A significant proportion of patients with cardiovascular pathology have latent iron deficiency, or iron deficiency anemia (IDA) or a combination of these conditions with other types of anemia.
Clinical signs of IDA consist of anemic and sideropenic syndromes, the latter is also determined by iron deficiency. Anemic syndrome may include the following manifestations: weakness, dizziness, syncope and orthostatic conditions, memory loss, epileptic seizures, symptoms of coronary insufficiency (anginal pain, repolarization disturbances on the ECG, arrhythmias), symptoms of myocardial insufficiency, systolic murmur on auscultation of the heart. Sideropenic syndrome leads to multiple disorders of various organs and systems. Lesions due to iron deficiency in the skin, skin appendages and mucous membranes (dryness, damage to hair and nails, etc.) are well known. No less common manifestations are symptoms from the gastrointestinal tract (decreased and perverted appetite, dysphagia, constipation or diarrhea, glossitis, burning tongue, esophagitis, dystrophic changes in the cells of the gastric mucosa); nervous system (increased fatigue, tinnitus, dizziness, headaches, decreased intellectual capabilities); cardiovascular system (tachycardia, diastolic dysfunction); urinary system (dysuria and urinary incontinence when coughing, laughing, nocturnal enuresis).
In the laboratory diagnosis of chronic IDA, microscopy of a peripheral blood smear reveals microcytic hypochromic anemia with hypoproliferation of reticulocytes. To confirm iron deficiency, reduced serum iron and ferritin levels are required.
Treatment of IDA is aimed at treating the disease underlying iron deficiency and actually compensating for iron deficiency.
Although patients with IDA need dietary advice, it is important to clearly explain that diet is not the basis of therapy. The largest amount of iron is found in meat (heme iron). All other foods contain less iron, and, most importantly, much less of them is absorbed (1–5% from apples, 10–15% from eggs and fish, and 25–30% from meat).
In drug therapy for IDA, the main focus has been and remains the use of iron supplements. The choice of iron drug is determined by its effectiveness (the amount and bioavailability of the iron it contains) and tolerability. An intake of 100 to 300 mg of elemental iron per day is required. The use of higher doses does not make sense, since iron absorption does not increase. Iron preparations on the domestic market are represented by hydroxypolymaltose complex, iron sorbitol complex, protein iron succinylate, iron sucrose complex. For patients with cardiac pathology, it is extremely important when carrying out additional drug therapy for IDA, in addition to high efficiency, the absence of negative drug interactions and good tolerability of the drug. The drug Maltofer, a polymaltose complex of iron sulfate (III), meets these requirements. Maltofer is a non-ionic iron preparation. Its absorption is ensured by active transport, without preliminary dissociation in the intestine, which eliminates the irritating effect on the mucous membrane and avoids most of the undesirable reactions from the gastrointestinal tract typical of ionized iron preparations [25, 26]. Maltofer does not interact with food or other medications, and the release form in the form of chewable tablets allows it to be used at any time and in any setting [27–30]. At the same time, the absorption of iron from other iron supplements may be reduced under the influence of substances contained in some foods - phytins (rice, soy), phosphates (fish, seafood), tannin (tea, coffee), while taking a number of medications (tetracyclines, antacids, calcium and magnesium salts), which requires taking these medications taking into account the time of consumption of food and these medications. Iron salt preparations contain divalent iron, which, after entering the blood, is converted into trivalent iron for its subsequent inclusion in the hemoglobin molecule, which can be accompanied by the formation of free radicals and have a negative effect on physiological processes in various organs and tissues [31]. Maltofer contains ferric iron, which is directly used to build the hemoglobin molecule, and therefore does not have a pro-oxidant effect [32]. When using iron supplements in adequate doses, a subjective improvement in well-being may be noted within a few days. The first objective criterion - reticulocyte crisis (an increase in the number of reticulocytes by 2-10 times compared to the initial one) is observed by the end of the first week of therapy. The absence of reticulocyte crisis indicates either an inadequate dose of the drug or an erroneous prescription of the drug. An increase in hemoglobin levels and the number of red blood cells is observed in the third week of therapy. After normalization of hemoglobin levels, a half dose of iron supplement is recommended for another 4–8 weeks to saturate the iron depot.
In 2013, the first recommendations for the treatment of anemia in patients with cardiovascular pathology were issued by the American College of Physicians [20]. They generally determine the tactics of managing a patient with cardiac pathology and anemia, regardless of its etiology. Three treatment strategies are considered: the use of erythropoietin-stimulating agents, red blood cell transfusion, and replenishment of iron deficiency. It is emphasized that red blood cell transfusion does not provide benefit and can cause harm to patients, so it is only possible in hospitalized severe patients with coronary artery disease with severe anemia. The use of erythropoietin-stimulating drugs for mild and moderate anemia in patients with CHF and coronary artery disease is not recommended due to the potential risk of thromboembolic complications and the lack of effect of therapy on the prognosis and frequency of hospitalizations. Positive data are currently available for the strategy of replenishing iron deficiency with intravenous administration of iron carboxymaltose; this tactic improves exercise tolerance, quality of life, reduces mortality and the frequency of hospitalizations [33].
Thus, anemia is a common comorbidity in cardiovascular diseases. Today in cardiology it is assessed as an independent predictor of the risk of adverse clinical outcomes, therefore patients with cardiovascular pathology need timely diagnosis of anemia in order to carry out adequate therapy.
Literature
- World Health Organization Cardiovascular diseases // Information bulletin No. 317. March 2013 [Electronic resource] - Access mode: https://www.who.int/mediacentre/factsheets/fs317/ru/ [Date of access: 10.04. 2014].
- World Health Organization 10 leading causes of death in the world // Information bulletin No. 310. July 2013 [Electronic resource] - Access mode: https://www.who.int/mediacentre/factsheets/fs310/ru/ [Access date: 04/10/2014].
- Worldwide prevalence of anemia 1993–2005. WHO Global Database on Anaemia. [Electronic resource] - Access mode: https://whqlibdoc.who.int/publications/2008/9789241596657_eng.pdf [Access date: 04/10/2014].
- Bross M.H., Soch K., Smith-Knuppel T. Anemia in older persons // Am Fam Physician. 2010. Sep 1; 82(5). P. 480–487.
- Boyd CM, Leff B, Wolff JL et al. Informing clinical practice guideline development and implementation: prevalence of coexisting conditions among adults with coronary heart disease // J Am Geriatr Soc. 2011. 59. P. 797–805.
- Felker GM, Adams KF Jr., Gattis WA et al. Anemia as a risk factor and therapeutic target in heart failure // J Am Coll Cardiol. 2004. 44. P. 959–966.
- Malyszko J., Bachorzewska-Gajewska H., Malyszko J. et al. Prevalence of chronic kidney disease and anemia in patients with coronary artery disease with normal serum creatinine undergoing percutaneous coronary interventions: relation to New York Heart Association class // Isr Med Assoc J. 2010. 12. P. 489–493.
- Stable Coronary Artery Disease (Management of). ESC Clinical Practice Guidelines. [Electronic resource] - Access mode: https://www.escardio.org/GUIDELINES-SURVEYS/ESC-GUIDELINES/Pages/GuidelinesList.aspx [Access date: 04/10/2014].
- Fihn SD, Cardin JM, Abrams J. et al. 2012 ACCF/AHA/ACP/FCP/AATS/PCNA/SCAI/ SNS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease // J. Am. Coll. Cardiol. 2012. Vol. 60. No. 24. P. e44-e164.
- 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. [Electronic resource] - Access mode: https://circ.ahajournals.org/content/128/16/e240.extract [Access date: 04/10/2014].
- Acute and Chronic Heart Failure. ESC Clinical Practice Guidelines. [Electronic resource] - Access mode: https://www.escardio.org/GUIDELINES-SURVEYS/ESC-GUIDELINES/Pages/GuidelinesList.aspx [Access date: 04/10/2014].
- Groenveld HF, Januzzi JL, Damman K. et al. Anemia and mortality in heartfailure patients a systematic review and metaanalysis // J Am Coll Cardiol. 2008. 52 (10). P. 818–827.
- Jankowska E.A., Rozentryt P., Witkowska A. et al. Iron deficiency: an ominous sign in patients with systolic chronic heart failure // Eur Heart J. 2010. 31 (15). P. 1872–1880.
- Meneveau N., Schiele F., Seronde MF et al. Anemia for Risk Assessment of Patients With Acute Coronary Syndromes // Am J Cardiol. 2009. Feb 15; 103(4). P. 442–447.
- Hasin T., Sorkin A., Markiewicz W. et al. Prevalence and Prognostic Significance of Transient, Persistent, and New-Onset Anemia After Acute Myocardial Infarction // Am J Cardiol. 2009. Aug 15; 104(4). P. 486–491.
- Arant C., Wessel T., Olson M. et al. Hemoglobin Level Is an Independent Predictor for Adverse Cardiovascular Outcomes in Women Undergoing Evaluation for Chest Pain. Results From the National Heart, Lung, and Blood Institute Women's Ischemia Syndrome Evaluation Study // J Am Coll Cardiol. 2004. 2, Jun 2; 43 (11). P. 2009–2014.
- Muñoz M, Ariza D, Gómez-RamÍrez S et al. Preoperative Anemia in Elective Cardiac Surgery: Prevalence, Risk Factors, and Influence on Postoperative Outcome // Transfusion Alternatives in Transfusion Medicine. 2010. 11 (2). P. 47–56.
- Sharma S., Gage B.F., Deych E. et al. Anemia: an independent predictor of death and hospitalizations among elderly patients with atrial fibrillation // Am Heart J. 2009. Jun; 157(6). P. 1057–1063.
- Astor B.C., Coresh J., Heiss G. et al. Kidney function and anemia as risk factors for coronary heart disease and mortality: the Atherosclerosis Risk in Communities (ARIC) Study // Am Heart J. 2006. Feb; 151(2). P. 492–500.
- Naito Y., Tsujino T., Matsumoto M. et al. Adaptive response of the heart to long-term anemia induced by iron deficiency // Am J Physiol Heart Circ Physiol. 2009. 296. P. 585–593.
- Ordway AG, Garry DJ Myoglobin: an essential hemoprotein in striated muscle // J Exp Biol. 2004. 20; 7. P. 3441–3446.
- Arredondo M., NbСеz MT Iron and copper metabolism // Mol Aspects Med. 2005. 26. P. 313–327.
- Ortiz E., Pasquini JM, Thompson K., Felt B. et al. Effect of manipulation of iron storage, transport, or availability on myelin composition and brain iron content in three different animal models // J Neurosci Res. 2004. 77. P. 681–689.
- Treatment of anemia in patients with heart disease: A clinical practice guideline from the American college of physicians // Annals of Internal Medicine. [Electronic resource] - Access mode: https://annals.org/article.aspx?articleid=1784292 [Access date: 04/10/2014].
- Geisser P., Muller A. Pharmacokinetics of iron salts and ferric hydroxide carbohydrate complexes // Drug Research 1987. 37. P. 100–104.
- Pestaner JP, Ishak KG, Mullick FG, Centeno JA Ferrous Sulfate toxicity. A review of autopsy findings // Biol Trace Elem Res. 1999. 69 (3). P. 191–198.
- Andrade JVD, Rodrigues PPB, Fontoura IB et al. Tratamento da anemia ferropriva com hidroxido de ferro polimaltosado - Estudo multicêntrico comparativo entre tratamento ministrado com e sem alimentação concomitante // Arq bras Med (Suppl). 1992. 66. P. 253–258.
- Funk F., Canclini C., Geisser P. Interactions between iron (III)-hydroxide polymaltose complex and commonly used medications. Laboratory studies in rats // Arzneimittel-Forschung (Drug Research). 2007. 57 (6 a). P. 370–375.
- Potgieter MA, Potgieter JH, Venter C., Venter JL, Geisser P. Effect of oral tetracycline on iron absorption from iron (III)-hydroxide polymaltose complex in patients with iron deficiency anemia. A single-centre randomized controlled isotope study // Arzneimittel-Forschung (Drug Research). 2007. 57 (6 a). P. 376–384.
- Burckhardt-Herold S., Klotz J., Funk F. et al. Interactions between iron (III)-hydroxide polymaltose complex and commonly used drugs. Simulations and in-vitro studies // Arzneimittel-Forschung (Drug Research). 2007. 57 (6a). P. 360–369
- Hutchinson C., Al-Ashgar W., Liu DY et al. Oral ferrous sulphate leads to a marked increase in pro-oxidant nontransferrin-bound iron // Eur. J. Clin. Invest. 2004. 34. P. 782–784.
- Geisser P. Safety and Efficacy of Iron (III) hydroxide Polymaltose Complex. A review of 25 years experience. Arzneimittel-Forschung (Drug Research) 2007. 57 (6 a). P. 439–452.
- Anker SD, Comin-Colet J., Filippatos G. et al. Ferric Carboxymaltose in Patients with Heart Failure and Iron Deficiency // N. Engl. J. Med. 2009. 361. P. 2436–2448.
E. S. Temnikova, Doctor of Medical Sciences, Professor
State Budgetary Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation, Omsk
Contact Information
Headache treatment
Headache with normal pressure also requires timely treatment. The regimen is prescribed individually, based on the results of a complete examination. It may include the following steps:
- painkillers - a first aid method for headaches, often used at home;
- antispasmodics - prescribed to relax blood vessels and relieve spasms;
- anti-inflammatory drugs in the form of tablets or injections - necessary for the treatment of diseases of the cervical spine;
- a set of measures to relieve intoxication: the use of antidotes (antidotes), drip infusion of electrolyte solutions;
- means to improve brain function;
- additional techniques: neck and head massage, therapeutic exercises.
At the Clinical Brain Institute, we prescribe only those drugs that are truly necessary to eliminate the cause or symptoms of headaches. The ability to conduct a full diagnosis allows you to select the most effective treatment methods. Doctors with many years of experience specialize in the treatment of diseases that manifest themselves as headaches and normal blood pressure.
Symptoms of intracranial pressure in adults
In many cases, a slight increase in ICP may not manifest itself for a long time. If the pressure rises sharply or high enough, the following symptoms may occur:
- headache - it can be pressing or bursting, usually occurs in the morning, this pain has no clear localization, it can be felt in different parts of the skull;
- nausea and vomiting - they usually occur at the peak of the headache;
- drowsiness, malaise, general poor health;
- memory impairment (forgetfulness), attention disorders, problems with thinking;
- changes in the autonomic nervous system – surges in blood pressure, slow pulse, increased sweating;
- visual impairment up to complete blindness.
Symptoms may come on suddenly or develop gradually over weeks or months.
Prevention methods
Headaches are often not associated with diseases, but appear as a result of a violation of the regime, poor nutrition, and a sedentary lifestyle. They are easy to prevent at home. To do this, it is enough to eat healthy foods rich in vitamins and microelements and avoid stress. It is also important to normalize your work and rest schedule, and spend time in the fresh air.
Doctors at the Clinical Institute of the Brain warn that if a headache does not go away at home even after following all the recommendations, you must contact them in a timely manner for a full examination and a treatment regimen.
Clinical Brain Institute Rating: 5/5 — 6 votes
Share article on social networks