Causes of severe headaches
An attack of sudden pain in the head can be associated with disorders of the cardiovascular system, endocrine glands, as well as various diseases of other organs. It is impossible to conduct a complete diagnosis at home, but it is important to pay attention to the characteristics of the headache. The location of its manifestation, strength and other characteristics may indicate the reason why it occurs.
- Severe, acute pain in the head is a consequence of traumatic brain injury, infectious diseases of the brain. They can also be a sign of migraine, hypertension and other diseases. If the pain continues to intensify, this indicates an increase in inflammatory or degenerative processes.
- Prolonged pain indicates dangerous chronic processes that require timely treatment. During diagnosis, a person may be diagnosed with infectious diseases of the brain, neoplasms, and parasite infestations. You should consult a doctor if attacks occur frequently and last more than a day.
- Throbbing pain is a typical symptom of hypertension or increased intracranial pressure. However, similar symptoms manifest themselves in migraine, eye and inner ear diseases. To understand the exact cause, a diagnosis must be carried out.
- Sudden, sharp pain accompanies vascular spasms. It can also occur due to mechanical compression of the nerve (with osteochondrosis and other diseases of the spine). However, a similar picture can develop with a stroke, so it is important to seek medical help in time.
Headache is not a separate disease, but a signal from the body about various disorders. A person needs to recognize it in time and begin treatment, depending on the cause. It is also important to understand the mechanisms of how pain occurs in order to select the most effective drugs against it.
Migraine
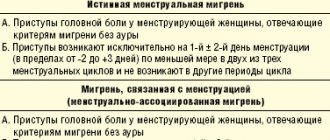
Migraine is a primary headache and one of the most common types. It often affects only one half of the head, but can also spread to the entire circumference of the head. It is believed that migraine attacks are associated with vascular or neurogenic disorders, and the triggers are environmental factors. A typical migraine occurs in several stages. Patients who have suffered from this disease for a long time can recognize the onset of an attack in the early stages and take anti-migraine medication in time.
- Prodromal phase - can begin several hours or days before an acute attack of headache. It is manifested by minor changes in well-being and mood swings. Disorders of the digestive tract and muscle spasms in the neck may also occur.
- Aura is a neurological symptom that develops in most patients. It begins immediately before a headache attack and lasts no more than an hour. Visual disturbances appear more often, which consist of a decrease in the ability to concentrate on various objects, the appearance of dark spots and circles in the field of vision. Sensory disturbances (tingling sensations, numbness of the skin), dizziness, speech impairment and memory loss are also possible. These symptoms are temporary and go away after the attack.
- The headache itself – in an adult, on average lasts from 4 hours to 3 days. For children it lasts no more than an hour. The pain can be unilateral or bilateral, often accompanied by soreness and discomfort in the neck. Patients also often complain of nausea, dizziness, and loss of coordination.
- Postdromal phase – develops after an intense headache. For some time after the attack (several days), disturbances such as fatigue, nausea, confusion, mood swings, and gastrointestinal disorders may remain.
Migraine is a chronic disease that can occur for the first time in both children and adults. Attacks occur with varying frequencies - from once every few years to several times a week. Headaches can be triggered by stress, extreme fatigue, and sudden changes in weather conditions. It is intense, and conventional painkillers are ineffective against it. The doctor will prescribe special medications against migraines, which must be taken at the first manifestations of the disease.
Read more in the material : Migraine with aura
Vascular disorders
Most cases of severe headaches are associated with changes in blood pressure (see Headache due to hypertension). Hypertension is a common disease that occurs in older people, as well as in various vascular pathologies. It can be triggered by atherosclerosis, a chronic disorder in which the walls of the arteries become saturated with cholesterol and certain fractions of lipoproteins. Their deposits narrow the lumen of blood vessels and can form plaques. Also, hypertension is often caused by decreased elasticity of the arteries, excess weight, and abnormal physical activity. It manifests itself in attacks during which the patient experiences the following symptoms:
- attack of severe headache;
- redness of the facial skin and visible mucous membranes;
- a feeling of pulsation in the head, which is especially noticeable in the back of the head and temples;
- increased heart rate;
- general weakness and dizziness;
- deterioration of hearing and vision, the appearance of visual, auditory, sensory hallucinations;
- disruption of the digestive tract.
Some patients are diagnosed with chronic hypotension. It is associated with a decrease in blood pressure. Attacks are manifested by a sharp, aching headache, impaired coordination of movements. A sudden drop in blood pressure may cause fainting. You can measure your blood pressure yourself using a tonometer. Its constant decrease is dangerous, since tissues experience hypoxia (oxygen starvation), which leads to disruption of their function.
Stroke
A stroke is an acute disorder of cerebral circulation. It can occur during prolonged ischemia or due to hemorrhage in the brain tissue. There are two main types of stroke. The first of them is ischemic, associated with insufficient blood supply to the brain. It can occur with prolonged hypotension or with narrowing of the lumen of important vessels. The second type is hemorrhagic, which is a cerebral hemorrhage. It can manifest itself in cases of traumatic brain injury or due to rupture of a vessel due to hypertension. The second type is more dangerous because it is more often fatal.
A stroke is manifested by a severe headache, nausea, and pallor of the mucous membranes. Fainting often occurs, but in some cases the person remains conscious. There is a diagram of how to identify the signs of a stroke in the early stages:
- ask the person to smile - the smile may be asymmetrical due to the inability to raise one of the corners of the mouth;
- raise both arms in front of you - one of them cannot be raised to the same height;
- repeat a simple sentence - during a stroke, diction is impaired, a person is unable to produce some words.
It is useful for every person to know the first signs of a stroke. The effectiveness of medical care decreases within a few hours. Even a mild attack can lead to irreversible changes in the structure of the brain, necrosis of its individual areas. Timely emergency care is the only way to restore cerebral circulation. This is followed by a long period of rehabilitation, the effectiveness of which depends on many factors: the severity of the attack, the age of the patient, and the presence of concomitant diseases.
Sinus pain
Colds can be complicated by inflammation of the paranasal sinuses. These formations are cavities in the skull filled with air. Inside, they are covered with a thin mucous membrane, on which viruses and bacteria develop during various infectious diseases. There are several types of sinusitis, which are manifested by a sharp headache:
- sinusitis - inflammation of the paranasal (maxillary) sinuses;
- frontal sinusitis - infection of the frontal sinus;
- ethmoiditis - inflammation of the sphenoid sinuses;
- sphenoiditis - inflammation of the mucous membrane of the ethmoid bone sinuses.
The most common type of sinusitis is sinusitis . It manifests itself in adults and children and often occurs in a chronic form. Characteristic signs of this disease are nasal congestion, fever, frequent headaches and general deterioration in health. Often these symptoms worsen in the cold and are practically not felt in a warm room. The simplest test for sinusitis can be done at home - sharply tilt your head forward and down. With sinusitis, this movement is accompanied by a sharp headache. To treat sinusitis, a course of antibiotics, nasal rinsing and symptomatic medications are prescribed. If these methods are not effective enough, it may be necessary to puncture the maxillary sinus to remove its contents and rinse the cavity with an antibacterial solution.
Read more: Sinus headaches
Infectious diseases
Influenza, acute respiratory viral infections and other viral respiratory diseases in the initial stages can manifest as a sharp pain in the head. They occur when an infection enters the mucous membranes of the mouth and nose, after which it causes acute inflammatory processes in the respiratory organs and nasopharynx. Viruses and bacteria are constantly in the external environment, and a person comes into contact with them, but infection occurs when the body’s immune defense is reduced. This is manifested by the following symptoms:
- headache, which may be the first of all symptoms;
- nasal congestion, runny nose;
- sore throat, inflammation of the mucous membrane of the nasopharynx;
- cough, pain when breathing.
A dangerous infectious disease that is accompanied by a severe headache is meningitis. It is manifested by inflammation of the membranes of the brain and poses a danger to the patient’s life. Its main cause is a viral and bacterial infection that penetrates the brain during various infectious diseases. Meningitis is manifested by acute headaches, nausea and vomiting, impaired coordination of movements, deterioration of hearing and vision, and fainting is also possible. Treatment takes place in a hospital setting, under the constant supervision of doctors.
Neuritis
Acute headaches can be caused by damage to the trigeminal nerve. This is the largest of the cranial nerves, which along its length is divided into 3 parts. Its mechanical damage or infectious inflammation causes acute, throbbing pain. It can appear in the forehead and temples, nose and upper jaw, or resemble a toothache. Headache with trigeminal neuritis is also accompanied by additional symptoms:
- spasms of the muscles of the face and head;
- increased body temperature;
- decreased sensitivity of facial skin;
- deterioration in the mobility of facial muscles.
At the first signs of neuritis of the facial nerve, it is necessary to begin treatment. The doctor will select a set of drugs that will affect both the cause and symptoms of inflammation. The general regimen includes antibiotics, anti-inflammatory and painkillers.
Other reasons
A sharp headache can also occur in a healthy person. Its causes include physical fatigue, stress, nervous tension, and disruption of sleep schedules. However, if it does not go away for a long time or appears too often, you should consult a doctor for a full examination. As a result, the following diseases are detected:
- injuries and their consequences - painful sensations can manifest themselves for a long time after a head injury;
- increased intracranial pressure;
- inner ear diseases;
- Cluster pain is a rare type that is characterized by very high intensity.
Regardless of the cause of the headache, it is dangerous to endure this condition. Your home medicine cabinet should contain painkillers that will relieve an attack. If pain is not relieved, brain cells experience constant hypoxia, which further increases the risk of stroke.
Dizziness in neuropediatrics
In neuropediatrics, many pathological conditions are accompanied by dizziness (at least a hundred of them) [1]. S. V. Morozova et al. (2002) indicate that dizziness is one of the most common symptoms encountered in medical practice (about 3–4% of the reasons for the total number of visits to doctors) [2].
Dizziness (vertigo) is a feeling of deviation or spinning of both one’s own body and surrounding objects. In the first case, we can talk about subjective (non-systemic) dizziness, and in the second about objective (systemic) [1].
In general, dizziness is a feeling of apparent rotation, displacement of surrounding objects or one’s own body, that is, manifested by signs of a violation of spatial orientation [1, 3, 4].
Etiological and pathogenetic factors
The main cause of dizziness is an imbalance of information coming from sensory stabilizing systems (vestibular, visual, somatosensory), leading to a violation of spatial orientation.
Dizziness occurs when there is inadequate conduction of a nerve impulse from the vestibular analyzer to the brain (especially to its cortex), when there is no coordination with one or another real movement. As a result of the inconsistency of this impulse with others emanating from the eyes and somatosensory system, a hallucinatory perception of one’s own and external movements arises.
Dizziness develops as a result of an imbalance of sensory information coming from the main afferent systems that provide spatial orientation (vestibular, visual, proprioceptive), but a significant role belongs to disturbances in the central processing of information and the efferent part of the motor act. Pathological changes in the musculoskeletal system are less significant.
Common causes of central vertigo are trauma, inflammation, demyelination and exogenous toxic lesions of the central nervous system (CNS), and CNS tumors. Central vertigo occurs when there is damage/dysfunction of the pons and/or cerebellum.
Peripheral vertigo occurs when there is damage/dysfunction of the labyrinth or VIII pair of cranial nerves. With peripheral dizziness, compensation occurs faster and more fully than with central dizziness.
Common causes of vertigo in children are diseases of the eustachian tube of the middle ear, but true vertigo can also be caused by labyrinthitis, perilymphatic fistula between the inner and middle ear (inner ear defect), trauma, mastoid or middle ear choleastomy, vestibular neuronitis, benign paroxysmal postural vertigo, Meniere's disease or diseases of the central nervous system [1, 3, 4].
A number of authors suggest considering panic attacks (induced by hyperventilation), cerebellar atrophy, vestibular neuronitis, etc. as causes of dizziness [1].
Approaches to classification
Physiological ones include dizziness that occurs, for example, when watching films with chase scenes, when looking at a moving train (or other type of transport), “sea sickness,” a feeling of motion sickness when ascending an airplane or high-speed elevator, when looking down from a height, etc. d.
Pathological dizziness occurs when the vestibular, visual and somatosensory systems are affected. It may appear with diplopia, incorrectly selected glasses or contact lenses, or impaired proprioceptive sensitivity.
It is generally accepted to divide dizziness into systemic and non-systemic. Systemic vertigo is characteristic of damage to the vestibular system, which consists of the organ of balance in the inner ear, the abducens nerve, the nuclei of the vestibular nerve in the medulla oblongata, associated with the nuclei of the vagus nerve, the red nucleus, the cerebellum, the nuclei of the oculomotor nerve, as well as with the cells of the anterior horns of the spinal cord. brain Systemic vertigo occurs in combination with other cochleovestibular disorders (nausea, vomiting, nystagmus, tinnitus) and often serves as a sign of damage to the vestibular analyzer at various levels (middle ear pathology, neuropathy of the vestibulocochlear nerve, segmental and suprasegmental disorders) [1, 3, 4].
Non-systemic dizziness is a disorder in the picture of a lipotimic state. The cause of syncope can be cardiogenic and vasodepressor disorders, hyperventilation, hypoglycemia, nocturia, orthostatic fainting, etc. With non-systemic dizziness, arterial hypotension and asthenia are often observed (after acute or exacerbation of chronic diseases). Unsystematic dizziness can occur with sudden turns of the head, in stuffy rooms.
Among the types of dizziness, the following are distinguished: 1) auditory (Meniere's disease); 2) gastric (a sign of stomach disease, Trousseau syndrome); 3) labyrinthine (endolymphatic hydrops, Meniere's disease); 4) visual (refractive errors, imbalance of the external muscles of the eye); 5) organic (with damage to the central nervous system); 6) postural (synonym: positional), which occurs when the body position changes, usually from a sitting or lying position [1, 3, 4].
The classification of the causes of dizziness proposed by GR Holt and JR Thomas (1980) includes 8 main groups of etiological factors: 1) inflammatory and non-inflammatory diseases of the middle/inner ear; 2) diseases of the central nervous system; 3) damage to the organs of the neck, including degenerative-dystrophic changes in the cervical spine; 4) metabolic and hematological disorders; 5) drug-induced disorders; 6) infectious lesions; 7) cardiogenic causes; other reasons. The latter includes no more than 10% of cases [1].
2) diseases of the central nervous system; 3) damage to the organs of the neck, including degenerative-dystrophic changes in the cervical spine; 4) metabolic and hematological disorders; 5) drug-induced disorders; 6) infectious lesions; 7) cardiogenic causes; other reasons. The latter includes no more than 10% of cases [1].
Additionally, dizziness is classified as constant and intermittent, paroxysmal and non-paroxysmal, positional (depending on the position of the body) and attitudinal (depending on the movement of the head) [1].
Clinical manifestations
Symptoms depend on the characteristics of certain types of neurological or somatic pathology; they are quite variable. Thus, older children may describe sensations of rotation and spinning, while younger children are more likely to demonstrate imbalance when falling, in the form of stumbling or clumsiness of movement.
Central vertigo often manifests itself in single attacks of varying duration; possible dysarthria, diplopia, numbness, weakness, and less commonly, pronounced nystagmus.
Peripheral dizziness is usually accompanied by nausea and vomiting; when the ear is affected, they are accompanied by decreased hearing, a feeling of fullness and noise in the ear, and otalgia. Attacks can be isolated or recurrent.
When the vestibular system is damaged, there is uncertainty when walking, frequent falls, fear and avoidance of sudden and rapid movements. Unsteadiness of gait, uncertainty when walking and a feeling of intoxication are not always symptoms of disorders of the vestibular system. These symptoms may indicate severe diffuse brain damage [1, 3–5].
Based on children’s descriptions of the sensations of dizziness, M. Hertl (1990) systematized them (scale of sensations of dizziness): 1) rotational dizziness - a feeling of apparent rotation of surrounding objects and one’s own body in the direction opposite to each other; 2) oscillatory dizziness - the patient feels as if the floor is shaking under him; 3) the feeling of an “elevator” - the impression of falling into an elevator shaft; 4) lateropulsion - a feeling of falling to the side [5].
Lesions of the central nervous system of inflammatory origin
Inflammatory lesions of the central nervous system are often accompanied by dizziness. With encephalitis, ventriculitis, hydrocephalus, there is a feeling of swaying, instability, sometimes with disturbances in spatial perception - the size, shape of objects or one's own body (Alice in Wonderland syndrome).
The causes of systemic peripheral vestibular disorders in children are bacterial lesions of the inner ear, viral neurolabyrinthitis, endolymph circulation disorders, traumatic injuries, Meniere's disease and Meniere-like syndromes.
Bacterial, viral or infectious-toxic damage to the labyrinth can be a complication of acute or chronic otitis (tympanogenic labyrinthitis), purulent meningitis (meningogenic labyrinthitis), influenza, mumps, or a manifestation of hematogenous metastasis during sepsis (hematogenous labyrinthitis). The progression of otitis media with the spread of the inflammatory process to the inner ear is often accompanied by vestibular disorders, uncontrollable vomiting, a sensation of rotation and rocking, and nystagmus. Purulent labyrinthitis can lead to irreversible problems with balance and hearing. Serous labyrinthitis, which develops as a result of toxic irritation of the neuroepithelium, is more prognostically favorable.
With a herpetic lesion, general signs of a viral disease are observed, vesicular rashes on the auricle, in the ear canal and even on the eardrum, sometimes on the anterior two-thirds of the same half of the tongue. In such cases, unilateral deafness or hearing loss, rotational vertigo with nystagmus, vomiting, severe pain, unilateral paresis of facial muscles due to true trigeminal neuralgia and facial nerve paralysis develop [1, 3–5].
Endolymph circulation disorders
Endolymph circulation disorders are manifested by attacks of systemic dizziness, nausea, vomiting without changes in hearing. These patients always have a positive Barany test. A common cause of changes in endolymph circulation in the inner ear is the entry of cold air or water into the middle ear cavity due to perforation of the eardrum of traumatic or inflammatory origin. Swimming and diving are dangerous for these children unless the external auditory canal is sealed tightly (for example, with cotton wool soaked in grease). Another cause may be canal cupulolithiasis; in these cases, canal tamponade relieves dizziness and nystagmus [1].
Exogenous toxic damage to the labyrinth
Aminoglycoside antibiotics (amikacin, gentamicin, tobramycin, etc.), antitumor and anthelmintic drugs, as well as salicylic acid preparations, quinine, etc., have significant ototoxicity. In neurological practice, benzodiazepines, anticonvulsants (carbamazepine, phenobarbital, phenytoin), neuroleptics (haloperidol) are widely used. , phenothiazines), which, acting on the central parts of the locomotor system, can cause dizziness. Toxic damage to the labyrinth is caused by botulinum toxin, some mushrooms and poisonous snake bites [1, 3, 4].
Movement sickness
It occurs especially often in children aged 2–12 years (10% of boys and 30% of girls). Clinical symptoms are variable: mild (lethargy, drowsiness, stomach discomfort, pallor or flushing of the face, hypersalivation with increased sweating, moderate increase in blood pressure), moderate (shortness of breath, nausea, vomiting, flatulence, perversion of taste, chills or feeling of heat, headache in the forehead, anxiety, tinnitus), severe (heart rhythm disturbances, spatial disorientation, fainting) [1, 3, 4].
Meniere's disease
A triad of symptoms is characteristic: 1) systemic dizziness (“rotational”); 2) ringing in the ears; 3) various hearing impairments. The duration of attacks averages 2–5 hours (from 10 minutes to 48 hours). Patients often experience a feeling of pressure in the ears. Meniere's disease is paroxysmal in nature and occurs against the background of complete well-being. This disease is observed mainly in older children. In addition to the described triad of symptoms, autonomic disorders, nausea, vomiting, nystagmus, and a feeling of “fullness” in the ears may be observed [1, 3, 4].
In practice, Meniere-like syndromes caused by vascular dyscirculation in autonomic dysfunction and vertebrobasilar insufficiency in osteochondrosis of the cervical spine are more common.
Vertebro-basilar insufficiency
Discirculatory disorders occur in the presence of deformations/anomalies of the vertebral arteries. Characterized by imbalances that increase when the head is turned. There are subjective vestibular manifestations, visual and oculomotor disorders, static and coordination disorders [1, 3–5].
Migraine
Atypical migraine attacks with dizziness are more common in children than in adults. Dizziness may precede a migraine or persist after the end of a cephalgic attack. In some cases, repeated paroxysmal dizziness can transform into typical migraine attacks over time.
With basilar artery migraine syndrome, in addition to dizziness, ataxia, tinnitus, dysarthria, and diplopia are noted (they precede an attack of headache). The first attack of the disease can occur at any age (from infancy to adolescence), and its duration can be up to several hours [1, 3–5].
Traumatic injuries of the vestibular apparatus
Dislocation of the stapes occurs when exposed to sharp objects, unsuccessful removal of a foreign body, or paracentesis. In these cases, dizziness suddenly appears so severe that the child may fall. With traumatic brain injuries with a fracture of the temporal bone pyramid, concussion of the labyrinth, dizziness with hearing loss is often observed.
Central vestibular vertigo is observed with fractures of the base of the skull passing through the pyramid of the temporal bone, accompanied by damage to the membranous semicircular canals and hemorrhage into the labyrinth. A concussion or contusion of the brain may be accompanied by damage to the ear labyrinth. In these cases, dizziness is transient and is triggered by head movement. Usually it persists for a long time (several months or years) [1, 3–5].
Multiple sclerosis (MS)
Of the demyelinating diseases, dizziness of the “Meniere-like” type most often occurs in MS with damage to the pons. Dizziness and a feeling of uncertainty when walking may appear as the initial manifestations of the disease. The diagnosis of MS is established on the basis of clinical, laboratory and instrumental signs [1, 3, 4].
Neurogenetic conditions
Malformations of the central nervous system such as cerebellar agenesis and atrophy, Arnold-Chiari syndrome, in addition to ataxia, are often accompanied by dizziness. Hereditary Friedreich's spinocerebellar ataxia causes dizziness with frequent falls [1, 3–5].
Brain tumors
The sudden onset of attacks of dizziness, headaches with vomiting, bradycardia, and convulsions may be symptoms of a brain tumor. Tumors of the cerebellopontine angle are more often found, usually neurofibromas (neurinomas) in Recklinghausen neurofibromatosis. Considerably less common with the described symptoms are tumors of the fourth ventricle and neoplasms of other localizations [1, 3–5].
Syringobulbia
Syringobulbia is a pathology in which tubular cavity formation (cavitation) of the spinal cord is noted when the cystic lesion spreads to the medulla and pons. In childhood, syringobulbia is sometimes associated with Arnold-Chiari malformation types I and II [1, 3, 4].
Benign paroxysmal vertigo
Benign paroxysmal vertigo usually occurs in children aged 12–36 months. The attacks occur suddenly and are characterized by ataxia, causing falls and refusal to walk or sit. Throughout the attack, the child may experience horizontal or rotational nystagmus. More often, dizziness occurs in the morning, and intensifies when moving to a horizontal position from a sitting position, as well as when turning in bed [1, 3–5].
Epilepsy
Unsystematic dizziness is often observed in children suffering from this disease. The aura before a grand mal (generalized) epileptic seizure may be accompanied by severe dizziness. Absence seizures with short-term loss of tone and short-term psychomotor seizures can give the impression of dizziness. With temporal lobe epilepsy, short-term attacks of non-systemic dizziness may occur, accompanied by unaccountable fear, phenomena of depersonalization and derealization [1, 3–5].
Diagnostics
First of all, you should try to clarify whether we are talking about single (episodic) or recurrent dizziness, as well as what its origin is (central or peripheral).
Systemic dizziness is observed with damage to the peripheral and central vestibular structures. The peripheral structures of the vestibular apparatus include the semicircular canaliculi, ampullae of the vestibule, and the vestibular portion of the vestibular-cochlear nerve. With peripheral damage to the vestibular apparatus, dizziness is accompanied by horizontal nystagmus, which in most cases is suppressed by gaze fixation. The central vestibular structures are represented by the nuclei of the vestibular nerve in the medulla oblongata, the cerebellum, and the red nucleus. When the central vestibular apparatus is damaged, dizziness is accompanied predominantly by nystagmus with a rotational or vertical component and is not suppressed by gaze fixation.
Non-systemic dizziness is diagnosed when imbalances develop secondary, due to any extra-vestibular diseases. In such cases, children complain of darkening of the eyes, blurriness of surrounding objects, tinnitus, “numbness,” and headache. They often develop a concomitant collaptoid state [1, 3–5].
Physical examination
Damage to the vestibular apparatus in infants and young children can be suspected in the presence of symptoms such as nausea and vomiting that occur during feeding, swaddling, as well as any change in the child’s position. Persistent vomiting often leads to exicosis and acetonemia. Among the clinical symptoms upon examination, spontaneous nystagmus attracts attention; children often fix their heads in an inclined position, usually in the direction where labyrinthitis has developed [1, 3, 4].
Anamnesis
When collecting anamnesis, they find out: 1) whether dizziness is accompanied by rotation, the presence of a feeling of falling and whether there is a certain direction of falling; 2) the connection between dizziness and changes in posture and physical stress; 3) duration of the dizziness attack; 4) the presence of accompanying signs indicating involvement of the ENT organs (ear) or brain in the pathological process; 5) whether dizziness is accompanied by hearing loss or ringing in the ears; 6) presence/absence of paralysis (present in transient ischemic attacks); 7) taking medications by the patient [1, 3, 4].
Coordination samples
Always checked during routine assessment of neurological status and include index finger-nose and knee-heel tests, indicating intact or impaired coordination of movements.
Using the Romberg test, the degree of imbalance in space is assessed.
Barany test: when the head is sharply turned backwards and towards the affected labyrinth, nystagmus occurs in the same direction. The described test is positive for cupulolithiasis (Barany syndrome).
Babinski-Weil test (“star” test): if, while walking with eyes closed, the patient periodically turns 180°, then due to his deviation when walking to the side, the traces of his feet form a figure resembling a star. The test indicates damage to the cerebellum, and the side of the deviation allows you to determine the side of the affected hemisphere.
An auxiliary diagnostic test is the Unterberger marching test (40 steps in place with eyes closed).
The Dix-Hallpike test confirms the presence of benign paroxysmal positional vertigo: the patient is quickly transferred from a sitting position to a lying position so that his head hangs over the edge of the couch (while turning his head to the right or left). The test is considered positive if dizziness in combination with rotational nystagmus is noted within 30 seconds after the described maneuver [1, 5].
Instrumental research methods
When studying the state of cerebral hemodynamics, transcranial Dopplerography and/or dynamic angioscintigraphy can provide additional information about cerebral blood flow and clarify the location, nature and severity of existing damage to the nervous system.
Neuroimaging methods, such as computed tomography and magnetic resonance imaging of the brain, allow not only to identify the location and level of damage to the central nervous system, but also to determine the presence and extent of damage to the middle and inner ear.
An electroencephalographic (EEG) study is necessary primarily to identify the epileptic genesis of paroxysms accompanied by dizziness [1].
ENT examination
It is necessary to exclude inflammatory, toxic and traumatic lesions of the middle and inner ear, labyrinthitis, neoplasms in the ear canal, etc. Sometimes there is a need to conduct a specialized otoneurological study (using special methods), for example, with Meniere’s disease [1, 3, 4].
Treatment approaches
Non-drug
Treatment by position (giving a certain posture) is used for postural dizziness, since in this case there is no need to prescribe medications. For dizziness due to pathology of the cervical spine, numerous methods of physiotherapy are used, including acupuncture, as well as physical therapy, etc. [1].
Medication
Anticholinergic blockers, vasodilators, antipsychotics, calcium ion antagonists, antihistamines and sedatives are used in the treatment of dizziness. Many of them have significant side effects. Below are drugs that are relatively safe and effective to use for dizziness in children.
Piracetam is widely used as a starting agent for the treatment of dizziness, mainly of vascular origin. Vinpocetine has indications for use such as dizziness associated with dyscirculatory or post-traumatic encephalopathy, as well as Meniere's disease and dizziness of labyrinthine origin. Hydroxyzine is prescribed for dizziness accompanying anxiety disorders and neurotic disorders.
For dizziness due to panic attacks, tricyclic antidepressants, clonazepam, and selective serotonin reuptake inhibitors are used, taking into account the age of the patients [1, 3, 4].
Children with serial benign paroxysmal vertigo respond well to dimenhydrinate [1].
Betahistine occupies a separate place in the treatment of dizziness. The drug has a histamine-like effect and has an effect primarily on the H1 and H3 receptors of the inner ear and vestibular nuclei of the central nervous system. It increases regional blood flow in the arteries of the inner ear and blocks synaptic transmission in the vestibular nuclei. M. A. Lobov et al. (1998) used betahistine in the treatment of dizziness of various origins in children (Meniere's disease, cochlear neuropathy, vertebrobasilar insufficiency, syringobulbia, etc.) in combination with routine medications (31 patients) and as monotherapy (11 children), achieving a positive effect in 40 cases (in 30 children the effect was satisfactory and good, in 10 patients the dizziness completely regressed) [6].
Nootropic drugs are widely used in the Russian Federation for the treatment of syndromes accompanied by dizziness of various origins.
Literature
- Studenikin V.M., Shelkovsky V.I., Bykova O.V., Vysotskaya L.M. Dizziness in childhood // Pediatrician’s Handbook. 2006; No. 11: 18–29.
- Morozova S.V., Zaitseva O.V., Naletova N.A. Dizziness as a medical and social problem // RMJ. 2002; 10 (16): 725–729.
- Nelson textbook of pediatrics. Kliegman RM, Stanton BF, St Geme III JW et al, eds. 20 th ed. Philadelphia. Elsevier, 2016. 3474.
- Menkes JH, Sarnat HB, Maria BL (eds.) 7th ed. Lippincott Williams & Wilkins. Philadelphia-Baltimore, 2006. 1286.
- Hertl M. Differential diagnosis in pediatrics. In 2 vols. Per. with him. M.: Medicine. 1990. T. 1. 255–258.
- Lobov M. A., Yakushin M. A., Borisova M. N., Misikov V. K. Betaserc: correction of dizziness in neurological diseases // Bulletin of Practical Neurology. 1998; No. 4: 198–199.
V. M. Studenikin, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Economics
LLC NPSMC "Dream Clinic", Moscow
Contact Information
Dizziness in neuropediatrics / V. M. Studenikin For citation: Attending physician No. 10/2018; Page numbers in issue: 52-55 Tags: spatial orientation, central nervous system, middle ear
Diagnostic methods
To choose an effective headache treatment regimen, it is important to undergo a full examination and determine its cause. To do this, a set of tests is prescribed to assess the condition of the heart and blood vessels, brain and other organs. It may include the following techniques:
- General and clinical blood tests - allow you to identify inflammatory processes, acute and chronic diseases of internal organs;
- electroencephalography is a method for diagnosing the brain, thanks to which it is possible to detect signs of tumors and vascular pathologies;
- MRI is an informative technique for assessing the patient’s condition in case of stroke, sinusitis, trauma and other pathologies;
- Ultrasound of the vessels of the neck and head using a contrast agent (Dopplerography) - allows you to determine atherosclerosis and other vascular diseases.
The Clinical Institute of the Brain has all the conditions for accurate and comfortable diagnosis. Doctors have extensive experience in treating diseases that are accompanied by severe headaches. They will prescribe only the necessary examinations to quickly determine the cause of the pain and prescribe an effective treatment regimen.
Classification
In modern clinical practice, the classification developed by the classification committee of the International Headache Society is used. In accordance with it, headaches are divided into primary, secondary and neuralgia.
Primary pain
The main pain of this type is migraine. It is not associated with any pathologies of internal organs, systemic diseases or injuries. Primary headaches also include:
- tension is the most common type of pain,
- after physical stress, sex, emotional stress,
- during long flights, climate change, sudden changes in weather,
- cluster.
The cause of primary pain is the chemical activity of brain cells and blood vessels and the increased sensitivity of pain receptors.
Secondary pain
Secondary pain is always associated with an existing disease. They may be a symptom:
- osteochondrosis,
- colds or viral diseases,
- hypertension,
- brain tumors,
- traumatic brain injuries and many other pathologies.
Neuralgia
Neuralgia is a condition caused by damage to the peripheral nerves. Severe headaches occur with inflammation of the trigeminal, glossopharyngeal, and occipital nerves. Neuralgia can be of a different nature and vary in intensity, appear suddenly or gradually increase.
Inflammation of the nerves can occur due to stress, hypothermia, problems with the immune system, or prolonged fasting.
Headache treatment
To treat a headache, it is important to determine its cause. At home, you can take a pain reliever and massage your neck and head. However, the doctor prescribes the full regimen based on test results. It may include the following techniques:
- drug treatment (antibiotic therapy for infectious processes, muscle relaxants, anti-inflammatory drugs, drugs to improve blood supply to the brain);
- physiotherapy – a set of techniques based on the effects of ultrasound, heat, electric or magnetic field;
- physical therapy – prescribed for neck diseases that are accompanied by headaches.
Doctors at the Clinical Institute of the Brain recommend not to self-medicate. Modern techniques allow you to quickly and safely get rid of headaches, eliminate its causes and prevent further development of diseases. The doctor will prescribe an effective regimen, but the results of treatment largely depend on following all instructions at home.
Prevention methods
Sharp pain in the head is a symptom of a number of disorders, which are often acquired. This means that they are easy to prevent if you follow the recommendations of doctors:
- give up bad habits - they form toxins that adversely affect brain cells;
- exclude from the diet fatty foods, sweets, salt and spices in large quantities, fast food;
- carry out moderate physical activity - it is important to maintain muscle tone to prevent diseases of the cervical spine;
- normalize your sleep schedule.
The Clinical Brain Institute specializes in the diagnosis and treatment of diseases that manifest as severe headaches. Our center has modern equipment for conducting complex examinations, and our doctors have extensive experience in treating head pain. For most patients, it is enough to follow the recommendations at home, but the center offers the possibility of comfortable placement in a hospital.
Clinical Brain Institute Rating: 3/5 — 1 votes
Share article on social networks