Tension headaches are typically diffuse, mild to moderate in intensity, and are often described as feeling like a “tight band” around the head. Tension headache (TTH) is the most common type of headache, yet the causes of this type of headache are still not well understood.
Treatment for tension headaches is quite effective. Management of tension-type headaches is often a balance between a healthy lifestyle, the use of non-drug treatments, and adequate drug treatment.
Symptoms
Symptoms of tension headaches include:
- Dull, aching headache
- A feeling of “tightness” or pressure in the forehead or sides of the head and at the back of the head
- Soreness of the scalp, neck and shoulder muscles
Tension headaches fall into two main categories - episodic and chronic.
Episodic tension headaches
Episodic tension headaches can last from 30 minutes to a week. Episodic tension headaches occur on fewer than 15 days per month for at least three months. Frequent episodic tension headaches can become chronic.
Chronic tension headaches
This type of tension headache lasts several hours and may be continuous. If headaches occur 15 or more days per month for at least three months, they are considered chronic.
Tension headaches and migraines
Tension headaches can sometimes be difficult to distinguish from migraines. Additionally, if a patient has frequent episodic tension-type headaches, they may also have migraines.
Unlike some forms of migraine, tension headaches are usually not accompanied by blurred vision, nausea, or vomiting. And if during migraines physical activity increases the intensity of the headache, then during headaches stress loads do not have such an effect. Increased sensitivity to any light or sound can sometimes occur with tension headaches, but these symptoms are uncommon.
Stress will split your head!
When someone complains that stress gives them a headache, it's not always an excuse! Tension headaches (TTH) are a common type of headache that can easily be caused by negative emotions. Oleg Glazunov, a psychologist and psychotherapist, a member of the Association of Cognitive Behavioral Therapy, explained to Laba how stress can split your head.
Are you saying that stress causes headaches? Always?
Not always. There are many causes of headaches. But there is one of the most common types of primary headache (that is, when it is not a symptom of another disease), which is associated with stress. This is a tension headache.
Another type of primary headache, migraine, is not dependent on stress, according to the latest data. In addition, migraines occur more often than tension headaches. Read about this in our detailed guide .
So how does stress cause pain?
To explain it quite simply, stress causes certain negative emotions, which in turn activate a number of physiological reactions in the body. Tension headache (TTH) is one such reaction.
By the way, it could be even worse. A negative emotion causes a headache, and this, in turn, also becomes stress for the body and again “restarts” the same chain: stress – emotion – increased tension.
Stress translated from English means “load, tension.” From a physiological point of view, this is the body’s response to some external or internal influence. The response, in turn, is a set of normal physiological reactions and actions of the body to adapt to these influences. If stress does not exceed a certain level, it is beneficial for the body and is called eustress. When stress is too strong, it begins to harm the body. Then it is called distress. Distress is what causes tension headaches.
So the main thing is the emotions we experience?
Yes, emotions play a leading role in the development of tension headaches. Moreover, the strength and duration of emotions is determined not by the strength of external or internal influence, but by how a person evaluates this situation.
So it is more correct to describe the process in this way: a certain event occurs - a person evaluates it and perceives it as distress - a person perceives negative emotions - a physiological reaction, in particular, tension-type headache. In the worst case, this mechanism loops: tension from negative emotions – assessment of pain as distress – new negative emotions – worsening headaches.
According to cognitive behavioral theory, the thinking process is almost simultaneously accompanied by physiological reactions in the body.
Unlike animals, which, by the way, also sometimes suffer from “stress” headaches, in humans the leading role in the occurrence of emotions is played by the so-called second signaling system.
The animal's brain functions in the first signaling system. It responds to direct visual, auditory, tactile and other influences. And in the course of evolution, man, in addition to these reactions, developed another system. This is speech. A person uses it as a tool for managing and monitoring the physiological processes of his body. The second signaling system operates equally and in parallel with the autonomic and nervous systems.
Sometimes in a person these two methods of controlling physiology come into conflict. This is signaled by so-called psychosomatic diseases. Nervous tension tension is one of them.
Isn't it easier to just take a painkiller?
Taking a pill, of course, is easier than sorting out your emotions. But in this way you ignore the essence of the problem.
In the 1930s, two American physiologists, Walter Cannon and Philip Bard, formulated a theory of emotions . According to it, excitation comes to the thalamus and there it is divided into two streams. One goes to the cerebral cortex, where it is encoded through language and causes a “subjective” experience. And the second goes to the hypothalamus, which controls physiological reactions in the body.
Russian physiologist Peter Anokhin developed this theory and explained how the first and second signaling systems are integrated in human behavior. Subsequently, this model was confirmed by many experiments .
According to Anokhin, a person’s emotional state prevails over the physiological one. When we experience strong emotions, there is an almost instantaneous unification of all the functions of our body into a single whole.
Emotions are a signal from our brain, which constantly evaluates the benefits or harm of internal or external influences. Harmful effects may include headaches.
The problem is this. Physiological manifestations are treated by doctors who are focused on the use of medications. Both here in Russia and abroad, people most often go to doctors for treatment of HDN, and they assign the leading role in treatment to pills. And the pills simply help get rid of the symptom. As a result, negative emotions may find another physical channel to make themselves known.
What to do with emotions and stress so as not to give yourself a headache?
You can learn to manage emotions and the level of stress assessment. First of all, cognitive behavioral therapy as a model of psychotherapy offers analysis and work with the client’s thinking and behavior. Progressive muscle relaxation according to Jacobson , techniques for working with imagination and self-hypnosis are also used.
A psychotherapist can teach a person to identify and change irrational negative patterns of thinking. As a result, he can control negative emotions and not allow them to manifest themselves as headaches.
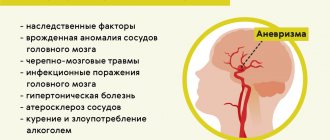
Causes
The causes of tension headaches are not known. Medical experts believed that tension headaches occur due to problems in the muscles of the face, neck and scalp, which in turn are caused by strong emotions, excess exertion or stress. But research shows that muscle spasm is not the cause of this type of headache.
The most common theories hold that there is an increased sensitivity to pain in people who have tension headaches and perhaps have an increased sensitivity to stress. Increased muscle soreness, a common symptom of tension headaches, may be a result of increased overall pain sensitivity.
Triggers
Stress is the most common trigger that causes tension headaches.
Risk factors
Risk factors for tension headaches include:
- Gender. Women are more likely to get this type of headache. One study found that nearly 90 percent of women and 70 percent of men experience tension headaches during their lifetime.
- Average age of the patient. The incidence of tension-type headaches peaks around age 40, although these headaches can develop at any age.
Complications
Due to the fact that headaches can be quite common, they can significantly affect work productivity and overall quality of life, especially if they become chronic. Frequent pain can disrupt your usual lifestyle and overall performance.
Classification
In the International Classification of Diseases, 10th revision, headache is coded under R51 and refers to typical disorders of the nervous system.
It is customary to distinguish two main variants of cephalgia, according to the etiological principle:
- Primary headache. This type of headache includes tension headache or tension headache, as well as migraine.
- Secondary headache. It does not arise independently, i.e. is formed under the influence of any pathological process occurring in the nervous tissue. For example, a secondary headache may occur as a result of oncological damage to the central nervous system or due to atherosclerotic damage to the cerebral vessels.
In addition to the etiological classification, there is also a pathogenetic classification of cephalgia, which includes types such as:
- Vascular headache. Vascular pain occurs as a result of spasm of the smooth muscles of the vascular walls, which leads to an increase in blood pressure in the cerebral basin and ischemia of brain tissue. In the opposite case, headache can also occur due to dilatation of the vascular bed or as a result of a violation of the rheological properties of the blood, which also leads to tissue hypoxia and ischemic damage.
- Muscle tension pain. In this case, overstimulation of the neuromuscular synapses occurs, which leads to excessive muscle tension and spasticity.
- Liquorodynamic pain. This type occurs as a result of changes in intracranial pressure, regardless of whether an increase or decrease in intracranial pressure occurred. Changes in pressure in the ventricles of the brain can lead to dislocation of brain structures, which ultimately creates pain.
- Neuralgic cephalgia. It is formed as a result of irritation of peripheral nerve fibers as a result of an extraneural or endoneurial pathological process. In this case, the mechanism of cephalgia is associated with the formation of a focus of pathological activity in the nociceptive system of the brain.
- Psychogenic. With this type, there are no pathological changes in tissues anatomically close to the nervous tissue. In this case, a malfunction occurs in the antinociceptive system of the brain, which leads to various disorders in the neurotransmitter dopaminergic system of the brain and the occurrence of pain. The main mechanism is disruption of the production of endogenous opiates.
- Mixed genesis. It occurs under the influence of the combined influence of the pathological process on the tissues surrounding the brain. The pathological effect can be either simultaneous or sequential.
Types of HDN
First of all, it is worth identifying the subspecies.
- Episodic pain occurs no more often than about 18 times a month, and a single attack lasts no more than half an hour. The severity of pain is usually low.
- Another type, chronic tension headache, is noticeably high in intensity. Patients have attacks more than 20 times a month, or more than 180 cases per year. Often this type of pain is accompanied by the appearance of depression.
Diagnostics
The diagnosis of tension-type headache is primarily based on medical history and symptoms and neurological examination.
The doctor may be interested in answers to the following questions:
- When did the symptoms begin?
- Has the patient noticed any triggers, such as stress or hunger?
- Were the symptoms continuous or episodic?
- How severe are the symptoms?
- How often do headaches occur?
- How long did you last have a headache?
- What does the patient believe reduces symptoms and what increases symptoms?
In addition, the doctor is also interested in the following details:
- Characteristics of pain. Is the pain throbbing? Is the pain dull, constant or sharp?
- Pain intensity. A good indicator of headache severity is the amount of time a patient can work during a headache attack. Can the patient work? Are there any episodes where the headache led to awakening from sleep or sleep disturbance?
- Localization of pain. Does the patient feel pain throughout the entire head, only on one side of the head, or just in the forehead or eye sockets?
Instrumental examination methods
If a patient has unusual or intense headaches, the doctor may order additional testing to rule out more serious causes of the headaches.
The two most commonly used diagnostic methods are CT (computed tomography) and MRI, which allow visualization of organs and tissues and detection of morphological changes.
1.General information
During the period of its active research, muscle tension headache has received many unofficial and semi-official synonyms - ranging from the laconic “simple headache” to the apt definition of “neurotic helmet”. Currently, in the international medical community it is recommended to call it a tension-type headache - which in translation is equivalent to the same original term “tension headache” (TTH), which we will use below.
TTH is widespread and, like any common pathology, in the statistical aspect it is assessed differently by different sources. Wikipedia, in particular, states that epidemiological indicators of HDN are about 20% of the general population. However, special sources often publish much more pessimistic data, according to which from 30% to 70% of people have experienced this type of headache, at least occasionally or sporadically. There is more or less consensus that tension headaches account for up to 80% of all types of headaches in general. The typical age range for manifestation is 20-40 years. In women, tension pain occurs one and a half to two times more often.
Thus, the problem of tension headaches is acutely relevant for neurology and, in addition, has a distinct social resonance: socio-psychological factors are included in almost all published etiopathogenetic lists and, on the other hand, tension headaches sharply reduce the quality of life of patients, negatively affecting performance , productivity, family and microsocial psychological climate.
A must read! Help with treatment and hospitalization!
Treatment
Some patients with tension headaches do not see a doctor and try to treat the pain on their own. Unfortunately, repeated self-use of painkillers can itself cause severe headaches.
Drug treatment
There are a wide variety of medications, including over-the-counter ones, that can help relieve pain, including:
- Painkillers. Simple over-the-counter pain relievers are usually the first line of treatment for headaches. These include aspirin, ibuprofen (Advil, Motrin IB, others), and naproxen (Aleve). Prescription medications include naproxen (Naprosyn), indomethacin (Indocin), and ketorolac (ketorolac tromethamine).
- Combined drugs. Aspirin or acetaminophen or both, often combined with caffeine or a sedative in one medicine. Combination medications may be more effective than medications with a single active ingredient.
- Triptans and drugs. For people who have both migraines and tension-type headaches, triptans can provide effective headache relief. Opiates, or narcotics, are rarely used due to their side effects and high risk of addiction.
How is tension headache treated?
The main recommendation for the treatment of tension headaches, as in general for any other disease, is to avoid self-medication and consult a doctor (neurologist).
It must be emphasized that tension headache is a disease that is based on various factors, and often their combination, and taking into account the individual characteristics of each individual, its treatment is also individual.
The influence of the family environment and other psychosocial factors must be analyzed individually for each patient and, if possible, included in the psychotherapeutic program.
Prophylactic drugs
Other medications may be prescribed to reduce the frequency and severity of attacks, especially if the patient has frequent or chronic headaches that are not relieved by pain medications.
Preventive medications may include:
- Tricyclic antidepressants. Tricyclic antidepressants, including amitriptyline and nortriptyline (Pamelor), are the most commonly used medications to prevent the development of tension headaches. Side effects of these drugs may include weight gain, drowsiness, and dry mouth.
- Other antidepressants. There is evidence that antidepressants such as venlafaxine (Effexor XR) and mirtazapine (Remeron) are effective in patients who are not depressed.
- Anticonvulsants and muscle relaxants. Other medications that may prevent tension headaches from developing include anticonvulsants such as topiramate (Topamax) and muscle relaxants.
Lifestyle adjustments and home remedies
Rest, ice packs, or long, hot showers can often reduce the intensity of headaches.
Non-drug treatment
- Acupuncture. Acupuncture may provide temporary relief from chronic tension headaches.
- Massage. Massage can help reduce stress and relieve tension. It is especially effective for relieving muscle spasms in the back of the head, neck and shoulders.
- Deep breathing, biofeedback and behavioral therapy. A variety of relaxation treatments are very helpful in treating tension headaches, including deep breathing and biofeedback.
2. Reasons
TTH received its name due to a direct etiopathogenetic connection with prolonged spasm (i.e. persistent involuntary tension) of the muscle groups of the face, neck, shoulder girdle and skull. This tension leads to compression of small blood vessels, vasculatory (blood supply) disturbances and hypoxia of the corresponding tissues; As lactic acid and other “fatigue metabolites” accumulate in them, excitation arises and intensifies in the nerve endings of spasmodic muscles, which is interpreted by the brain as a headache.
Trigger, provoking and risk factors include:
- anxiety-depressive reactions to psychosocial distress;
- larvated (syn. masked, latent, atypical, erased, hidden) depression of any origin;
- professional activities that involve staying in one position for a long time (driving a car, working at a computer, fine assembly installation, etc.);
- long-term uncontrolled use of certain medications (analgesics, tranquilizers, etc.);
- chronic fatigue, forced disturbances of the circadian cycle (alternating sleep and wakefulness);
- weather factors (heat, frost, strong wind);
- malnutrition, deficiency of iron compounds;
- alcohol, active and passive tobacco smoking;
- incorrect posture;
- unknown causes (in this case they speak of idiopathic tension-type headache).
Visit our Neurology page