Elbow joint
is a unique connection of three bones: humerus, radius and ulna. This is a complex combined joint, which includes three simple joints: humeroulnar, brachioradialis, proximal radioulnar. All of them are united by one common capsule and articular capsule (cavity). Inside the joint capsule, synovial fluid is constantly produced, which serves as a lubricant for the rubbing articular surfaces and nutrition for the anatomical parts. The ends of the bones are covered by a layer of periosteum, which helps protect and renew bone tissue, and also facilitates the supply of nutrients from the synovial fluid. All articular surfaces are covered with articular cartilage. The elbow joint is securely strengthened by ligaments and protected by a good muscular frame. These features allow you to perform four types of movements: extension and flexion, supination (rotation of the forearm in the elbow joint, in which it is possible to turn the hand with the palm up) and pronation (rotation of the forearm in the elbow joint, in which it is possible to turn the hand with the palm down). It is worth noting that the top end of the ulna has an olecranon process, shaped like a hook. The triceps brachii muscle is attached to it. A fracture of this process is a fairly common injury.
Types of damage
The following categories of diseases are characteristic of the elbow joint:
- Traumatic
Bruises. The most common injuries are to the olecranon, periarticular tissues, humeral condyles and ulnar nerve. - Ligament sprains
- Dislocations. There are: isolated dislocation and pronation subluxation of the radial head; dislocations of the forearm posteriorly, anteriorly, inwardly, outwardly; divergent dislocations with rupture of the proximal articulation and divergence of the bones of the forearm to the sides
- Fractures of the bones of the elbow joint according to the nature of the damage can be divided into: intra-articular;
- periarticular;
- closed;
- open;
- no offset;
- with displacement of fragments (displacement of bone fragments most often occurs with fractures of the olecranon)
- Epicondylitis (“tennis elbow”) is an inflammatory and degenerative disease that affects the tendons in the elbow joint due to chronic overload of the forearm muscles.
- Osteoarthritis is a dystrophic-degenerative disease of the cartilage and bone tissue of the joint.
Pain in the elbow joint when extending
Pain in the elbow, which only bothers you when straightening, may indicate damage to the ligamentous apparatus of the joint or displacement of the bones of the forearm from their normal position. Minor subluxations of the ulna or radius are possible after injuries, a fall on the arm, or sudden movements.
With arthritis of the elbow joint, pain can occur from any movement; selective pain during extension is not characteristic of the inflammatory process inside the joint. If the arm cannot be straightened at all, most likely it will be a subluxation, bone fracture or ligament injury.
Symptoms of pain
The main symptom of elbow disease is pain.
The following signs are typical for the traumatic group of injuries:
- Piercing pain at the time of injury
- Swelling and hematoma in the elbow joint
- Elbow deformity
- Restrictions in arm movements, partial or complete loss of limb function
- Or pathological mobility and the possibility of movements atypical for the elbow
- Numbness or tingling in the forearm, wrist, or hand
- Creaking or clicking noise when moving your elbow
- Any discoloration of the skin in the area of injury
- Palpable protrusion of bone fragments under the surface of the skin
If any of the above symptoms occur, you should immediately seek help from the traumatology department.
Elbow pain when bending
Inflammatory swelling of the joint can cause pain in the elbow that increases with bending. This happens because the swollen tissue puts pressure on the joint and nerves, causing pain. This can be observed in arthritis of any nature: rheumatoid reactive, gouty, etc.
If your elbow hurts when bending, under no circumstances should you try to “straighten” it yourself and press with force, because this can injure the joint capsule and bursae. For arthritis, it is necessary to give the hand the most comfortable position and begin anti-inflammatory therapy.
Treatment Options
Treatment largely depends on the type and nature of the fracture in the elbow joint. For non-displaced fractures (for example, the olecranon), conservative treatment can be achieved by applying a fixing plaster cast for several weeks. If a joint has been displaced, then the issue of surgical intervention is decided. To do this, reposition the fragments (closed or open). With open comparisons, surgical fixation of fragments is required; this operation is called osteosynthesis. Osteosynthesis is the joining of bone fragments using special fixing agents (bone grafts or metal structures). If the fractures of the articular part of the humerus are fragmented, then it is possible to replace the elbow joint with a prosthesis. To restore the function of the elbow joint in case of deforming arthrosis, as well as in congenital and acquired deformities and contractures of other etiologies, osteotomy is currently performed. Osteotomy is a surgical operation that helps eliminate deformation of the elbow joint or improve the function of the musculoskeletal system through an artificial fracture with further fixation to give a functionally advantageous position. After any surgical intervention, the patient is prescribed rehabilitation measures drawn up by the attending physician individually for each person.
The main causes of pain in the elbow joint
- Epicondylitis of the elbow joint is an inflammatory disease of the tendons around the olecranon on the inside or outside. In fact, the disease is not associated with the joint itself and affects only its outer part. The causes of epicondylitis are usually occupational: excessive stress on the elbow, frequent injuries, repetitive movements. Read more about epicondylitis of the elbow joint.
- Bursitis of the olecranon is an inflammation of the connective tissue membrane around the olecranon. Usually associated with repetitive microtrauma, but can also be the result of a systemic disease (gout, rheumatoid arthritis, etc.)
- Bone fractures are not always obvious, especially after minor injuries and with increased bone fragility (osteoporosis). Therefore, if you suspect a fracture, you need to take an x-ray.
- Sprain of the intra-articular ligaments is a possible scenario in both arm sprain injuries and compression injuries of the elbow. Elbow pain will depend on how many ligaments are stretched and how far they are stretched.
- Arthritis of the elbow joint is an inflammation that can be the result of many systemic diseases: gout, rheumatoid arthritis, psoriatic and reactive arthritis, etc. Pain in the elbow occurs at rest, when flexing and extending the elbow. The function of the joint is impaired, external swelling and redness are observed.
- Infection of the skin and subcutaneous tissue (cellulitis) around the joint - may cause pain in the elbow when flexing and extending, but such pain is never felt inside the joint, but only on the skin. A complication may be infectious ulnar bursitis.
- Septic arthritis of the elbow joint is a rare disease that mainly affects people with severely weakened immune systems. Symptoms include high fever, pain and swelling in the joint, and limited movement in the elbow.
- Bone tumors are a very rare scenario for elbow pain. Chondromas can cause pain in the elbow when they are close together, or they may not cause pain symptoms at all. Detected on x-ray and CT scan.
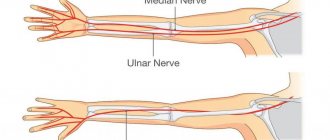
- Pinching of the ulnar nerve is possible along its canal in the elbow area. Typically, the main symptoms are numbness in the little and ring fingers, pain and numbness along the outside of the forearm.
Diagnosis of pain
For elbow pain, diagnosis begins with a consultation. The doctor conducts a survey to find out whether the patient has had any past or recent injuries, surgeries or treatments, and whether there are any hereditary factors that may affect the current condition of the joints. Next, the joint site is examined and felt (palpation), joint mobility and reaction to various positions of the limb are assessed. Most likely, to make a diagnosis you will have to visit several doctors - a surgeon, osteopath, neurologist, as well as a rheumatologist if you suspect rheumatoid arthritis - an autoimmune disease of the joints. A visit to a traumatologist may be required if there are injuries, dislocations, or sprains.
Since pain accompanies many diseases, the examination must exclude tumors and infections. Standard laboratory tests include blood and urine tests, as well as blood biochemistry. This list can be supplemented by tests prescribed by specialists: taking a sample of synovial fluid, tests for rheumatoid factor, C-reactive protein, etc. A comprehensive examination is necessary to timely and accurately determine the cause of the elbow joint disease.
In addition to examination, consultations and tests, diagnostics include:
- ultrasound examination - allows you to see damage to the structure of the joint, signs of inflammation, fluid accumulation, pathological changes in cartilage;
- radiography - shows the condition of the bones that form the joint, reveals bone growths, calcium deposits, deviations in the size of the joint space;
- computed tomography - helps to see all pathological, inflammatory and destructive changes in bone tissue;
- magnetic resonance imaging - reveals degenerative processes, tumors, injuries, foci of infections and inflammations.
Based on the diagnostic results, treatment is prescribed that eliminates the cause of elbow pain and alleviates the patient’s condition.
Reduction
First aid is provided by a traumatologist; you cannot take measures on your own. The doctor will perform a diagnosis and correct the dislocation. You cannot perform this procedure yourself, as it requires certain knowledge. It is also important to undergo an x-ray to rule out the possibility of a fracture.
After realigning the joint, the doctor will apply a tight bandage to the patient's arm. The limb must be fixed in a bent position and suspended in a bandage. For 10 days, it is important to avoid any physical activity, because mobility can lead to re-dislocation. It is important to follow this recommendation to prevent complications.
Massage can be started approximately 5-7 days after the joint has been realigned. It is also important not to forget about physical therapy. You are allowed to do those exercises that your doctor recommends. This will make it possible to prevent the development of contracture, as well as reduce the likelihood of disruption of blood flow in the area of dislocation. You should not do exercises that will cause intense pain. It is important to listen to your body and be careful.
If the elbow joint is dislocated, it is difficult to say how long the recovery will take. Much depends on the degree of damage to surrounding tissues, as well as the injury itself. The recovery period is also influenced by the person’s age, the presence of concomitant diseases, and the correctness of rehabilitation. If there is a rupture of the joint capsule, then recovery may take 3-4 months. When the injury does not damage the tendons and ligaments, the acute symptoms usually subside within two weeks.
The doctor must develop a rehabilitation scheme individually for the person. It depends on whether there are complications and how quickly the problem area is restored. If contracture appears during the period of exclusion of mobility, then it will take longer to develop the arm. When stretching, care must be taken to restore the elasticity of the tissue.
Diagnostics
Ulnar nerve neuritis is detected using the following functional tests:
- if you press the hand with your palm to the plane of the table, the patient will not be able to perform scratching movements with the little finger;
- the patient cannot spread his fingers on his hands, palms pressed to the table;
- the hand on the hand affected by neuritis cannot completely bend into a fist; bending the 4th and 5th fingers is most difficult;
- the last phalanx of the thumb becomes flexible, which prevents the patient from holding a strip of paper between the index and thumb.
Often, the diagnosis of ulnar nerve neuritis requires various electrophysiological procedures. The Health Workshop specialists determine for each patient an individual list of required procedures, which make it possible to accurately determine the localization of inflammation, the specificity and severity of damage to the innervated area.
Treatment
To treat elbow tendonitis, it is important to identify the cause of the pathology. Treatment of a disease that is complicated by tendinitis is often indicated. After injuries, joint fixation is indicated. For the purpose of immobilization, a plaster splint is applied for 2-3 weeks or the joint is fixed using rigid, semi-rigid orthoses.
Next, the rigid fixation is replaced with elastic supports and bandages with silicone inserts. Immobilization prevents further trauma and promotes healing.
Medications
For acute pain and severe swelling of the joint, glucocorticoids (Triamcinolone, Kenalog, Diprospan, Hydrocortisone or Dexamethasone) are prescribed. Hormones are used in short courses due to significant systemic side effects, including progression of tendon degeneration.
If the disease is infectious, the doctor prescribes antibacterial drugs.
Nonsteroidal anti-inflammatory drugs relieve inflammation, eliminate swelling and pain. Apply topically in the form of ointments (Nurofen, Finalgon, Ortofen, Indomethacin, etc.), applied 3 times a day, rubbed into the skin. Systemic NSAIDs are indicated for severe inflammation and persistent acute pain (Diclofenate, Nimesulide, Ketorolac, Ibuprofen, Meloxicam).
NSAIDs have side effects: they can cause drowsiness, dizziness, nausea, vomiting, diarrhea, skin rashes, and swelling. Possible blood changes: anemia, leukopenia, thrombocytopenia. They cannot be used for gastric and duodenal ulcers, liver, kidney and heart failure, pregnancy and lactation, and children under 12 years of age.
“HYAL-IN” and “HYAL-IN PROLONG” are biological products based on hyaluronic acid, which is part of connective tissue. Penetrating into the intercellular spaces, the drug stimulates metabolism, accelerates the regeneration of ligaments, cartilage, joint capsules, and synovial membranes of muscles.
Reference! Biological products “HIAL-IN” and “HIAL-IN PROLONG” have no side effects and no restrictions on the duration of use. Indicated for tendonitis of any etiology, degenerative-dystrophic changes in tendon-ligament structures and soft tissues.
Physiotherapeutic procedures
In subacute tendonitis, hormones and NSAIDs are preferred to 5-7 physiotherapy procedures, which accelerate tendon regeneration and have no side effects.
Laser therapy stimulates metabolic processes in cells, potentiates the healing of collagen fibers, and activates the local immune response.
Magnetotherapy. The electromagnetic field improves blood supply to the tendon, thereby increasing the flow of nutrients and bioactive substances into the cell.
UHF therapy helps resolve swelling, eliminates pain, and increases range of motion.
Electrophoresis is the effect of weak electric current discharges on the affected joint. A metal plate is placed on top of the napkin soaked in the preparation. When current passes, drug molecules penetrate directly into the area of inflammation, which is effective and safe.
After the elimination of acute phenomena, physical therapy (stretching exercises) is prescribed.
Reference! If conservative therapy is ineffective, surgical treatment is indicated - excision of the inflamed tendon.