Ulnar nerve compression (UCN) can occur in two places: at the elbow and at the wrist. SLN at the elbow joint occurs in the cubital tunnel (cubital tunnel syndrome). Ulnar nerve neuropathy in the cubital tunnel is the second most common compression neuropathy (the first most common neuropathy is associated with entrapment of the median nerve in the carpal tunnel). Ulnar neuropathy is less commonly seen in Guyon's canal (Guyon's canal syndrome/ulnar carpal syndrome).
Causes
SLN in the cubital and Guyon's canals occurs due to repetitive compression due to support on the elbows or wrists (cyclist's palsy) or prolonged flexion of the elbow. It can also occur due to trauma, swelling, fracture, vascular and bone pathologies/disorders.
Ulnar carpal syndrome occurs when the ulnar nerve becomes compressed between the hook of the hamate bone and the transverse carpal ligament. Guyon's canal syndrome is considered an overuse injury that is typically caused by direct pressure on the handlebars (eg, bicycle handlebars, weight lifting, heavy equipment) and is thus sometimes referred to as "steering wheel palsy." This syndrome may also result from intense gripping, rotation, or repetitive movements of the wrist and hand. Impingement can develop if the hand is flexed and the elbow is abducted for an extended period of time.
The incidence of injuries leading to ulnar nerve compression is unknown; however, ulnar neuropathy has been documented after distal humerus fractures, of which up to 10% are associated with elbow dislocation, and can also develop following any complex trauma to the elbow or wrist.
Clawed hand - causes, symptoms, what it looks like and how to treat it?
A clawed hand is a characteristic symptom of ulnar nerve damage. Permanent nerve damage can occur as a result of nerve injury, cutting injury. Sometimes the appearance of a clawed hand is temporary and reversible, for example as a result of abnormal pressure on the ulnar nerve. Ulnar nerve dysfunction can be treated conservatively or surgically.
Fotolia
Clinical picture
Symptoms of ulnar nerve compression include tingling in the 4th and 5th fingers, weakness when grasping objects with the hand, pain and tenderness in the ulnar aspect of the wrist, forearm and hand, muscle atrophy, and inability to straighten the 4th and 5th fingers (a sign of blessing).
Cubital tunnel syndrome can manifest itself in varying degrees of severity:
Grade I: Mild symptoms such as:
- Periodically occurring paresthesia.
- Some decrease in sensitivity of the dorsal and palmar surfaces of the fifth and medial parts of the fourth fingers.
- No movement disorders.
Grade II: Moderate and persistent symptoms such as:
- Paresthesia.
- Hypesthesia of the dorsal and palmar surfaces of the fifth and medial parts of the fourth fingers.
- Mild weakness in the muscles innervated by the ulnar nerve.
- Early signs of muscle atrophy.
Grade III: Severe symptoms such as:
- Paresthesia.
- There is obvious loss of sensation on the dorsal and palmar surfaces of the fifth and medial aspects of the fourth fingers.
- Significant functional and motor impairments.
- Muscular atrophy of the deep muscles of the hand.
- Inability to straighten the fourth and fifth fingers (a sign of blessing).
Symptoms of Guyon's canal syndrome include:
- Muscle atrophy - mainly in the hypothenar and interosseous muscles, without affecting the palmar muscles:
- weakness when abducting and adducting the fingers (interosseous muscles);
- weakness in adduction of the thumb (abductor pollicis muscle).
- Sensation loss and pain that may involve the palmar aspect of the fifth finger and the medial aspect of the fourth finger, but the dorsal and medial aspect of the fourth finger and the dorsal aspect of the fifth finger do not lose sensation.
- The symptom of a “clawed” hand (a sign of blessing) may be present.
Treatment of ulnar nerve neuritis
Treatment for ulnar nerve neuritis is selected individually in each specific case. It includes a set of conservative procedures:
- acupuncture
- nerve and muscle stimulation
- vitamins of group “B”, “C” and “E”
- antiviral drugs
- homeopathic remedies
- surgical treatment (neurolysis, suturing of the nerve trunk, etc.)
Elimination of paresthesia and pain, restoration of muscle strength in the treatment of ulnar nerve neuritis is accelerated by the use of physiotherapy.
Physiotherapeutic examination
Elbow carpal syndrome: It is important to rule out other diagnoses that may be related to the elbow joint. Physical examination includes:
- Assessment of range of motion of the wrist and fingers.
- Manual muscle testing of the ulnar nerve muscles innervated distal to Guyon's canal.
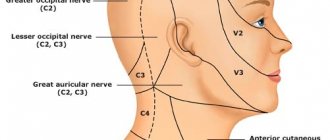
- Sensory examination of the cutaneous branches of the ulnar nerve distal to Guyon's canal
- Assessment of atrophy of the deep muscles of the hand.
Friends, on April 11-12 in Moscow there will be a seminar by Anna Ovsyannikova “Fundamentals of anatomy and biomechanics of the hand. Diseases and injuries of the hand and fingers." Find out more...
Special tests
- "Card" test.
- Froment's sign
- Tinnel's sign in Guyon's canal.
- The Ulnar Nerve Neurodynamic Test (ULTT3) may increase the patient's symptoms.
Diagnostic tests to determine ulnar nerve compression
- Visualization of osteoarthritis, osteophytes or bone cysts.
- Nerve conduction studies (EMG).
- If there is a suspicion of a fracture/dislocation, a plain X-ray.
Diagnostics
When a patient consults a doctor with complaints about symptoms characteristic of ulnar nerve neuropathy, diagnostic measures are prescribed aimed at identifying the true factors that may affect not only the ulnar nerve, but also the radial nerve.
Testing a patient using the Froman method is quite effective for diagnosing neuropathy. In this case, patients are asked to perform several simple tasks:
- It is necessary to press the paper sheet firmly with your thumbs onto a flat surface. With a positive test for neuropathy, the patient constantly bends the thumb in the phalanx, and if necessary, it is almost impossible to straighten the finger.
- To confirm pinching of the ulnar nerve, the doctor applies several light blows to the cubital canal with the edge of the palm or fingers. When symptomatic signs intensify and become more pronounced, which is classified as Tinnel's sign, the presence of ulnar neuropathy is confirmed.
- Using light tingling and palpating of the hand, the degree of loss of sensitivity (paresthesia) is determined. The most common symptom of neuropathy is partial paresthesia.
Positive Tinnel's sign indicating ulnar nerve involvement
In all cases, patients are referred for instrumental diagnostics, which includes the following research methods:
- X-ray examination and MRI, necessary to determine various defects in the bone structure that cause the development of compression of nerve endings in the elbow or hand;
- Ultrasound is used to visualize changes in the structure of the nerve trunk (at the site of entry into the cubital or Guyon's canal);
- Electromyography (ENG) detects impulse conduction disturbances occurring below the compression area.
Electromyography allows the doctor to identify the location of the lesion in order to determine the activity of the ulnar nerve
In addition, the doctor can prescribe a number of laboratory tests (blood, urine, etc.) to more accurately determine the cause of the development of the pathological condition. After diagnostic measures, treatment procedures are prescribed, the purpose of which is to relieve negative symptoms as quickly as possible.
Criteria for evaluation
- Disabilities of the Arm, Shoulder, and Hand (DASH) is a 30-question questionnaire designed to assess patient function and symptoms.
- The Patient Specific Functional Scale (PSFS) is a questionnaire used to assess a patient's activity limitations and functional outcomes.
- The DASH assessment criteria are a questionnaire that assesses a patient's functional ability and symptom severity.
- The Upper Extremity Functional Inventory (UEFI) is a 20-question questionnaire designed to measure the severity of complex tasks performed throughout the day.
How is bird's foot diagnosed?
Call your doctor if you notice that your hand begins to feel like a bear's claw. You should also contact your doctor if your symptoms get worse or if treatment doesn't help.
A doctor can diagnose claw hands based on the appearance of your fingers. However, your doctor may need to do a test to determine the cause and severity of the condition.
Medical history
Your doctor may ask you questions about your medical history to determine whether your symptoms are the result of a past injury or illness.
Medical checkup
The doctor may ask you to flex your fingers and grasp an object, in addition to other tests, to see how much strength and flexibility you have in your fingers and hand.
Electromyography
An electromyography test (EMG) checks how well your nerves are working. To perform an EMG, your doctor will insert thin needles through the skin into the muscles in your arm. The needles are connected to a machine that measures electrical impulses from your nerves as you move. You may feel a little discomfort from the small needles, but it is usually not painful. There may be some minor bruising and some pain for a few days after the test.
If the results of an EMG test show that you have abnormal nerve activity, your doctor may do additional tests to determine the cause of your nerve damage. The tests your doctor will perform depend on your medical history and other symptoms you may experience.
Physical therapy
- An impairment assessment approach may be used to identify strength deficits, decreased range of motion, and problems in achieving functional goals.
- The source of pain must be treated in conjunction with the disorder.
- After treatment, re-evaluate the functional tasks that caused pain to determine the effect of treatment.
- Create an exercise program to do at home to treat impairments and perform functional tasks.
A study conducted by Swernlov compared three types of treatment for patients with elbow tunnel syndrome. All three groups showed positive results; the control group showed similar improvement as the intervention groups.
- Splint group protocol —patients wore an elbow splint every night for 3 months to prevent elbow flexion greater than 45 degrees.
- Neural glide protocol – patients did neurodynamic exercises twice a day in six different positions, which were held for 30 seconds (three sets); the break between repetitions was 1 minute. Patients were instructed how to perform these exercises until their next follow-up visit, which was 1–2 weeks later. If no symptoms were found at the next visit to the doctor, the frequency of exercise was increased to three times a day with the position held for 1 minute (every day for 3 months).
- Control Group Protocol – The control group received only educational recommendations.
According to a study report by Coppieters, administration of elbow joint mobilization, thoracic spine and rib thrust manipulation, and ulnar nerve glide/tension techniques for 6 sets was associated with a reduction in elbow pain and a significant improvement in scores on a self-assessment questionnaire. cervical spine for at least ten months of observation. Patients reported a history of symptoms in the two months prior to physical therapy.
Treatment methods
At the initial stage of the disease, conservative treatment of ulnar nerve neuropathy is provided, with the exception of tunnel syndrome, which appears as a result of gross deforming changes in the canal.
First of all, it is necessary to reduce the likelihood of injury in the canal of the pinched nerve. With ulnocarpal syndrome, the patient is advised to avoid grasping movements, as well as resting on the hands and any actions that require dorsal extension of the hand.
Conservative therapy
If compression develops, it is necessary to resort to the help of orthopedic and fixing devices that limit compression during movement of the ulnar nerve. In this case, splints, bandages and orthoses can be used. In some cases, they are recommended to be worn only at night.
In cases where compression of the nerve is caused by movement or a habit caused by professional activity, the patient should abandon them and limit motor activity in the elbow so as not to provoke an increase in pain symptoms.
To eliminate pain, as well as the inflammatory process in tunnel neuropathy, in the initial stage of the disease, NSAIDs (Diclofenac, Indomethacin, Nimesulide, Meloxicam, Ibuprofen, etc.) are prescribed. Locally, you can use the Versatis medicinal patch, which contains Lidocaine, which has an analgesic and anesthetic effect.
In case of pronounced swelling, it is recommended to take diuretics (Furosemide, Lasix, Hypothiazide, Veroshpiron, etc.), which have a diuretic and anti-inflammatory effect. In order to improve nerve nutrition, it is necessary to take B vitamins (Neurovit, Milgamma, Combilipen, Neurovitan, etc.).
As a rule, such procedures quickly eliminate the symptoms of ulnar nerve neuropathy, providing a long-term therapeutic effect.
In case of insufficient effectiveness and progression of the inflammatory process, you can use injections of a mixture of Lidocaine (Novocaine) and Hydrocortisone directly into the Guyon canal (cubital)
Surgery
If the therapeutic and physiotherapeutic measures taken are ineffective, as well as if there is a pronounced scar change in the place where the nerves pass through the canals, a decision is made to perform surgical intervention.
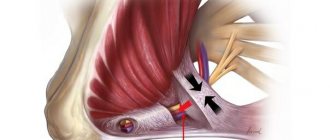
The main focus of such operations is the removal or dissection of structures that compress the ulnar nerve. In case of compression of the cubital canal, plastic surgery is recommended to remove a limited area of the epicondyle with subsequent creation of a new canal in order to ensure free movement of the nerve. For Guyon's canal syndrome, an incision is made in the palmar carpal ligament located above the canal. In this case, surgery relieves the ulnar and median nerves from compression.
Performing surgery on Guyon's canal to relieve pressure on the nerve allows restoration of nerve innervation
After the operation, immobilization of the limb with a splint or splint is required for at least 7-10 days. After 20-30 days, the patient is allowed to perform passive movements, and increasing the load is permissible no earlier than after 2 months.
The total duration of the rehabilitation period after surgery is 3-6 months.
However, it is important to remember that complete restoration of the lost functionality of the ulnar nerve is possible only with additional therapy in the postoperative period (diuretics, vitamins, drugs to improve nerve innervation and nutrition, analgesics, etc.). In addition to drug intervention, exercise therapy and physiotherapeutic measures are required during the rehabilitation period.
Exercise therapy
Physical therapy, which includes the following exercises, is of no small importance in the general treatment of neuropathy:
- the patient is asked to press (5-6 times) on the phalanges of the fingers, achieving their full straightening;
- all fingers of the affected limb (from the thumb to the little finger) are raised (alternately) with the healthy hand at least 10 times for each finger;
- starting with the thumb, all the rest are pulled back with the healthy hand 10 times;
- It is recommended to perform circular movements with all fingers in both directions;
- 4 fingers, starting with the index and ending with the little finger, rise and fall with maximum straightening;
- the sore elbow is raised with the healthy arm and slowly lowered onto the edge of the palm (from the little finger), followed by circular movements of the wrist, first 10 times in a clockwise direction, and then in the opposite direction;
- The hand should be placed on the edge with the fingers apart and slightly bent, after which it is necessary to straighten the fingers with springy movements. This exercise should be repeated 10 times (for the left and right elbow);
- the patient is asked to grab, feel, squeeze, move a paper napkin placed on a flat surface with slightly bent arms while simultaneously moving the base of the palm forward, repeating at least 10 times for each hand. You can grab and squeeze rubber balls of different sizes in your brush.
As motor activity is restored, the individual gymnastic complex can expand, with more complex tasks, for example, modeling from clay or plasticine, collecting small objects, etc.
The principle of working with plasticine (clay) for the effective development of the ulnar nerve during the rehabilitation period
The effectiveness of the rehabilitation period depends on the timeliness of started therapy. When the inflammatory process is advanced, even surgical intervention does not guarantee complete restoration of nerve conduction, and partial paresis can accompany the patient throughout his life.
Neuropathies of the ulnar nerve are provoked by various reasons that determine further treatment tactics. The prognosis for recovery (full or partial) directly depends on the cause of the development of negative symptoms. When ulnar nerve decompression is performed early, almost all patients return to normal function. During surgical intervention in patients over 50 years of age, positive results are extremely rare. In patients of the older age group, the prognosis for recovery sharply decreases.
Differential diagnosis
The cervical spine and shoulder girdle should be examined to rule out diagnoses that may relate to the elbow joint. There are many differential diagnoses for ulnar nerve entrapment.
- Elbow fracture/dislocation.
- Cervical radiculopathy.
- Thoracic outlet syndrome.
- Peripheral vascular disease.
- Damage to the collateral ligament of the elbow joint.
- Rheumatoid arthritis.
- Medial epicondylitis.
- Acute polyradiculoneuritis (Guillain-Barré syndrome).
- Neuropathy associated with alcohol (ethanol) consumption.
- Amyotrophic lateral sclerosis.
- Tumor of the apex of the lung.
- Primary bone tumors.
- Peripheral polyneuropathy.
Key Points of Physical Therapy
- Special tests used in diagnosing ulnar nerve entrapment have very high sensitivity - 0.98 or higher - and are therefore very useful in making the diagnosis.
- Conservative treatment is effective in approximately 50% of cases, while surgery is effective in 60-95% of cases.
- Conservative treatment has been shown to be effective when introducing the use of orthoses and manual therapy, including neurodynamics and joint mobilization; however, a recent study highlighted that more research is needed to know when conservative versus surgical treatment is needed.
- A patient who begins conservative treatment earlier has a 30% higher chance of avoiding surgery.