13 May 2020
173531
1
3.8 out of 5
Sciatica is sometimes also called lumbosacral radiculitis - a chronic neurological disease in which the sciatic nerve passing through the buttock and leg is compressed. This is accompanied by severe pain and a number of other disorders. It can occur at any age in people of both sexes, often occurs in pregnant women, but is most often diagnosed in people 40–60 years old. Although sciatica is not life-threatening, it can significantly reduce the quality of life and deprive a person of ability to work. Therefore, when the first signs appear, you should contact a neurologist and begin treatment immediately. In this case, it will be as easy as possible, effective and will allow you to quickly eliminate both the signs of the disease and the causes of its occurrence.
What is sciatica
Sciatica is a non-inflammatory disease that occurs due to compression of the sciatic nerve in any area. The concept of “sciatic nerve sciatica” is not used either in the literature or in everyday life, since the term “sciatica” is used exclusively to describe cases of compression of the sciatic nerve and no other.
The sciatic nerve itself is paired and is one of the largest nerves in the human body. Its two branches begin at the sacral nerve plexus, located in close proximity to the vertebrae and sacrum, and run symmetrically along the buttocks, down the back of the thighs and reaching the legs.
The sacral nerve plexus is formed by closely intertwined nerves that run along both sides of the spine from its outer side.
In the upper part of the leg, the sciatic nerve is divided into 2 large branches: the peroneal and tibial. They pass along the back of the lower leg on the right and left.
Thus, the sciatic nerves are quite long, so sciatica can be caused by a huge variety of different causes. And depending on the area where the nerve fiber was compressed, there are 3 types of sciatica:
- upper – the cord or spinal roots at the level of the lumbar vertebrae of the spine are subjected to compression;
- middle (plexitis) – the sciatic nerve is pinched in the area of the sacral nerve plexus;
- lower - pinched nerve fiber is observed in any part along its entire length from the buttock to the foot.
Most often, it is lower sciatica, which is often called neuritis. But since the latter term describes an inflammatory lesion of the nerve, its use as a synonym for sciatica is not entirely correct. Indeed, with sciatica, pain is caused solely by compression of a nerve in one area or another, while with neuritis it can be involved in the inflammatory process or be pinched by hyperemic tissues.
You should not let the course of the disease take its course. Non-intervention and ignoring the symptoms of sciatica is fraught with changes in the lower extremities, which can ultimately lead to loss of performance and the ability to care for oneself independently.
Symptoms of a pinched nerve in the leg
Signs indicating a pinched nerve in the lower extremities are as follows:
- The appearance of acute and sharp painful sensations in the pinched area. They may also be tingling;
- Swelling of the epidermis, change in shade to red at the pinching point;
- Increased sweating (quite rare);
- Inability to straighten limbs in the morning. As the disease worsens, this symptom becomes permanent.
- The patient appears more constrained; when in an upright position, unbearable pain is noted;
- Painful sensations can also reach the back area.
Most often, symptoms of this kind appear unexpectedly, but disappear just as quickly. In later stages of the disease, the presented sensations continue uninterrupted. In the area in which the pain is felt most strongly, there is precisely the point where the nerve is pinched. This may be due to both physical and psychological influences.
Painful sensations may also occur during sleep. Additional factors that determine pinched nerves in the lower extremities, as mentioned above, may be redness and swelling of the skin. Constant sweating is sometimes added to this. There is a worsening of motor activity in situations where the motor nerve is affected, and sometimes atrophy.
Causes
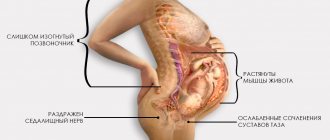
Compression of the sciatic nerve can occur in a variety of different cases. This can occur due to injuries to the legs, pelvis and back, during pregnancy, prolonged immobility, pinched nerves by fibrous cords or neoplasms, etc.
Most often, sciatica becomes a complication of various spinal diseases, including:
- lumbar osteochondrosis - degeneration of large intervertebral discs of the lumbar spine is the main prerequisite for the development of other spinal diseases and pinching of nerve fibers of different sizes;
- the formation of intervertebral hernias is the most common complication of osteochondrosis, manifested by protrusion of the disc, which leads to compression and damage to the spinal roots;
- spondylolisthesis – displacement of the vertebrae relative to the underlying one by different amounts, which can provoke pinching of the nerve roots;
- facet syndrome - nerve fibers are pinched in the narrow natural openings of the spine as a result of deformation of the vertebrae, the formation of osteophytes, or other disorders.
Another common cause of sciatica is spasm of the piriformis muscle located in the buttock. Since the sciatic nerve passes through it, an increase in its tone leads to stretching and irritation of the nerve fiber, which immediately results in severe pain.
Other prerequisites for the development of sciatica include:
- excessive physical activity;
- spinal tumors of various natures from hemangiomas to malignant neoplasms;
- arthritis;
- thrombosis of blood vessels;
- hypothermia and the development of inflammatory processes in anatomical structures adjacent to the spine at the level of the lumbosacral region;
- infectious gynecological and other diseases, including influenza, tuberculosis, typhoid fever, sepsis (released toxins affect the sheath of the sciatic nerve);
- spinal deformities (scoliosis, etc.).
Causes of a pinched nerve
The main sign of a pinched nerve in the cervical or lumbar spine is severe pain in this area. In the first case, pain accompanies numbness of the hands, in the second case - numbness of the limbs (legs), the causes of which lie in the disruption of the functioning of the nerve endings located in the spine.
Pain from a pinched nerve can be of different types:
- Unilateral pain radiating to the thigh or buttock.
- Numbness, feeling of heaviness and cramps in the leg.
- Lumbago - sharp painful shootings.
- Constant aching pain.
A pinched nerve in the cervical spine can impair blood supply to the brain and cause:
- Increase or decrease in blood pressure.
- Visual and hearing impairments.
- Dizziness.
- Headache.
In this case, pain appears in the neck, which is especially severe when turning the head and radiates under the shoulder blade, into the forearm or shoulder, and is intense.
Symptoms
As a rule, the development of sciatica occurs gradually. The first signs are of a mild discomfort and are often perceived by people as a manifestation of banal fatigue after performing physical work. Initially, there may be slight pain in the lumbar region, which radiates to the buttock. In this case, slight discomfort occurs in the leg along the back of the thigh.
The belief of patients that such symptoms are a consequence of overwork and the fact that they occur mainly after physical exertion and disappear without a trace after a short rest are rooted. This condition can persist for several years and is already perceived by the patient as normal.
But sooner or later, lifting an object that is too heavy, hypothermia, or simply careless movement provokes an attack. A person is constrained by pain. It interferes with normal mobility and is often accompanied by autonomic and neurological symptoms.
A specific symptom of sciatica is unilateral pain affecting only one of the buttocks and one leg. As a result of the progression of pathological changes, it increasingly differs in functionality and even appearance from a healthy leg: it is cold to the touch, smaller than healthy, the skin is pale and dry.
The nature of the disorders directly depends on which of the fibers of the sciatic nerve are affected as a result of infringement: motor or sensory. Thus, patients may suffer from:
- decreased sensitivity of the skin of the affected lower limb; sometimes, on the contrary, there is increased sensitivity of the outer edge of the foot;
- muscle weakness in the legs and feet;
- changes in tissue nutrition, which leads to pale skin and thinning;
- disorders of the pelvic organs, which may be accompanied by loss of control over the process of urination and defecation;
- bowel dysfunction, etc.
Sciatica typically has a paroxysmal course with periodic exacerbations.
Manifestations of the disease may vary in intensity and nature. In some cases, acute pain comes to the fore, in others, patients will complain more about limited mobility or other symptoms, mentioning pain only in passing. Thus, sciatica can manifest itself in varying degrees of pain, motor, sensory and neurological impairment. Let's take a closer look at each group of symptoms separately.
Sciatica pain
The nature of pain when the sciatic nerve is pinched can be different. During an attack they are sharp, powerful, burning and shooting. Patients describe them as being struck with a knife or electric shock. Literally any movement or change in body position is extremely painful, and bending or sitting leads to a sudden aggravation of the pain syndrome. Often the pain does not subside even when lying down.
With chronic sciatica, the pain may not be so severe. They are often nagging, aching, present constantly or appear after physical activity. Just as with an attack, they tend to get worse during bending, lifting a leg, or prolonged sitting or standing.
With sciatica, the epicenter of pain is in the lumbosacral spine or directly in the area where the sciatic nerve is pinched. But a typical feature of the disease is the spread of pain along the nerve, i.e., along the buttock, back of the thigh, lower leg, and sometimes even to the toes. To reduce pain, a person takes a forced body position. He leans forward and to the side.
When you try to turn the affected leg bent inward at the hip and knee, a sharp pain occurs in the buttock.
Motor and sensory disorders
The sciatic nerve is formed by sensory and motor fibers. It is responsible for providing sensitivity and mobility to the muscles of the back of the legs. Therefore, when it is compressed, both motor and sensory disorders may occur. They can manifest themselves in varying degrees, be combined with pain or be isolated. In most cases, one or more of the following symptoms are present. Combinations can be different, so different patients with sciatica rarely have the same clinical picture:
- decreased sensitivity of the skin along the lateral and posterior surface of the lower leg and throughout the entire foot;
- the presence of tingling, numbness, goosebumps;
- violations of flexion and extension of the muscles of the back of the thigh and lower leg, which negatively affects the work of the knee and ankle joints and, accordingly, gait (it seems that a person does not bend his leg at all when walking);
- difficulties when bending;
- weakness in the foot, which can literally hang completely motionless on the shin;
- reduction in muscle size due to their gradual atrophy;
- complete paralysis of the muscles of the foot and the back of the thigh and lower leg (with severe sciatica);
- dryness, peeling, thinning, paleness or, conversely, redness of the skin of the lower extremities;
- increased sweating;
- thinning and brittle toenails.
Over time, it becomes increasingly difficult for the patient to walk, since the affected leg loses stability and cannot fully perform its supporting function. There is progressive weakness and lameness.
Impaired nerve conduction can lead to insufficient tissue trophism, which can result in osteoporosis. In such cases, fractures often occur, even under the influence of factors that are normally unable to disrupt the integrity of the bones.
Osteoporosis is a disease in which bone tissue becomes porous, loses its normal strength and becomes brittle.
Symptoms - neurological manifestations
Since the sciatic nerve is pinched in one place or another, this is accompanied by impaired conduction of nerve impulses and a decrease in the intensity or complete loss of reflexes. It is the presence of such symptoms that most often helps a neurologist make the correct diagnosis.
With sciatica, the following are practically not manifested or are completely absent:
- Achilles tendon reflex - a blow with a hammer or the edge of the palm to the Achilles tendon when a person takes a lying position on his stomach normally provokes the foot to move back to a position as if the person is standing on tiptoes;
- knee reflex - hitting a point under the knee with a hammer or the edge of the palm normally leads to extension of the knee joint if a person sits on the edge of the bed with his legs hanging freely;
- plantar reflex - passing the tip of a milk or any other blunt object along a relaxed foot from the heel to the toes provokes its flexion.
Also a clear neurological sign of sciatica is the occurrence of severe pain in the lower back, buttock and thigh when trying to lift a straight leg while lying on your back. When bending the leg, its intensity decreases.
In addition, at some points the sciatic nerve runs very close to the skin: in the subgluteal fold, the back of the knee, the center of the lower leg and in the area of the Achilles tendon. Such points are called Vallee points. Therefore, pressing on them provokes an attack of pain in the presence of sciatica.
Read also
Epicondylitis
Do you know this disgusting feeling when you are passionately doing something, and suddenly, completely by accident, your elbow bumps into something hard and in that very place, after the impact of which the whole arm weakens,…
Read more
Aphasia
Aphasias are speech defects that appear with minor brain damage, most often affecting the left hemisphere in right-handed people, and consisting of various forms of speech changes. Location and size...
More details
Clubfoot
Clubfoot should not be understood as just one foot disorder. This is a group of deformities of the foot and ankle joint with their pathological setting. Clubfoot is a deformity in which...
More details
Amyotrophy
The word atrophy, translated from Latin, means loss or decrease in the volume of muscle mass or an individual muscle. Most often, muscle atrophy occurs due to limitation of active movements, for example, after...
More details
Lambert-Eaton syndrome
The first description of the disease in the literature appeared in 1953. J. Anderson described a case from practice: a 47-year-old man with lung cancer experienced symptoms similar to myasthenia gravis. After tumor removal...
More details
Diagnostics
A neurologist diagnoses and treats sciatica. It is this specialist who should be contacted if any of the above symptoms occur. Already during the first appointment, based on the patient’s complaints and examination, the doctor may suspect compression of the sciatic nerve. But in order to find the most effective treatment, you need to find out why this happened. For this purpose, the patient is prescribed a set of studies, thanks to which the condition of the intervertebral discs, joints, bones, etc. can be assessed.
Therefore, as part of the diagnosis of sciatica and the causes of its occurrence, the following are used:
- X-ray of the sore leg, sacrum and lower back - the results of the study show the condition of the vertebrae and partly the intervertebral discs;
- MRI – provides comprehensive information about the condition of the intervertebral discs and spinal cord;
- CT is an informative method that allows you to detect pathologies of the sacrum and lumbar vertebrae;
- Electroneuromyography – provides data on the quality of transmission of nerve impulses to the muscles of the lower extremities and their contractility.
The most informative method for diagnosing diseases of the cartilage tissue from which intervertebral discs are formed, as well as pathologies of the spinal cord, is MRI. It is this method that allows you to thoroughly examine the discs, assess their size, position, and detect the slightest hernia and other disorders.
Causes of a pinched nerve in the leg
A pinched nerve in the lower extremities can form due to the following factors:
- Osteochondrosis at the acute stage. Cartilage and discs, changing their shape, leave a small space that highlights the vertebrae. This has a positive effect on increasing compression in the area of the nerve branches. If we talk about muscles, then they, being in a much more active state and with increased tone, further aggravate the situation. Indeed, in connection with this, painful sensations turn out to be much more noticeable;
- Radiculitis. As you know, a large number of people over the age of 45 are faced with this disease. It is this disease that can cause a pinched nerve in the leg. The pain can be so severe that prolonged loss of consciousness is even possible. In this regard, at a critical moment it is necessary to reduce pain as soon as possible;
- Tumors of any origin;
- Loads that involve heavy or prolonged physical labor;
- Received injuries that change the optimal structure of the bones and thereby affect pinching.
Conservative treatment of sciatica
One can hope for a lasting improvement in the condition and elimination of pain in the buttock, back of the thigh and lower leg only if the factor that caused the pinching of the sciatic nerve is eliminated. Otherwise, all attempts to improve the patient’s condition will either be ineffective or will produce a weak, short-term effect. The modern level of development of medicine makes it possible to eliminate, conservatively or surgically, almost any disorder that provokes compression of the sciatic nerve. But the sooner they are detected and treatment started, the better the prognosis will be.
Therefore, patients are always prescribed complex treatment, consisting of symptomatic and etiotropic therapy, selected according to the detected cause of sciatica. In this way, it is possible to improve the patient’s condition and eliminate the risk of relapse of the disease.
In most cases, conservative therapy is initially prescribed. Only in particularly advanced cases, when severe pathologies of the spine are detected, is surgical intervention immediately recommended to the patient. As part of conservative treatment, patients are prescribed:
- drug therapy;
- physiotherapy;
- exercise therapy;
- manual therapy.
Also, with sciatica, wearing fixation belts has a positive effect on the patient’s condition.
But conservative therapy, unfortunately, does not always give the desired results and in certain cases it is impossible to eliminate the causes of sciatica without surgery. Then patients are recommended to undergo surgical intervention appropriate to the situation.
Drug therapy
Directly to improve the patient’s condition with sciatica, the following are prescribed:
- NSAIDs and non-narcotic analgesics are used to relieve pain, and drugs from the NSAID group additionally provide an anti-inflammatory effect;
- corticosteroids - used to eliminate severe inflammatory processes and quickly reduce the swelling of soft tissues caused by them;
- muscle relaxants – help eliminate muscle spasms that occur in response to attacks of pain and help break the vicious circle of “pain - spasm - pain”;
- antioxidants, B vitamins - are used to improve tissue trophism and normalize nerve conduction along the sciatic nerve, which allows for improved sensitivity and elimination of numbness;
- angioprotectors and microcirculation stimulants - help improve microcirculation, and therefore prevent muscle atrophy and restore the sciatic nerve;
- metabolic drugs - used to improve the quality of nutrition of nerve fibers and their restoration;
- products for topical use - ointments with bee, snake venom, other warming and irritating substances, as well as containing NSAIDs, help reduce pain and stimulate local blood circulation.
If, despite conservative therapy, acute pain does not go away or a new attack occurs, patients may be given novocaine or lidocaine blockades. Such procedures are performed only in a medical facility, since they require compliance with sterile conditions and thorough mastery of special skills. When performing a blockade, anesthetics are injected directly into the area where the nerve bundles pass. This prevents the passage of painful nerve impulses and quickly leads to improvement. But the blockade does not affect the causes of pain, but only temporarily eliminates them.
In severe cases, when pain is not relieved by any other methods, patients are prescribed opioid analgesics. They are taken in short courses under the supervision of a doctor, as they quickly cause addiction and drug dependence.
Etiotropic therapy is selected strictly individually based on the nature of the detected pathologies. So, for example, when infectious diseases are detected, treatment will necessarily include antibacterial and antiviral agents, etc.
Physiotherapy
Physiotherapeutic procedures are widely used for sciatica. They help to activate blood circulation in the affected area, reduce pain, restore sensitivity and relieve swelling. The most effective are:
- diadynamic currents;
- darsonvalization;
- laser therapy;
- magnetic therapy;
- UV therapy;
- ultrasound therapy.
Electrophoresis is often indicated for sciatica. The essence of the method is to deliver drugs directly to the right place using electric current. This ensures a pronounced therapeutic effect and rapid improvement in the patient’s condition. Using electrophoresis, anti-inflammatory, antispasmodic agents, as well as muscle relaxants can be injected into the area of compression of the sciatic nerve.
Exercise therapy
Physical therapy for sciatica plays an important role. A properly selected set of exercises allows you to relieve muscle spasms, activate metabolic processes and thereby speed up the process of nerve fiber restoration and eliminate soft tissue swelling.
The exercise therapy program is selected for each patient individually, taking into account the nature of the existing spinal pathologies. Therefore, only a specialist can cope with this task.
For sciatica, most exercises are recommended to be performed lying on a hard surface. Initially, the doctor selects light exercises and requires a small number of repetitions. The first classes are conducted under his supervision so that the patient can fully master the correct technique of the proposed exercises and continue to practice independently.
Gradually, the complexity of the exercises is increased and the load is increased in order to achieve optimal results. But this can also only be done under the strict supervision of a specialist.
It is necessary to do exercise therapy every day. Exercises are performed slowly, without sudden movements. And if pain occurs, you should immediately stop exercising and consult a doctor.
Manual therapy
Properly conducted manual therapy sessions increase the effectiveness of the treatment and contribute to a rapid improvement in the condition. The use of special techniques of manipulation, mobilization, post-isometric relaxation and others can not only improve blood circulation in the affected area and relieve muscle spasms, but also normalize the position of the vertebrae, increase the distance between them to normal levels and release pinched nerve fibers. This quickly leads to relief and normalization of the patient’s condition.
But manual therapy sessions can only be trusted by qualified specialists, since incorrect movements or lack of understanding of the effects on the spine in certain diseases can cause significant harm and provoke the development of unwanted complications.
Sciatica is not uncommon during pregnancy. But due to the fact that during this period the use of most medications is unacceptable, manual therapy is one of the main ways to relieve pain and improve the condition of women before childbirth.
Surgery
The operation is indicated if conservative therapy is ineffective and severe pain that cannot be eliminated by conservative methods persists for more than 6 weeks, as well as in the presence of:
- large intervertebral hernias;
- spondylolisthesis;
- spinal deformities;
- hemangiomas, chondromas and other spinal tumors;
- severe dysfunction of the pelvic organs, leading to urinary or fecal incontinence.
In such situations, conservative therapy will, at best, slow down the development of these pathologies, but not eliminate them completely. But if in the isolated existence of, for example, an intervertebral hernia, this is enough to improve the patient’s condition, then in cases where the presence of spinal pathology provokes the addition of sciatica, such measures will not be enough.
After all, the cause of the pinched sciatic nerve remains, it continues to suffer and cause the corresponding clinical picture. Therefore, in such cases, surgery is the only way to achieve a lasting improvement in the condition, restore a normal quality of life and eliminate the risk of loss of ability to work.
But even if there are indications, surgical intervention cannot always be performed. It is contraindicated for:
- pregnancy;
- infectious and inflammatory diseases;
- decompensated diabetes mellitus;
- serious respiratory or heart failure.
A timely operation can completely eliminate the causes of sciatica.
Surgical treatment of sciatica for intervertebral hernias
Herniated discs are a common cause of sciatica. Moreover, the severity of symptoms of nerve entrapment does not always depend on the size of the protrusion. Sometimes even small hernias can cause serious pain, limited mobility and neurological disorders.
Today, the problem of intervertebral hernia can be completely solved only by surgery, but the type of operation directly depends on the size, location and other features of the hernia. For small protrusions, preference is given to percutaneous surgical methods: nucleoplasty and hydroplasty.
In both cases, the essence of the operation is to destroy part of the nucleus pulposus of the disc, which leads to a reduction in the size of the hernia or even its retraction due to the creation of reduced pressure inside the disc. Percutaneous surgery techniques involve the use of thin cannulas, the diameter of which does not exceed several millimeters.
Operations of this type can be performed under general or local anesthesia. The instruments are inserted into the disc under the control of the image intensifier, which allows the neurosurgeon to precisely control the direction and depth of needle insertion, and also practically reduces the likelihood of injury to nerves or large blood vessels to 0.
Using cold plasma, radio waves, thermal laser energy or liquid pressure (during hydroplasty), part of the nucleus pulposus is destroyed. The volume of intervention is clearly controlled by the surgeon. Once the desired effect is achieved, the cannula is removed, and the remaining postoperative wound does not even require sutures. It is covered with a sterile bandage, and within a few hours the patient can leave the clinic and return to daily activities.
But nucleoplasty and hydroplasty are effective only for hernia sizes up to 0.7 cm. In other cases, other methods are used:
- Microdiscectomy – involves removing the hernia through an incision of about 3 cm in the projection of the affected disc. Special miniature instruments are used to perform the operation. Microdiscectomy allows you to remove a hernia of almost any size and location, while the small size of the incision ensures ease of rehabilitation and speed of recovery.
- Endoscopic surgery is a gentle method of surgical treatment of intervertebral hernia, which involves removing it with special instruments that are inserted into the patient’s body through punctures up to 1 cm in diameter. Through endoscopic surgery it is also possible to remove almost any hernia, but if its location is complex, the technique is powerless.
Surgery for sciatica caused by spondylolisthesis
Surgical treatment is indicated for spondylolisthesis, accompanied by a displacement of the vertebra by more than 50% relative to the normal axis. It can be carried out in two ways, and the choice of a particular one is based on the results of the MRI. But with sciatica, stabilization of a displaced vertebra in a normal position is permissible only after removal of the anatomical formation that provokes compression of the nerve and the development of neurological symptoms of sciatica.
In almost all cases, stabilization of a displaced vertebra is carried out using a special plate, which is fixed to a healthy and slipping vertebra using screws. This eliminates the possibility of it being re-displaced from its anatomically correct position. But first it is necessary to carry out:
- Discectomy – removal of the intervertebral disc is indicated if, against the background of spondylolisthesis, an intervertebral hernia forms and impinges on the spinal root. If complete removal of the disc is required, it is replaced with an endoprosthesis or a graft of the patient's own bone. The first option is preferable, since modern endoprostheses are in no way inferior in functionality to natural intervertebral discs.
- Foraminotomy - is performed when a nerve is pinched in the foraminal openings of the spine as a result of a decrease in their size due to the proliferation of bone tissue or other reasons.
- Laminectomy is a radical operation used only in extreme cases when spondylolisthesis has led to stenosis of the spinal canal. During a laminectomy, both individual anatomical structures and entire vertebrae can be removed. In the latter case, the removed vertebra is replaced with appropriate implants.
Surgery for sciatica caused by scoliosis
Scoliotic deformity of the spine often provokes pinching of various nerves and the development of sciatica in particular. Therefore, if the deformity cannot be corrected conservatively, surgical intervention is resorted to.
There are several types of operations performed for scoliosis. The specific tactics for restoring the correct axis of the spine are determined individually, but in all cases special metal structures are used that fix the vertebrae in the correct position. Sometimes they involve correcting the position of the vertebrae after surgery with gradual tightening of the screws to form a more correct axis of the spine.
But if previously all operations to correct scoliosis involved long incisions along almost the entire length of the spine, today this is possible even in a minimally invasive way. As a result of eliminating spinal deformity, the nerves are freed, which helps eliminate the causes of sciatica and progressively improve the patient’s condition.
Causes of pain in calves
The causes of pain in the calves may lie in muscle fatigue, but often such a clinical manifestation can signal pathologies of arterial vessels, veins, tissues, surrounding muscles and the spine. If you constantly have pain in the calf of your left or right leg, or regularly experience leg cramps, you should seek medical help, as the consequences can be unpredictable.
Vein diseases
A pain symptom in venous diseases is a valuable signal, since it is thanks to it that serious pathologies that require immediate medical attention can be identified:
- Varicose veins - characterized by persistent pain in the calf muscles, which is felt in the afternoon and is accompanied by swelling of the ankles. This disease can also be determined visually, since visible dilated veins appear on the lower extremities. The reason that the calf of the right or left leg hurts, in this case, is the development of swelling of the leg, as a result of which compression of the nerve endings occurs;
- Acute venous thrombosis requires immediate treatment, since blood clots that form in the deep veins can enter the vessels of the pulmonary circulation and clog the arteries, leading to pulmonary embolism, which is often fatal. Pain in the affected calf covers the inner surface of the lower leg and spreads up to the thigh and down to the foot. They are accompanied by swelling of the lower leg, a feeling of heaviness in the legs and increased pain when trying to bend the foot.
More about vein thrombosis
Arterial diseases
Arterial diseases cause insufficient supply of oxygen and nutrients to tissues, which leads to their destruction. The pain in this case is caused by ischemia (lack of blood supply) and is of a different nature for different diseases:
- Acute form of obstruction of arterial vessels - characterized by acute pain with a burning sensation, which is accompanied by swelling of the affected leg and its coldness;
- Chronic arterial insufficiency is characterized by two types of pain: attacks during acute ischemia and constant pain due to chronic insufficiency of blood supply. Both types of pain can be accompanied by cramps, muscle atrophy, ulcers and gangrene.
Muscle diseases
Muscle tissue lesions of various etiologies can also cause pain in the calves:
- Inflammatory processes of the calf muscles (myositis) - characterized by nagging, aching painful sensations that do not stop or occur in attacks and become more pronounced with movements;
- Parasitic diseases (in particular, trichinosis) are characterized by muscle pain, which is accompanied by swelling of the face, fever, nausea, vomiting, and diarrhea.
More about myositis
Nerve fiber lesions
One of the symptoms of neuritis and polyneuritis is severe nagging pain, which occurs in attacks and can spread along the affected nerve. This manifestation may be caused by compression of the nerve roots. Often, his companions are:
- trophic disorders in the innervated (i.e., organs and tissues supplied by nerves) area;
- feeling of numbness, tingling or pins and needles;
- motor disorders in the innervated area;
- decreased sensitivity.
Other reasons
Pain in the calves may occur due to damage to adjacent tissues:
- osteomyelitis of the tibia;
- diseases of the knee joint;
- ankle joint diseases;
- skin inflammation.
Referred pain in the calves of the lower extremities is one of the symptoms of osteochondrosis of the lumbar spine.
Prevention of sciatica
In fact, avoiding the development of sciatica is much easier than then suffering from unbearable pain and undergoing treatment. To do this, as well as to avoid relapse of the disease after successful treatment, it is enough to lead a healthy lifestyle and follow simple rules:
- maintain the level of physical activity at an optimal level (daily walking, morning exercises and visits to the pool 2-3 times a week are enough to maintain normal muscle tone and improve the condition of the whole body);
- take breaks every hour when working sedentarily and use an orthopedic corset if you need to sit for a long time;
- purchase an orthopedic mattress that will not sag under body weight;
- observe the correct technique for lifting heavy objects: with your knees bent and your back straight;
- refuse strong physical activity;
- normalize your diet and avoid overeating.
Thus, it is possible to cope with sciatica, improve the quality of life and avoid the risk of losing the ability to self-care at almost any stage of development. But it is much easier to do this when the first symptoms appear. Otherwise, the likelihood of needing surgery is very high.