Literally minutes count
“The vascular departments use the latest technologies that make it possible to most effectively help a patient with a stroke.
These include emergency operations and thrombolytic therapy, which restores blood supply to the brain,” said Galina Ivanova, chief specialist in medical rehabilitation of the Russian Ministry of Health. — Thrombolysis is included in the procedure for providing care to patients with cerebrovascular accidents. Moreover, innovative thrombolytic drugs, which until recently were purchased exclusively abroad, have begun to be produced in our country.” We are talking about a joint Russian-German project to localize their production at an already existing production site. However, it makes sense to use such methods only if the patient sees a specialist within the first 4.5 hours after the impact. “The prognosis of a patient’s condition after an ischemic stroke depends on the time of thrombolysis literally minute by minute: if you manage it within the first 1.5 hours, one patient in 4-5 has a chance to fully recover, if within three hours, then one in 9, and if in within 4.5 hours, then one out of 14,” noted Galina Ivanova.
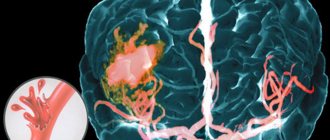
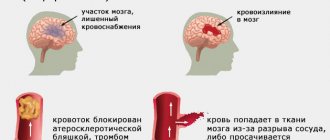
Ischemic stroke
Occurs in 80–85% of cases. It develops when the arteries supplying the brain are narrowed or blocked by atherosclerotic plaque or blood clot. Due to a lack of oxygen and nutrients, brain cells die. Most often occurs in people over 60 years of age. In most cases, it develops at night without loss of consciousness.
Atherothrombotic stroke is the formation of a blood clot at the site of an atherosclerotic plaque.
Embolic stroke is a blockage of small blood vessels by emboli: droplets of fat, blood clots, air bubbles carried by the blood flow from larger vessels.
Lacunar stroke is a narrowing of small arteries as a result of atherosclerosis, developing against the background of arterial hypertension.
Hemodynamic stroke is a combination of two factors: a sharp decrease in blood pressure during heart failure and narrowing of one of the large vessels of the brain.
Hemorheological blockage of cerebral vessels occurs as a result of increased blood clotting or increased ability of platelets to stick together.
At first I had a headache. Moscow hospitals teach how to avoid strokes Read more
It won't go away on its own
However, the number of patients admitted to hospital on time is still low. It seems that the ambulance on such calls arrives much faster, and they take the patient not to the nearest hospital, but to where there is a specialized department. But, unfortunately, there are many cases when the victims themselves and their relatives put off calling an ambulance, in the hope that “it will go away on its own.” Actually, the project “Stroke in Lens” is intended to once again remind us all of the threat of vascular catastrophe, which can happen at any time even in apparently healthy people.
“It is necessary that as many citizens of our country as possible know the first external signs of a stroke - a skewed smile, incoherent speech, the inability to raise both arms,” Ivanova said. “And, faced with their manifestations in one of our relatives, acquaintances, or just passers-by, we called an ambulance immediately.”
Why can't we recognize a stroke in time?
— What determines the severity of these consequences?
— Each case is individual. It all depends on the degree of damage to the vessel by atherosclerotic plaque, namely, the degree of narrowing of its lumen. As a rule, this depends on age, the presence of severe concomitant diseases, the location of neurological damage and partly on treatment.
Example: the day before yesterday we removed a large hematoma, the formation of which was caused by taking an anticoagulant - warfarin (reduces blood clotting to prevent the formation of blood clots). The patient was taking this drug because he had heart surgery a month ago. Due to decreased blood clotting, a cerebral hemorrhage occurred. The hemorrhage was huge in the frontal lobe, it led to disturbances in speech, psyche, and movements of the right arm and leg. After the operation, everything was partially restored, and this is not the limit - recovery continues.
— How often do you have to resort to surgical treatment and how important is it for a positive outcome of the disease?
— A rupture of an aneurysm requires quick decisions and emergency measures. For hemorrhages associated with hypertension, atherosclerosis - the so-called hypertensive hemorrhages, patients need surgery in approximately 10% of cases, in other situations they should be treated conservatively - this is drug treatment and rehabilitation.
Urgent measures in case of vessel rupture are necessary to prevent repeated hemorrhages - they occur in 60% of cases in the first three weeks after a vascular accident and in 20-30% of cases lead to death.
— Why is surgery not always required?
- With a hemorrhagic stroke, the hemorrhage may be small, or it may be located in functionally significant parts of the brain, penetration into which is harmful - causing even greater damage than the stroke itself. For these patients, the results of surgical treatment are poor, even worse than the natural history of the disease.
In an ischemic stroke (cardioembolic), a thrombus breaks away from the wall of the heart cavity and enters one of the brain vessels through the bloodstream. Modern surgery makes it possible to remove this thrombus from the vessels using x-ray surgical methods. If this is technically possible and the brain damage is minor, surgery can achieve very good results in the patient's recovery. But we don’t always have a chance to use existing technologies: it makes sense to carry out such an operation very quickly - minutes and hours count (up to 3-6 hours). That is, the time of delivery of the patient to the clinic, which has the capabilities for such interventions (cerebral coronary angiography, computed tomography and angiography), plays an important role.
Over the course of five months, we performed only 10 such operations, all of them were successful.
- Why so few?
— Most often, the reason is the delay in seeking help, and as a result, the late delivery of the patient. Someone puts off calling an ambulance with the confidence that it will “go away on its own” and is not aware that these are symptoms of a stroke. For some, a vascular accident immediately left them in a serious condition, and there was no one nearby who could call an ambulance. And it’s very difficult when a disaster happens in a dream. In addition, when the ambulance was called, it could not get there quickly in our traffic jams. Rarely, of course, but it happens that the ambulance team makes the wrong decision, or in the emergency room of a medical institution, doctors work slowly and underestimate the situation. The result is that precious time is lost to perform life-saving surgery.
About 10 years ago we were in one of the Israeli clinics and they showed us a patient who underwent thromboextraction (removal of a blood clot) of the cerebral arteries and thereby saved him from death. They were very proud of him. This can be done here too - technology is available to everyone and at any time of the day or night - again, when everything is done on time. The time factor is a very important factor and must be strictly observed. The only shame is that we cannot always take advantage of this opportunity, and for a trivial reason - due to the patient or those around him not knowing the signs of a stroke, which everyone should be able to recognize.
— It turns out that the time of calling an ambulance and delivery to the hospital is important in case of ischemic stroke, but in case of hemorrhagic stroke it is not always of great importance for the outcome of the disease?
— In case of hemorrhagic stroke (cerebral hemorrhage), if there is no compression of the brain and large hemorrhage, speed (hours and minutes) does not play a big role. In the event of an ischemic stroke, when a vessel becomes blocked and the blood supply to an area of the brain sharply decreases or stops altogether, it is necessary to remove the blood clot from the vessel as quickly as possible. And here the speed of delivery of the patient to the hospital and the start time of the manipulations are very important. They determine the prognosis for the patient’s future, because time depends on how many brain cells have time to die. Neither those around you nor the emergency doctors can always understand “on the fly” without the necessary examination whether it is a hemorrhagic stroke or an ischemic one, so as soon as it becomes clear that the patient is having a stroke, one must always hurry. In a hospital, first of all, you need to make an accurate diagnosis - to understand which parts of the brain are damaged and why. To do this, it is necessary to urgently carry out neuroimaging - computed tomography, magnetic resonance imaging or cerebral angiography - according to indications determined only by a doctor. A decision is then made quickly on the appropriate treatment modality and the patient is taken to the operating room.
We in the neurosurgery department deal with this all the time, and sometimes we do not immediately determine what kind of stroke the admitted patient has, or whether he has one at all. Often a patient is brought in with a preliminary diagnosis of “ischemic stroke”; they are rushed because the blood clot needs to be removed urgently, but this is a hemorrhagic stroke and surgery is not required. Only after the necessary examination can the necessary measures be taken. And for any stroke, including hemorrhagic, the sooner you start treating, the better. And many have a chance of recovery, although previously such patients, especially the severe ones, were left at home and told: “An elderly person, unconscious, not transportable.” Now I can responsibly declare that many people have a chance to maintain an active life, we use it and try to ensure that the majority of our patients have it.
— You say that specialists may have doubts about a patient with symptoms of a stroke: “whether it exists at all.” Why?
— Some elderly patients with severe and long-term damage to cerebral vessels, chronic cerebral insufficiency, and widespread atherosclerosis may have manifestations similar to strokes. Some of them can be helped, or rather, improved quality of life, if they are operated on. It happens that patients with other diseases present with stroke manifestations - with a brain tumor (metastases or primary tumor): they experience weakness in an arm or leg, sudden headaches. We currently have three such patients in our department. Two of them were found to have melanoma metastases in their heads, and we removed them. The third has metastases in the brain and a large kidney tumor. However, benign tumors can also “masquerade” as a stroke.
That’s why we say that the acute onset of neurological symptoms requires urgent medical attention and a quick diagnosis. A stroke or any other problem requires immediate diagnosis and equally prompt medical care.
© DoctorPeter
Hemorrhagic stroke
Occurs in 10–15% of cases. It occurs as a result of a rupture of a vessel: blood under high pressure comes out of the damaged vessel, pushes apart the brain tissue and forms a hematoma.
Intracerebral hemorrhage . Hemorrhage into the substance of the brain, into the brain itself. The mortality rate from intracerebral hemorrhages reaches 40%. The main cause of this type of hemorrhage is hypertension.
Subarachnoid hemorrhage. In this type of hemorrhagic stroke, aneurysms rupture. The blood enters the area around the brain, which is filled with a special protective fluid. The cause may also be traumatic brain injury.
Complications: partial or complete paralysis, impaired speech, writing, memory disorders and other functions of higher nervous activity, coma, high mortality.
It won’t go away on its own, get help immediately. Debunking myths about stroke Read more
Symptoms of a stroke
Stroke most often occurs early in the morning or late at night. The following signs indicate a stroke:
► sudden numbness or weakness of the muscles of the face, arms or legs, up to paralysis. Most often it affects only the left or right side of the body. The smile is skewed, the protruding tongue is curved or tilts to the side; ► Impaired speech and pronunciation of words. When trying to pronounce even a simple sentence, diction is disrupted and phrases become confused; ► decreased vision, most often only in one eye, and visible pulsation of the carotid artery on the affected side, strabismus, double vision; ► sudden loss of coordination of movements, unsteadiness of gait; ► sudden sharp and unexplained headache; ► nausea, vomiting, dizziness; ► loss of orientation in time and space.
Before the ambulance arrives
Emergency assistance should be provided within a maximum of 4 hours from the onset of the attack. When calling emergency services, describe your symptoms accurately so that a specialized neurological team can attend. While waiting for the service to arrive, it is necessary to lay the patient down, raising his head 30 degrees above his body, loosen any compressive clothing, and open a window or vent. Measure your blood pressure. If it is high, give the person a medicine to lower the pressure and/or apply a heating pad or hot water bottle to the feet. In case of nausea and vomiting, place the patient on the right side. Check with the ambulance team whether the hospital where the patient is being hospitalized is equipped with equipment for magnetic resonance imaging or computed tomography.
After a stroke. Artists whose careers were interrupted by serious illness Read more