If the brain dies, this means the onset of biological death. The death of the tissues that make it up is irreversible. Without neuron signals, the body will not be able to maintain heartbeat and breathing.
In the world, it is customary to distinguish several types of death - biological, clinical, brain death.
Clinical death is considered reversible. Degenerative processes begin to occur, from which a person can die, but there is still a chance to restore the vital functions of the body. If the outcome is favorable, you can fully regain your health and continue to live a full life. In this case, necrosis of tissues and organs does not occur.
Biological death is associated with the death of all organs and systems. This process is already irreversible, as neuronal damage and necrosis are observed. Vital functions are completely lost, death occurs.
What are the criteria for brain death? It is associated with the death of neurons. If the brain dies, this process is also irreversible. The body is no longer able to maintain vital functions; the respiratory and cardiovascular systems do not work. This is analogous to biological death. When brain death occurs, necrosis of its tissues is necessarily observed.
Sometimes brain decortication is performed - partial surgical removal of the cortex. Such a serious operation is performed only for special indications.
Causes
Brain death can be caused by different reasons, but they trigger the development of the same pathological processes. Blood circulation is impaired, and this dysfunction is persistent. This provokes acute oxygen starvation, which causes metabolic products to stagnate in the tissues. Irreversible brain damage develops.
The main reasons are as follows:
- diseases, including inflammatory processes in brain tissue;
- injuries;
- circulatory disorders (hemorrhagic or ischemic stroke);
- multiple organ failure;
- poisoning (alcohol, lithium, drugs);
- tumor (cancer causes numerous tissue destructions);
- heart diseases, etc.
The phenomenon of vascular occlusion is extremely dangerous. At the same time, their patency is impaired, and oxygen starvation of the tissues occurs. Occlusion of arteries and veins that lead to the brain is especially dangerous. Often, pathological anatomy of the deceased reveals complete blockage of blood vessels. This can be a consequence of injury, disease and causes damage to neurons.
The brain stem may be damaged primarily or secondary. With a primary lesion, direct damage occurs (if there is a fracture of the base of the skull, the functions of the trunk itself are impaired). In case of secondary damage, the trunk suffers due to the resulting edema and dislocation syndrome. With swelling, the tissue begins to protrude strongly through the opening of the back of the head, due to which the trunk is excessively compressed, blood circulation stops and necrosis begins. This is why protecting the brain from swelling is so important.
All of the above reasons are considered extreme; they have an extremely negative effect on neurons. The brain stem and its cortex are primarily affected. The task of the trunk area is to maintain cardiac activity, breathing, control blood pressure, and the cortex is responsible for thought processes, consciousness, etc.
Cardiac arrest does not immediately lead to brain death, but everything happens very quickly. A person without blood circulation can live only a few minutes. 3 minutes without blood supply can lead to irreversible death of neurons, resulting in coma. If the cerebral cortex has died, vital functions will be lost and death can occur almost immediately.
The time that the body can survive without cardiac activity is influenced by a whole range of factors:
- age;
- general condition of the body;
- presence of diseases;
- the reason that caused this condition;
- ambient temperature, etc.
After just three minutes of oxygen starvation, neurons begin to die. This is an irreversible process, since dead tissue is not restored. In a healthy young person, brain death may slow down slightly. If the ambient temperature is low, the brain will die more slowly. If resuscitation is performed correctly at this time, the person can be brought back to life.
The consequences of circulatory arrest can be unpredictable. Sometimes a person wakes up from a coma, blood supply to the brain is restored, but it turns out that a significant part of the neurons have already died. If the brain dies, but the heart works, it will no longer be possible to return the victim to normal life. He can only exist, and is not even able to breathe on his own.
Symptoms
The following symptoms indicate brain death:
- there is no consciousness, and this process is persistent;
- there are no reactions to tingling, stroking, handling, no tactile sensitivity;
- no movement of the eyeballs;
- the heart has stopped, as evidenced by a straight line on the ECG;
- there is urinary and fecal incontinence;
- breathing is impaired, the chest does not rise.
Determining whether a patient has died is an extremely important task. Doctors do not immediately diagnose death. Even if all of the listed signs are detected, the person is monitored in the hospital for up to 12 hours. Sometimes, although rarely, signs of brain activity may appear. If during this time the patient does not react in any way, there are no trunk reflexes, then biological death can be stated.
It is important how the brain dies, what triggered the death of neurons. If poisoning has led to such serious consequences, the patient should be monitored for at least a day. If the cause is TBI, the observation time is reduced to 6 hours. The specific decision must be made by the neurosurgeon. It is important that the doctor monitors the patient from the onset of this condition, then he will have a complete picture of events that will allow him to make the right decision.
The onset of biological death is determined exclusively by a neurologist. It is based on subjective and objective criteria. If signs of brain death are clearly identified, the person must be disconnected from life support. This difficult decision is especially difficult to make if the disaster happened suddenly. Often relatives are literally horrified by such a message. If a person is sick for a long time, his loved ones eventually become at least a little accustomed to the idea that their loved one will be gone. In any case, this decision is very difficult.
Observation and proof of irreversibility of pathology
In the absence of breathing, we can talk about the loss of vital activity of the entire brain; the doctor can only establish the fact that this process is completely irreversible. The irreversibility of brain disorders can be judged after a certain period of observation, depending on the cause of the pathology that caused the death of the nervous tissue.
If primary brain damage has occurred, then to establish brain death, the duration of observation must be at least 6 hours from the moment when the symptoms of the pathology were first recorded. After this period, a repeat neurological examination is performed, and the apnea test is no longer necessary.
Previously, it was recommended to observe the patient for a minimum of 12 hours, but now in most countries of the world the time has been reduced to 6 hours, since this time interval is considered sufficient to diagnose brain death. In addition, reducing observation time plays an important role when planning organ transplantation from a brain-dead patient.
In case of secondary damage to the nervous tissue, a longer observation is required to make a diagnosis of brain death - at least a day from the moment of the initial symptoms of the pathology. If there is reason to suspect poisoning, the time is increased to 72 hours, during which neurological monitoring is carried out every 2 hours. If the results are negative, brain death is declared after 72 hours.
Based on the stated diagnostic criteria, during observation of the patient, undoubted signs of brain death are recorded - the absence of reflex and brainstem activity, a positive apneic test. These parameters are considered absolutely indicative and reliable, not requiring additional examination, and therefore are used by doctors all over the world.
Diagnostics
When diagnosing, the doctor must collect anamnesis. He must find out how long ago the patient fell into such a dangerous state, under what conditions he lost consciousness, and whether he had speech or motor activity. It is important to know what event preceded the loss of consciousness. An examination is carried out by a neurologist, he necessarily assesses the patient’s level of consciousness and checks his reflexes.
It is extremely important that the doctor excludes all those factors that can cause simulated brain death. It is sometimes caused by severe poisoning, including drugs. For this reason, a toxicological analysis is prescribed. It will help detect toxins or drugs that mimic the appearance of death.
Body temperature must be measured. If the temperature is below 32.2°C, it may distort the picture and show a false death. In this case, the person may be alive, but tests will show the opposite, since physiological processes literally freeze from the cold.
A blood test is prescribed that will help determine whether the metabolism is disturbed, whether there is hormonal dysfunction, and at what level the glucose levels are.
To correctly diagnose brain death, inpatients resort to instrumental research:
- encephalogram (EEG);
- contrast study of cerebral vessels;
- test with irritation of the eardrums (ice water is dripped onto them through the ear canal);
- apneic oxygenation test.
Oxygen starvation is extremely destructive for neurons, even if it is not long-term. Literally after a few minutes of complete lack of oxygen supply, tissues begin to die. The electroencephalogram in this case will show a zero line. This means that there is no brain activity at all.
Encephalography examines brain activity. In this case, the device registers biocurrents, their work is reproduced on paper in the form of curves.
The diagnostic protocol also includes the study of cerebral vessels using a contrast agent. It cannot always be accomplished, as there may be financial restrictions, and sometimes there is simply no equipment. The essence of the test is that a contrast agent is injected, which enters the brain vessels through the bloodstream and identifies possible areas of necrosis. If the brain is dead, the substance does not enter its vessels. This is one hundred percent confirmation of death.
Apneic oxygenation involves temporarily removing the patient from a ventilator. The goal is to observe whether spontaneous respiratory movements have appeared. The monitor monitors the level of carbon dioxide in the blood. It is carbon dioxide that stimulates the body to produce breathing movements. If after 8-10 minutes breathing does not appear, and the level of CO2 in the blood jumps by 20 mm Hg. Art. higher than the original, we can definitely talk about death.
Clinical data analysis
The next stage in diagnosing brain death, which begins after establishing the causes and excluding other pathologies, will be the assessment of clinical data - coma, absence of brainstem reflexes, inability to spontaneously breathe (apnea).
Coma is a complete absence of consciousness. According to modern concepts, it is always accompanied by total atony of the muscular system. In a coma, the patient does not react to external stimuli, does not feel pain, changes in the temperature of surrounding objects, or touch.
Brainstem reflexes are determined in all patients without exception with possible brain death, while the following signs are always taken into account to verify the diagnosis:
- There is no response to sufficiently intense pain effects in the areas of exit of the branches of the trigeminal nerve or the absence of other reflexes, the arcs of which close above the cervical part of the spinal cord;
- The eyes do not move, the pupils do not react to a light stimulus (when it is clearly established that there is no effect of medications that dilate them);
- Corneal, oculovestibular, tracheal, pharyngeal and oculocephalic reflexes are not detected.
The absence of oculocephalic reflexes is determined by turning the patient's head to the sides with raised eyelids: if the eyes remain motionless, then there are no reflexes. This symptom is not assessed for cervical spine injuries.
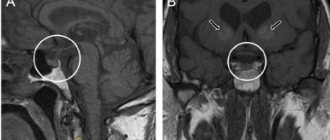
checking oculocephalic reflexes
connection of oculocephalic and oculovestibular reflexes with brain stem vitality
To determine oculovestibular reflexes, the patient's head is raised, and cold water is pumped into the ear canals using a thin catheter. If the brain stem is active, the eyeballs will deviate to the sides. This symptom is not indicative of injury to the eardrums with a violation of their integrity. Pharyngeal and tracheal reflexes are checked by displacing the endotracheal tube or inserting a bronchial suction catheter.
One of the most important diagnostic criteria for brain death is the inability to breathe independently (apnea). This indicator is the final one at the stage of clinical assessment of brain functioning and can be determined only after checking all of the above parameters.
To determine whether a patient is able to breathe on his own or not, it is unacceptable to simply disconnect him from the ventilator equipment, since sudden hypoxia will have a detrimental effect on the already suffering brain and myocardium. Disconnection from the equipment is carried out on the basis of an apneic oxygenation test.
An apneic test involves monitoring the gas composition of the blood (the concentration of oxygen and carbon dioxide in it), for which a catheter is installed in the peripheral arteries. Before disconnecting the ventilator, ventilation of the lungs is carried out for a quarter of an hour under conditions of normal CO2 content and high oxygen pressure. After these two rules are observed, the ventilator is turned off, and humidified 100% oxygen is supplied to the trachea through the endotracheal tube.
If spontaneous breathing is possible, then an increase in the level of carbon dioxide in the blood will lead to activation of the stem nerve centers and the appearance of spontaneous respiratory movements. The presence of even minimal breathing serves as a reason to exclude brain death and immediately return to artificial ventilation of the respiratory system. A positive test result, that is, absence of breathing, will indicate irreversible death of the brain stem structures.
If the body is accidentally discovered
If an ambulance team finds a victim without signs of life, doctors have no information how long he remains in this condition. In the absence of cadaveric spots, doctors cannot confirm in the field that biological death has occurred. In this case, resuscitation is mandatory.
Resuscitation measures include artificial ventilation of the lungs and closed heart massage. If there is bleeding, it is important to stop it so the victim does not bleed out. Damage to a large artery or head is extremely dangerous. If resuscitation measures are carried out correctly, a person can be brought back to life.
How to tell your family
Recently, it has become common to resort to the help of a psychologist in such cases. It will help family members come to terms with their loss.
Making a decision to disconnect a patient from life support is extremely difficult even for experienced doctors. Relatives are always unprepared for such a tragic development of events, so they literally lose their minds. Relatives tend to believe that they can still try to do something. They are often asked to wait at least a few days. If there is accurate evidence of brain death, the doctor must find the right words to explain the current situation to the relatives.
According to the rules of bioethics, if brain death is definitely established, the patient should be disconnected from devices that support life processes. There is no point in expecting him to come back to life if all tests have confirmed the absence of neuronal activity. This will be a humane decision.
Relatives should definitely ask what diagnostic research methods were used. The doctor must show a document confirming the established brain death. Only relatives have the right to decide to disconnect the victim from life-sustaining devices. The doctor’s task is not to succumb to emotions, but to make the right decision based on the specific results of the patient’s examination.
It is important to exclude the human factor and rely only on test results.
How long to keep the victim on life support is decided individually in each case. After a person is disconnected from the devices, Lazarus syndrome may occur. It consists in the fact that the deceased experiences individual muscle twitches. The head may turn involuntarily, the person may bend an arm or leg. It even happens that an already dead person arches. This is the result of contraction of the back muscles. It is important that the doctor warns the patient’s relatives in advance that such manifestations are possible. This does not mean that the victim comes to life.
Consequences
Brain death does not always lead to biological death. Sometimes medical intervention can save a life, if such a condition can be called that. In fact, after brain death, only certain vital functions can be maintained. The consequences of total neuronal death are terrible, this is complete dementia. Any vital indicator is so low that the body cannot cope without the support of devices. Such people are no longer able to continue living a full life. They live like plants and can die at any moment.
Even in order to maintain basic vital functions, continuous administration of medications will be required. Without medical equipment, the patient will not be able to breathe, and his heart will not be able to beat.
In the medical literature there are several descriptions of a case of a person returning to life after death. There is some confusion here. Most likely, such patients “resurrected” after clinical death, rather than biological death. This happens quite often. Clinical death can occur with serious damage, and with proper care, body functions are restored.
Even clinical death is not identical to brain death. It is the death of neurons that leads to the most tragic consequences.
Assessment of causes of brain death
A doctor has the right to begin diagnosing biological brain death only when the causative factors and mechanisms of changes in nervous tissue are precisely known. The causes of irreversible brain disorders can be primary, caused by direct damage to the organ, and secondary.
Primary brain damage leading to brain death is provoked by:
- Severe traumatic brain injuries;
- Hemorrhages, both traumatic and spontaneous;
- Cerebral infarctions of any nature (atherosclerosis, thromboembolism);
- Oncological diseases;
- Acute hydrocephalus, edema;
- Previous surgical operations inside the skull.
Secondary irreversible damage occurs due to pathology of other organs and systems - cardiac arrest, shock, severe hypoxia against the background of systemic circulatory disorders, severe infectious processes, etc.
An important diagnostic step is the exclusion of all other pathological conditions that could manifest symptoms similar to brain death, but which, nevertheless, are potentially reversible with proper treatment. Thus, the diagnosis of brain death should not even be assumed until a specialist makes sure that there are no influences such as:
- Intoxication, drug poisoning;
- Hypothermia;
- Hypovolemic shock due to blood loss, dehydration;
- Coma of any origin;
- The effect of muscle relaxants, anesthetics.
In other words, an indispensable condition when diagnosing brain death will be the search for evidence that the symptoms are not caused by drugs that depress the nervous tissue, poisoning, metabolic disorders, or infections. In case of intoxication, appropriate treatment is carried out, but until its signs are eliminated, a conclusion about brain death is not considered. If all possible causes for the lack of brain functioning are excluded, then the question of its death will be raised.
When monitoring patients with brain disorders potentially associated with other causes, the rectal temperature is determined, which should not be less than 32 C, the systolic blood pressure is not less than 90 mm Hg. Art., and if it is lower, vasopressors are administered intravenously to maintain hemodynamics.
Reanimation
The consequences of brain death are irreversible. Just because a person is unconscious does not mean that he needs to perform resuscitation measures (ventilation, cardiac massage).
Cardiac massage is strictly contraindicated if the victim’s heart is beating, even abnormally. In this case, massage can, on the contrary, interfere with the correct contraction of the heart muscles.
Mouth-to-mouth or mouth-to-nose breathing, as well as chest compressions, are performed only if there is no heartbeat. Such events can save a person's life. If you ensure the supply of oxygen to the body and improve blood circulation, irreversible necrotic changes will not occur. Body functions can be completely restored.
If a pregnant woman is injured, it is important to monitor not only her vital signs, but also the condition of the fetus. The patient must be taken to the hospital as quickly as possible, since the child may die due to injury and stress.
It is extremely important to thoroughly master resuscitation techniques. Any of us can master them and, if necessary, save a person’s life.
Forecasts
Clinical death does not always mean that the patient will definitely die. Sometimes doctors manage to bring a person out of a state of clinical death. The prognosis will be influenced by what circumstance led to such a condition and what resuscitation measures were taken. The main condition is to restore blood circulation in the first 3-5 minutes. Sometimes resuscitation is carried out for up to 20-40 minutes.
Even if partial extinction and death of neurons has occurred, the functions of the medulla can be restored. If biological death or brain death is established, it is impossible to bring the patient back to life, you need to come to terms with this.
The peculiarity of the human brain is that it strives to preserve its functions by any means. If some neurons die, their tasks can be redistributed to other zones. Patients who have suffered a stroke, ischemia, and even serious TBI often return to a full life.
Both scary and awkward
As the medical encyclopedia says, death is the irreversible cessation of the body’s vital activity, the natural and inevitable final stage of its individual existence.
In warm-blooded animals and humans, it is primarily associated with a complete stop of breathing and blood circulation. In fact, death can consist of several stages and terminal conditions. And the signs of biological death (when all physiological processes in cells and tissues are stopped) were constantly refined with the development of medicine. This question is vital in the truest sense of the word. And the point is not that a person can be buried alive (in our time this is difficult to imagine, but in the past it happened regularly) - the exact confirmation of death determines when resuscitation measures can be stopped, as well as organs removed for further transplantation. That is, saving someone's life.
Imaginary death: what is lethargic sleep Read more
What happens to the body when all vital processes stop? The brain cells are the first to die. They are most sensitive to lack of oxygen. However, some nerve cells can live so long that scientists are not entirely sure whether such a person should be considered dead? After all, he seems to continue to perceive something and (who knows!), perhaps, think!
Swedish scientists from the Karolinska Institute conducted research and came to the conclusion: the brain activity of the deceased fluctuates greatly. Either it is near zero, which indicates death has occurred, then it suddenly rises to a value corresponding to the state of wakefulness. And then it falls again. What happens in the brain of the deceased remains unclear. It is possible that he has some thoughts and feelings even after his heart has stopped beating.
Scientists suggest that the nerve cells of the brain at this moment emit the last impulse. This also explains the phenomenon of experiences in a state of clinical death - the feeling of flight, light at the end of the tunnel, meeting with a higher being, etc. “It is unlikely that a person is conscious during such brain activity,” says Lars Ohlsson, a researcher from the Karolinska Institute. “The only people who have come close and can say anything about it are those who have had near-death experiences.” And according to believers, a flash of brain activity corresponds to the moment when the soul of the deceased leaves the body.
Article on the topic
Locked brain. Do people in a coma hear everything, think and can communicate? If it is not possible to ask the deceased what he is thinking about, then seeing his movements and hearing sounds is quite possible. The fact is that after death the body twitches for a couple of seconds and spasms occur in it. The muscles then relax, returning to their original state, and this may be perceived as moving or twitching of the limbs. There have been cases where a person has given up the ghost and his chest moves, giving the impression that he is still breathing. The reason is that after death, the nervous system sends signals to the spinal cord “by inertia” for some time.
Sometimes the dead make strange sounds, which, of course, horrifies the relatives and those gathered to see him off on his last journey. These sounds sound like a groan, a whistle, a sigh, or a strangled cry. There is no mysticism here: the body of every person is filled with liquids and gases. Once the body begins to decompose, additional gases are created that need an outlet. They find it through the trachea. Hence the sounds.
There is even “inappropriate behavior” on the part of deceased men, when those present notice they have an erection. The awkwardness and bewilderment are understandable, but so is the phenomenon itself. After the heart stops, blood can move to the pelvic area and cause temporary swelling of the penis.
How is lethargic sleep recognized and distinguished from death? More details