Meniere's disease is a disease of the inner ear of unknown etiology. During an attack of the disease, tinnitus, dizziness and hearing loss are observed. The duration of vestibular crises ranges from several minutes to several days and may be accompanied by nausea, vomiting, increased sweating and imbalance. The prognosis is favorable, but repeated attacks are painful for the patient and lead to decreased ability to work.
The main goal of treatment for Meniere's disease is to relieve and prevent attacks. If conservative therapy is ineffective, surgical intervention is indicated for patients.
Anatomy and physiology of the inner ear
Anatomically, the hearing organ consists of three parts:
- The outer ear includes the external auditory canal and the pinna;
- The middle consists of the auditory ossicles, the Eustachian tube and the tympanic cavity;
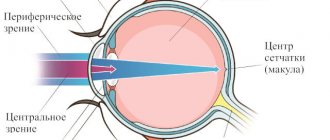
- The inner ear includes the sensory apparatus of the organ of hearing and balance. The vestibular analyzer consists of the vestibule of the cochlea and the semicircular canals. The auditory analyzer is located in the cochlea. The cochlea is a bony, spirally convoluted canal, tapering from the base to the apex. Inside the bone canal there is a membranous labyrinth, completely repeating the structure of the first. The membranous labyrinth is filled with endolymph and bone perilymph. Perilymph is similar in composition to cerebrospinal fluid, as it communicates with the subarachnoid space of the brain. The cochlea contains three sections: the vestibular, middle and tympanic scala. The vestibular septum is separated from the scala mediali by Reisner's septum, and the scala mediali is separated from the scala tympanum by the basilar membrane. The birth of a nerve impulse is ensured by the activity of the cells of the organ of Corti. This is an accumulation of neuroepithelial elements on the basilar membrane. Cells of the organ of Corti perceive and transform auditory stimuli into a signal for the brain.
Sound is produced by the passage of air through the auricle to the eardrum, which causes the auditory ossicles to move. The vibrations of the ossicles cause the movement of the peri, then the endolymph. This in turn excites the auditory receptors and a nerve impulse is born that goes to the hearing center of the cerebral cortex.
What happens in Meniere's disease?
It is believed that the appearance of symptoms of Meniere's disease is associated with an increase in fluid pressure (endolymph) in the cavities of the inner ear, which may occur due to its increased production or malabsorption.
There are several possible causes of the development of Meniere's disease:
- Impaired circulation of fluid in the cavities of the inner ear due to injury or anatomical disorders
- Viral infection, as well as an abnormal response of the immune system to it
- Allergy
- Genetic predisposition
- Cervical osteochondrosis
- Head injury
- Migraine
Causes
Enlarged endolymph can be caused by:
- congenital anomalies: absence of the vein of the peri-vestibular canaliculus, underdevelopment of the cochlea;
- hereditary predisposition;
- endocrine disorders, especially adrenal and thyroid disorders;
- atherosclerosis, spasm of the coronary arteries;
- degenerative changes and spinal injuries;
- violation of carbohydrate, fat, protein and water-salt metabolism;
- vegetative-vascular dystonia;
- hypercoagulability;
- autoimmune processes;
- hypovitaminosis.
Poisoning with alcohol, drugs and allergies can provoke vestibular crises. The role of cytomegalovirus and herpes simplex virus among the causes of Meniere's disease has now been proven.
Causes of the disease
To date, the exact causes of Meniere's disease remain unclear. There are a number of hypotheses and assumptions that to some extent explain the probable causes of the development of this disease:
- complications of viral infections, as a result of which autoimmune processes develop (immune system mechanisms directed against the cells and tissues of one’s own body);
- hereditary predisposition (a number of researchers note cases of this disease in previous generations in the family history of patients with Meniere's disease);
- vascular diseases in which the outflow of blood from the tissues of the inner ear is impaired, which leads to the accumulation of excess fluid in its cavity;
- metabolic disorders, in particular water-volitional metabolism;
- traumatic injuries of the inner ear;
- diseases of an endocrine nature in which estrogen deficiency is expressed;
- inflammatory and infectious diseases of the inner ear with interrupted or improper treatment, as a result of which negative changes develop in the tissues of the labyrinth;
- allergy.
The causes, symptoms and treatment of Meniere's disease are quite closely related concepts. Treatment of the disease necessarily takes into account the characteristics of the clinical picture, anamnesis and objective diagnostic results, which allow us to assess the severity of the condition.
Classification
Meniere's disease should be distinguished from the syndrome of the same name.
Meniere's syndrome is a concomitant factor of a certain disease; BM represents an independent nosological unit. Meniere's disease, according to ICD-10, corresponds to class H81—vestibular function disorders, code H81.0.
Along the course, endolymphatic hydrops occurs:
- classic, when auditory and vestibular disorders appear simultaneously;
- if the balance is first disturbed - vestibular;
- in the cochlear form, auditory disorders primarily occur.
According to the severity, BM is classified into mild (short attacks with a break of at least a month), moderate (crises up to 6 hours) and severe (exacerbations once a day with loss of ability to work). There are also reversible and irreversible forms of the disease. If reversible, it is possible to restore the functions of the auditory analyzer.
Symptoms
The disease is named after the French physician Prosper Meniere. He was able to prove the connection between hearing impairment and pathology of the hearing system, and not the brain.
Meniere's disease occurs with periods of exacerbations and remissions. The process is often one-sided, with the exception of autoimmune lesions. The primary signs of an attack of endolymphatic hydrops are sudden (labyrinthine attacks) dizziness, tinnitus and gradually increasing hearing loss.
Secondary symptoms of endolymphatic hydrops crisis:
- nausea, vomiting;
- increased sensitivity to loud sounds;
- nystagmus - frequent vibrations of the eyeballs;
- diarrhea;
- frequent urination;
- increased salivation;
- increased sweating;
- blood pressure is usually reduced;
- heaviness, feeling of pressure on the side of the affected ear.
Labyrinth attacks occur suddenly, often at night or during the day. Attacks occur against the background of normal health, but they can be triggered by stress, malnutrition, poisoning, allergic reactions and physical stress. Sometimes patients feel the onset of an attack several hours or even days in advance. Attacks with BM are divided into:
- frequent (1-2 times a day, week, month);
- rare (several times a year);
- occasional (once every couple of years).
Vestibular disorders in peripheral type MD.
This type of imbalance is characterized by systemic vertigo and horizontal nystagmus. Systemic (true) dizziness occurs when the receptors of the balance organ are irritated. For differential diagnosis of the type of dizziness, the Dix-Hallpike test is used. The duration of attacks varies from several hours to several days. After a crisis, in the first 48 hours the patient feels fatigue and decreased ability to work. In severe and moderate forms of the disease, there is no working capacity. During remissions the condition is satisfactory.
Dizziness
The first symptom of a labyrinthine attack is dizziness (vertigo). It is caused by irritation and compression of the vestibular analyzer receptors. Dizziness with MD is characterized by a feeling of rotation of oneself or objects, and imbalance. The symptom is often accompanied by migraine-like headaches. During an attack, patients often cannot stand on their feet and take a horizontal position. For relief, patients close their eyes. Any movements of the head and body cause deterioration of the condition, increased dizziness, nausea and vomiting. An objective sign of exacerbation is nystagmus. It can be observed not only during, but also after the crisis for up to one week. Nystagmus in Meniere's disease can change direction: at the beginning of the attack it is directed towards the diseased ear, and at the end towards the healthy ear. Vertigo can be dangerous and cause injury because it often occurs suddenly without any previous symptoms. To eliminate this symptom, radical measures are often resorted to - removal of the vestibular nerve. In the final stage of the disease, instantaneous falls without dizziness occur (Tumarkin crises).
Hearing loss
During vestibular crises, patients note hearing impairment. Subjectively, the condition is described as congestion, a feeling of fullness or heaviness in the ear. Hearing loss in Meniere's disease is fluctuating. Fluctuating hearing loss is characterized by changes in hearing acuity - a decrease before and during attacks. Some patients experience a decrease in hearing acuity with each attack. Hearing loss is usually unilateral, but as it progresses, a second organ may be affected. This symptom is detected by audiometry. In the first stages of the disease, the perception of low frequencies is impaired. Sensorineural hearing loss increases as degenerative processes of spiral ganglion neurons increase.
Noise in ears
Tinnitus is low or mid-frequency.
It intensifies before and reaches its maximum during attacks. The ringing is sometimes accompanied by pain in the affected ear. Meniere's disease occurs in three stages:
- Initial (reversible) stage. Patients are bothered by rare (several times a year, sometimes every two years) attacks lasting an average of 2 hours. During this period, patients complain of tinnitus, vestibular dizziness, a feeling of fullness and pressure in the ear, nausea and vomiting. Tinnitus is intermittent, intensifies before an attack, and reaches maximum strength during a vestibular crisis. The first stage is characterized by fluctuating hearing loss, when the hearing loss is unstable. Hearing loss may be absent during the first attacks. However, in the future, hearing loss intensifies during the attack and is restored after its end. Sometimes hearing loss disappears immediately after a vestibular crisis and reappears a few days later. At the initial stage, the hearing threshold deteriorates when perceiving sound with low and medium frequencies. Nystagmus is recorded only during attacks and can last for several days.
- The second is the stage of pronounced clinical manifestations. During this period, all the symptoms of Meniere's disease are observed. Attacks are recorded every day or several times a month. Vestibular attacks are accompanied by severe dizziness, vomiting, increased sweating and other autonomic disorders. Tinnitus occurs constantly and may intensify during vestibular attacks. Also, patients are always bothered by a feeling of pressure, ear congestion and hearing loss on the affected side. According to the results of audiometry, hearing loss is usually grade I-III. A dehydration test in the second stage of Meniere's disease shows persistently increased pressure within the labyrinth. On vestibulometry, hyporeflexia of the labyrinth is noted, and during attacks - hyperreflexia.
- The third, final stage, is also called “burnt out”. During this period, dehydration tests do not provide relief from symptoms, and the patient is completely unable to work. Attacks of dizziness become less frequent, and imbalances, on the contrary, become more frequent. Fluctuating hearing loss is replaced by persistent, permanent hearing loss on the affected side, up to complete loss. At the third stage, the disease progresses and the second ear is involved in the pathological process. Vestibulometry displays hypo-, in advanced stages, and areflexia of the labyrinth. With Meniere's disease at the final stage, Tumarkin crises may occur - an instant fall without loss of consciousness. Tumarkin crises appear as a result of damage to the receptors of the vestibular analyzer.
Meniere's disease most often affects people aged 20-50 years. The connection with gender is ambiguous: some authors indicate a more frequent occurrence in women, others in men. Among children, the disease is extremely rare.
Symptoms
The disease is paroxysmal in nature: the symptoms of Meniere's disease periodically intensify, then after some time they disappear, only to return again after a few months, days or hours, often to a stronger degree. The main signs of the disease include:
- congestion of one or both ears, which can reach complete deafness;
- noise, ringing, or discomfort in one or both ears;
- regular attacks of dizziness, which can be so severe that a person cannot stand and falls;
- disturbance of the sense of balance;
- nausea or vomiting during attacks;
- spontaneous nystagmus - involuntary movements of the pupils during attacks;
- increased sweating;
- surges in blood pressure - usually a decrease, but in some patients the pressure may increase;
- uncoordinated muscle contractions;
- loss of coordination of movements;
- decrease in body temperature.
If left untreated, hearing loss and tinnitus worsen over time, then the disease affects both ears, which can lead a person to almost complete hearing loss. Attacks of dizziness often begin suddenly, due to which a person loses the ability to drive a car or other complex equipment - this becomes dangerous for the patient and for others. Periods of exacerbation continue for several weeks, during which attacks may recur several times during the day. Then a remission occurs, lasting several months or years, after which the disease returns. Sometimes attacks go away spontaneously after 7-10 years, but most patients require qualified treatment.
Are you experiencing symptoms of Meniere's disease?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Diagnostics
The diagnosis of Meniere's disease is established taking into account specific symptoms and the results of instrumental studies. The American Academy of Otolaryngologists, based on clinical manifestations, distinguishes three degrees of reliability of BM: possible, probable and definite BM. An important diagnostic criterion is the triad of symptoms:
- dizziness;
- noise in ears;
- hearing loss.
The diagnosis is confirmed by gradual deterioration of hearing and repeated episodes of vestibular attacks.
The following instrumental methods are used to diagnose Meniere's disease:
- Pure-tone threshold audiometry is the main method according to international diagnostic criteria. The result of such a study will be an audiogram, which graphically depicts the function of the hearing organ;
- Otoscopy is performed to exclude middle ear pathology;
- Extratympanic electrocochleography evaluates the performance of the auditory nerve;
- A tuning fork test determines the type of hearing loss. In this case, the hearing loss is of the conductive type.
These methods allow you to analyze the degree of hearing impairment. Audiometry is the main criterion when choosing treatment tactics. To detect endolymphatic hydrops, doctors use electrocochleography and a dehydration test.
Audiogram for Meniere's disease
An audiogram is used to determine the degree of hearing loss. Before the procedure, the doctor examines the ears; if ear plugs are found, they are removed. The patient is put on headphones, and signals of different frequencies are sent via a computer. The subject needs to press the button when he hears the signal. In the initial stages, poor perception of low frequencies is recorded.
Electrocochleography
To perform extratympanic electrocochleography, electrodes are placed on the skin of the auricle or eardrum. The electrodes determine the ability of the auditory nerve to generate nerve impulses after a signal is given.
Dehydration test
Before the test, the patient undergoes threshold pure-tone audiometry. Then osmotic diuretics (furosemide) are administered and audiometry is repeated again every 3 hours, after 24 and 48 hours. The test is positive if there is an improvement in hearing of 10 dB or more after 3-4 hours. During remission of the disease, the study is not very informative.
Multislice computed tomography of the bone labyrinth
MSCT allows you to detect the smallest changes in all organs.
The images visualize pathognomonic processes in the inner ear with BM. To assess disorders of the balance organ, the following studies are used:
- videonystagmography to detect horizontal nystagmus;
- the video impulse test displays the vestibulo-ocular reflex and the presence of asymmetry;
- stabilometry;
- bithermal bitemporal calorization is performed to assess the function of the semicircular canals;
- rotational tests.
Differential diagnosis of Meniere's disease is carried out with the following diseases:
- traumatic brain injuries;
- ischemic attacks. Such attacks last minutes and are observed in elderly people with vascular pathology;
- other vestibulopathies, they can arise as a result of purulent otitis, otosclerosis, labyrinthitis;
- tumors of the cerebellopontine fossa;
- vestibular migraine;
- otosclerosis. The disease is often bilateral, the main symptoms are cochlear;
- benign paroxysmal positional vertigo. The attack is intense and occurs in a certain position of the body;
- osteochondrosis.
To exclude brain tumors, injuries, and anomalies in the structure of the temporal bone, CT and MRI are highly informative.
To choose the right treatment tactics, timely and accurate diagnosis is necessary. At the Yusupov Hospital you can get the necessary examinations and consultation from a highly qualified specialist. The clinic has modern high-quality equipment and diagnostic laboratories.
Make an appointment
Meniere's disease: clinical and diagnostic criteria, treatment tactics
Meniere's disease is a non-suppurative disease of the inner ear, characterized by an increase in the volume of endolymph (labyrinth fluid) and an increase in intralabyrinth pressure, resulting in recurrent attacks of progressive deafness (usually unilateral), tinnitus, systemic vertigo, imbalance and autonomic disorders.
For the first time, a symptom complex characterized by hearing loss, tinnitus and periodic dizziness was described in detail by Prosper Meniere in 1861 in a report “On a special type of severe deafness depending on damage to the inner ear” at a meeting of the French Academy of Medical Sciences. At the same time, this condition was called “Meniere’s disease.” Based on fourteen years of experience in examining patients with a similar symptom complex, the results of autopsies and data from experiments on transection of the semicircular canals in pigeons, published in 1824 by the physiologist Jean Pierre Marie Flourens, P. Meuniere suggested that this disease is associated with the inner ear [1]. Later, in 1938, Hallpike and Cairns proved that the basis of Meniere's disease is endolymphatic hydrops [2].
Meniere's disease affects predominantly Caucasians, regardless of gender. The average age of patients ranges from 20 to 50 years, but the disease can also occur in children. The disease is somewhat more common in people with intellectual work and in residents of large cities.
Despite the undying interest of medical scientists in this problem for many years, the etiology of the disease is not fully understood. There are several theories about the development of Meniere's disease. Thus, according to the anatomical theory, Meniere's disease may be associated with a pathology of the structure of the temporal bone, in particular, with reduced pneumatization of mastoid cells and hypoplasia of the vestibular canal, while the small endolymphatic sac is incorrectly located behind the labyrinth.
According to the genetic theory, the hereditary transmission of Meniere's disease was identified more than half a century ago, and the results of recent studies (M. Verstreken, Belgium) indicate an autosomal dominant type of inheritance. It is believed that the DFNA9 region of the COCH gene plays a special role.
The immunological theory is supported by the detection of immune complexes in the endolymphatic sac in patients with Meniere's disease.
The vascular theory is supported by the frequent combination of Meniere's disease with migraine, which was noticed by P. Meniere himself.
According to the allergic theory, the frequency of allergic reactions in patients with Meniere's disease is higher than in the general population. Thus, of 734 patients with Meniere's disease examined by MJ Derebery (USA), 59% said that they suffered from an established or suspected allergy to airborne agents, and 40% from an established or suspected allergy to food products (while the frequency of allergic reactions of the total US population is approximately 20%).
According to the metabolic theory, in Meniere's disease, potassium retention occurs in the endolymphatic space. This causes potassium intoxication of hair cells and vestibular neuroepithelium, resulting in hearing loss and dizziness. Many authors are inclined to the polyetiology of this disease and identify “causing factors” and “predisposing factors” [3].
The clinical picture of Meniere's disease in the vast majority of cases (80–90%) is characterized by unilateral damage with possible “involvement in the pathological process” of the second labyrinth. In this case, we should talk about “bilateral disease” [4, 5].
Meniere's disease can debut with both vestibular and auditory (hearing loss, ear congestion, tinnitus) symptoms. In the first 2–3 years of the disease, hearing loss can be fluctuating (transient) with almost complete restoration of hearing in the interictal period. Over the years, hearing gradually decreases, up to complete deafness.
Dizziness in Meniere's disease is painful - systemic, accompanied by spontaneous nystagmus, ataxia, coordination disorders, pronounced autonomic manifestations (hypersalivation, hyperhidrosis, blood pressure fluctuations, dyspeptic disorders). The duration of the attack lasts from several minutes to days (status meniericus). The severity of dizziness can also vary: from mild “precursors” to a violent reaction, during which patients take a forced position on their side, corresponding to the sore ear (or the direction of the fast component of spontaneous nystagmus). Ataxia and coordination disorders may persist for several days after the attack. In the first years of the disease (up to 3 years), between attacks, when conducting vestibulometry, experimental vestibular normoreflexia is usually recorded. Later, during the period of remission, vestibular hyporeflexia is recorded on the affected and then on the opposite side. Typically, after 10 years or more, the severity of vestibular manifestations decreases.
In the classic course of Meniere's disease, three stages of the disease are distinguished:
I - the predominant symptom is dizziness, often accompanied by nausea and vomiting. Paleness and sweating may occur. Typically, an attack of dizziness is preceded by a feeling of pressure in the ear or the corresponding half of the head, lasting from 20 minutes to several hours. Between attacks, hearing is normal.
II - sensorineural hearing loss develops with a predominant decrease in sound perception at low frequencies. Attacks of dizziness reach maximum severity with a subsequent tendency to reduce the severity of manifestations.
III - there is a progressive decrease in hearing with the development of bilateral deafness. Episodes of dizziness decrease and then disappear completely; however, ataxia may persist, especially in the dark.
The American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) (1995) defines "obvious" Meniere's disease as follows:
- two or more spontaneous attacks of dizziness lasting 20 minutes or more;
- hearing loss confirmed by audiological tests in at least one case;
- tinnitus or a feeling of fullness in the causative ear;
- other causes are excluded [6].
Diagnosis of the classic form of Meniere's disease is based on characteristic clinical manifestations and audiometric data. Difficulties in making a diagnosis may be due to the fact that many patients whose disease begins with attacks of dizziness cannot clearly describe their complaints. In addition, there are a number of diseases and conditions accompanied by vestibular disorders [7]:
- benign paroxysmal positional vertigo;
- vertebrobasilar insufficiency;
- vestibular neuronitis;
- traumatic brain injury;
- labyrinthine fistula;
- infectious labyrinthitis;
- consequences of otosurgical interventions;
- otosclerosis;
- cerebellopontine tumors;
- multiple sclerosis;
- side effects of medications;
- acute purulent otitis media;
- hyperventilation.
Disorders that may present with dizziness and hearing symptoms are presented in the table.
The final diagnosis of Meniere's disease is made based on the results of dehydration tests (in response to drug dehydration, sound perception thresholds at low frequencies decrease and auditory perception of speech improves), extra- and transtympanic electrocochleography (a curve characteristic of endolymphatic hydrops) [9]. The summation potential (SP) and action potential (AP) are recorded. Violation of the ratio of SP/AP amplitude values (p > 0.3) is a characteristic sign of hydrops of the labyrinth, recording of vestibular evoked myogenic potentials (characteristic is the absence of peaks P13, N23 - a graph in the form of a straight line).
Examination of patients with Meniere's disease should include a number of mandatory tests. Traditional equilibrium tests that are diagnostically quite reliable include the Romberg test, the Unterberger test, the Babinski-Weil test, and the Barany index test. The listed studies have somewhat lost their significance in recent years, since specialized clinics use special equipment for vestibulometry and complicated tests. In addition, the “battery of tests” includes: detection of spontaneous otoneurological symptoms, caloric tests (heat and cold), Barany rotation test, smooth pursuit test, saccadic test, study of optokinetic nystagmus.
Treatment of Meniere's disease is empirical, since there is no consensus on the etiopathogenesis of this disease. All currently existing methods and methods of treatment are aimed at making patients more tolerant of attacks of dizziness, but do not significantly change the course of the process and do not prevent the development of hearing loss [7]. However, individual therapy, selected taking into account concomitant diseases, can slow down the development of hearing loss, reduce the severity of tinnitus, and reduce the frequency and severity of dizziness [5].
In the treatment of an acute attack of Meniere's disease, mainly medication and, if conditions exist, carbogen or oxygen therapy are used. They use sedatives and drugs that improve cerebral circulation (prochlorperazine, promethazine, cinnarizine, diazepam) [7], and dehydration agents. In the acute period, it is advisable to administer drugs parenterally or in suppositories. It is advisable to carry out behind-the-ear novocaine blockades [4].
One of the most well-known schemes for relieving an acute attack of Meniere’s disease is the scheme developed by I. B. Soldatov and N. S. Khrappo (1977): glucose 40% - 20.0 i.v., Pipolfen 2.5% - 2.0 i.v. /m (or Aminazine 2.5% - 1.0 w/m), atropine sulfate 0.1% - 1.0 s.c. (or platiphylline hydrotartrate 0.2% - 2.0 s.c.), caffeine sodium benzoate 10% - 1.0 s.c.; mustard plasters on the cervical-occipital region, a heating pad on the legs [9]. Sometimes xanthinol nicotinate 15% - 2.0 IM or cinnarizine or vinpocetine is added to the indicated regimen [4]. Treatment in the interictal period (maintenance therapy) should be comprehensive and quite active. Drugs that prevent the development or reduce endolymphatic hydrops are indicated: diuretics (furosemide, amiloride, hydrochlorothiazide), vasodilators (histamine analogue - betahistine dihydrochloride), drugs that improve cerebral circulation (cinnarizine, propranolol), corticosteroids, as well as non-drug treatment - vestibular rehabilitation, acupuncture .
One of the medications that effectively eliminates dizziness and reduces subjective ear noise is betahistine dihydrochloride, a synthetic analogue of histamine. Betahistine dihydrochloride was first synthesized in 1941 by Walter et al., and in 1970 it was registered as a drug for the treatment of Meniere's disease. Betahistine dihydrochloride does not have histamine side effects such as severe headache, facial flushing, diplopia and vomiting, and is taken orally.
According to modern concepts, betahistine dihydrochloride has three levels of action:
- on cochlear blood flow;
- to the central vestibular apparatus;
- on the peripheral vestibular apparatus.
Being a weak H1 receptor agonist and an active H3 receptor blocker, this drug stimulates postsynaptic histamine receptors. It is the H3-antagonistic effect of betahistine dihydrochloride that explains the effect of normalizing the excitation of the vestibular nuclei in the subcortical structures of the central nervous system and the vasoactive component of the action of this drug [11, 12]. It should be emphasized the selectivity of the vasoactive effect of betahistine dihydrochloride [11], which improves microcirculation of the inner ear and capillary permeability, and also normalizes endolymph pressure in the labyrinth, without leading to a pronounced decrease in blood pressure. The drug also has a positive effect on the transmission of nerve impulses in the medial and lateral vestibular nuclei and peripheral vestibular receptor formations [13]. The experience of many clinicians indicates that betahistine dihydrochloride reduces the intensity of dizziness, shortens the duration of dizziness episodes, and makes them more rare. The drug is effective both for relieving attacks of dizziness and preventing their relapses, and for reducing subjective ear noise.
It should be noted that it is advisable to use betahistine dihydrochloride in patients with Meniere's disease and in the postoperative period - dizziness, as a rule, disappears 3–4 days after surgery [5].
Of particular note is the use of aminoglycosides, which have a toxic effect on neuroepithelial cells of the inner ear. The method can be used in the late stages of BM with bilateral lesions and is used in persons for whom surgical treatment is contraindicated. Intratympanic administration of aminoglycosides is quite effective and possible with unilateral lesions [14].
If conservative treatment is clearly ineffective, various surgical interventions are advisable, both gentle (hearing-preserving) and destructive. Destructive methods are indicated for severe disabling forms of Meniere's disease. There are 5 groups:
1 — interventions on the autonomic nervous system (chord and chord plexusectomy); 2 - cutting the tendons of the muscles of the tympanic cavity; 3 — decompressive operations on the inner ear; 4 - destructive operations on the labyrinth; 5 - destructive operations on the vestibulocochlear nerve [5].
Hearing-preserving surgeries include:
- endolymphatic sac bypass is the most common surgical procedure for BM;
- sacculotomy - decompressive surgery on the spherical sac;
- intersection of the vestibular nerve to stop afferent impulses, which contributes to the disappearance of vestibular disorders.
If gentle types of surgical interventions are unsuccessful, destructive operations are performed:
- labyrinthectomy;
- cochleosacculotomy;
- vestibular neurectomy.
It should be noted that operations on the autonomic nervous system and cutting the tendons of the muscles of the tympanic cavity are ineffective, and decompressive and destructive surgical interventions, as a rule, lead to deafness in the operated ear and the resumption of attacks of dizziness in the long term due to fibrous fusion of the created anastomosis; destructive operations on the vestibulocochlear nerve are performed in neurosurgery departments.
Currently, a method of surgical treatment is used, such as laser destruction of the horizontal semicircular canal, which allows one to achieve relief from attacks of dizziness in the immediate and long term, preserve hearing and delay the development of the hydropic process in the other ear with a unilateral process.
However, despite the abundance of scientific works devoted to Meniere's disease, the many means and methods used in its treatment, the problem essentially remains unresolved, since to date there is no single treatment strategy recognized by all leading specialists. The search for an ideal treatment for Meniere's disease continues.
Literature
- Meniere MP Pathologie auriculare. Maladies de l'orielle interne offrant les symptoms de la congestion cerebrale apoplectiforme // Gaz. Med. de Paris. 1861. T. 16. P. 88–89.
- Hallpike CS, Cairns H. Observation on the pathology of Meniere's syndrome // J. Laryngol. Otol. 1938. Vol. 53. P. 625–655.
- Sagalovich B. M., Palchun V. T. Meniere's disease. M.: Medical Information Agency LLC, 1999. 525 p.
- Babiyak V. I., Lantsov A. A., Bazarov V. G. Clinical vestibulology. St. Petersburg: “Hippocrates”, 1996. 336 p.
- Patyakina O.K. Treatment tactics for vestibulogenic dizziness // Consilium medicum. Application. 2001. pp. 9–12.
- Monsell EM New and revised reporting guidelines from the Committee on Hearing and Equilibrium. American Academy of Otolaryngology - Head and Neck Surgery Foundation, Inc. Otolaryngology - Head and Neck Surgery. 1995. 113 (3). R. 176–8.
- Nurmukhametova E. Diagnosis and treatment of Meniere’s disease // Russian Medical Journal. 1998. No. 20. pp. 1346–1347.
- Bronsteind AM, Lempert Th. Dizzines. Cambridge University Press, 2007. P. 215.
- Gibson WP R, Prasher DK, Kilkenny GPG Diagnostic significance of transtympanic electrocochleography in Meniere's diseas // Ann. Otol. Rhinol. Laryngol. 1983. Vol. 92. P. 155–159.
- Soldatov I. B., Khrappo N. S. Methods of treating Meniere’s disease // Journal. ear, nose and throat bol. 1977. No. 6. p. 8–14.
- Timmerman H. Pharmacotherapy of vertigo: any news to be expected? // Acta Otolaryngol. 1994, Suppl 513, 28–32.
- Van Cauwenberge PB, De Moor SEG Physiopathology of H 3-receptors and pharmacology of betahistine // Acta Otolaryngol. 1997. Suppl. 526. P. 43–46.
- Arrang JM, Garbarg M., Quach TT, Toung MDT, Yeramian E., Schwarts JC Actions of betahistine at histamine receptors in the brain // Eur Pharmacol. 1985. Vol. 11. P. 73–84.
- Pfleiderer AG The current role of local intratympanic Gentamicin therapy in the management of unilateral Meniere's disease // Clin Otolaryngol. 1998. Vol. 23(1). P. 34–41.
O. V. Zaitseva, Candidate of Medical Sciences
FSBI Scientific Center of Otorhinolaryngology FMBA of Russia, Moscow
Contact Information
Treatment
Treatment of Meniere's disease is aimed at stopping and preventing the occurrence of attacks. Depending on the severity of the disease, treatment can be conservative or surgical. At the first symptoms, you should contact an otolaryngologist or neurologist.
Treatment for an attack of Meniere's disease
To relieve an attack of Meniere's disease, the patient is placed on a hard surface.
The eyes should be open and fixed at a fixed point, a heating pad may be applied to the legs, and exposure to loud sounds and bright lights should be removed. In order to relieve an attack of Meniere's disease, drugs are used that can relieve endolymphatic hydrops (diuretics), which leads to a decrease in intralabyrinth pressure. Symptomatic therapy is aimed at normalizing mental status, relieving vomiting and dizziness.
- During an attack, it is effective to administer atropine (subcutaneously 1 ml of 0.1% solution) to relieve impulses from the irritated labyrinth, 40% glucose solution;
- To eliminate this, dimenhydrate, a vestibular receptor blocker, is used. The effectiveness of betahistine has now been proven. The drug is able to cause dilation of the vessels of the inner ear, which leads to better blood supply, reabsorption and a decrease in the amount of endolymph. Papaverine is also sometimes used among vasodilators;
- In order to eliminate vomiting, antiemetic (antiemetics) drugs of central and peripheral action are used. The most popular substances are in release forms for intramuscular and rectal administration, since during an attack it is often impossible to take them orally due to profuse vomiting. These drugs include metoclopramide and thiethylperazine. Among the substances in the oral form are Bonin, Aviamarin, Ciel;
- To normalize the patient's mental state, sedatives are administered. Diazepam, Lorazepam, Mexidol have a pronounced anxiolytic effect;
- The use of diuretics in Meniere's disease is aimed at increasing diuresis, relieving ear congestion and, as a result, reducing the volume of endolymph (Manit, Diacarb). The use of diuretics must be combined with potassium supplements (Asparkam, Panangin).
A course of intravenous infusion of sodium bicarbonate will help normalize the alkaline reserve of the blood.
Treatment of Meniere's disease
Treatment of Meniere's disease has two directions: stopping attacks of systemic vertigo and preventing further changes in the inner ear.
Depending on the course of the disease, the presence of concomitant pathologies in the patient, the degree of dysfunction of the inner ear and other factors, various treatment methods can be used.
Drug treatment.
Based on the diagnostic results, the patient is prescribed the following groups of medications:
- neuroleptics;
- vasodilators;
- antihistamines;
- diuretics;
- antispasmodic;
- sedatives, etc.
The combination of drugs and specific names are selected by the doctor and taken according to the regimen specified by him. In most cases, treatment of the symptoms of Meniere's disease and its complications in the inner ear is carried out on an outpatient basis. For severe vestibular disorders, which are accompanied by nausea and vomiting, the prescribed drugs are administered by injection.
Surgery.
If the effectiveness of drug treatment is insufficient or completely absent, surgical intervention is recommended. Depending on the identified changes in the inner ear and other factors, surgery may have the following goals:
- Reduced fluid pressure on the cells of the inner ear. For this purpose, decompression operations are used to normalize the outflow of fluid from the ear cavity. For different indications, different methods can be used (drainage of the endolymphatic sac, perforation of the base of the stapes, and others).
- Destructive operations allow for controlled destruction of areas of the inner ear and its innervation pathways that are responsible for the occurrence of symptoms of Meniere's disease. This type of intervention is indicated for severe attacks of systemic vertigo that cannot be controlled with medications, and changes in the cavity of the inner ear have reached the point where drainage operations are inappropriate.
- Surgeries on the autonomic nervous system involve disconnecting the channel through which erroneous signals are “transmitted” from the inner ear to the brain. This allows you to solve the problem of systemic dizziness in the most radical way.
Other methods of treating Meniere's disease Treatment of this disease should be carried out simultaneously with the correction of the patient's life and diet.
Thus, products containing excess salt (pickles, sausage products, smoked meats, etc.) should be excluded from the menu. It is recommended to spend fasting days on a salt-free diet 1-2 times a week. In addition, you should avoid consuming alcohol, coffee and caffeine-containing drinks and products, as they have a negative effect on the nervous system and can, to a certain extent, provoke attacks of dizziness.
Physical activity should not be limited (provided that episodes of dizziness are controlled and treated with medications). Based on the direction of the otolaryngologist, the exercise therapy instructor will create a set of exercises that improve coordination of movements and, in general, strengthen the vestibular apparatus.
Treatment during the interictal period
Treatment during the interictal period consists of complex therapy: a salt-free diet, diuretics and long courses of betahistine hydrochloride.
A salt-free diet is aimed at changing the osmolarity of plasma and endolymph. Patients need to limit their salt intake to 2 g per day. A course of intravenous injections of sodium bicarbonate is required to maintain the acid-base balance of the blood. To improve the therapeutic effect, drugs are prescribed that improve blood circulation in the brain and inner ear (Polyglyukin, Reopoliglyukin, Cavinton), B vitamins, venotonics (Detralex), antispasmodics (Eufillin, Dibazol), sedatives. In order to reduce the frequency of attacks, patients are advised to limit provoking factors: stress, smoking, drinking alcohol, scuba diving, drinking caffeine; working at heights with moving objects is contraindicated. Currently, there is a good therapeutic effect of taking glucocorticoids orally or as injections into the eardrum.
Surgery
Surgical interventions on nerves and their plexuses are effective in the initial stage of Meniere's disease in the first two years. These include:
- Transection of the vestibular nerve is a complex neurosurgical operation. Allows you to preserve hearing, since only the vestibular part of the vestibular-cochlear nerve is removed. However, the following complications are possible: intracranial infections, headaches, liquorrhea;
- Destruction of the cervical node;
- At any stage of the disease, laser destruction of the semicircular canal receptor is possible. This allows you to preserve hearing functions;
- Operations aimed at restoring pressure in the membranous labyrinth are indicated for persistent hydrops at stages II-III:
- Drainage of the cochlear duct is carried out by dissecting it;
- Endolymphatic sac bypass;
- Opening the vestibular sacs.
Such surgical procedures have a high therapeutic effect and are not accompanied by complications from auditory perception.
Intratympanic administration of antibiotics, in particular gentamicin, is usually performed for unilateral lesions and may be accompanied by progression of hearing loss.
Complex treatment
The complex treatment of Meniere's disease includes physiotherapeutic procedures:
- head and neck massage;
- electrophoresis;
- sea, pine baths;
- UV irradiation of the collar area.
For several years, the Yusupov Hospital has been successfully treating Meniere's disease using new techniques. At the clinic you can get advice from the necessary specialist.
Prevention of Meniere's disease
Prevention of Meniere's disease is a relative concept, since the causes of the development of this disease and the provoking factors are not fully understood. But to reduce the likelihood of developing this disease, you should use gold health standards:
- treat all identified diseases in a timely manner, and also undergo regular preventive medical examinations;
- adjust your diet in favor of wholesome and healthy foods, and monitor compliance with the work and rest schedule;
- since allergies are one of the most likely factors provoking Meniere’s disease, the presence of an allergic reaction to something is a good reason for reorganizing your lifestyle in order to eliminate the influence of allergens on the body;
- giving up bad habits is another important step to maintaining overall health at the proper level, as well as reducing risks to the health of the inner ear.
Research Clinical Institute of Otolaryngology named after. L.I. Sverzhevsky offers you to undergo diagnosis and treatment of diseases of the inner ear of varying severity.
Treatment takes place with the participation and supervision of leading specialists in the field of otolaryngology and using the latest equipment.
Prognosis and prevention
Each patient has personal distinctive features, which lie in the nature of the disease, so it is not easy to give an accurate prognosis.
This has a great impact on the performance of patients. Often, conventional medications are needed to alleviate the disease; in special situations, doctors have to try various treatment methods until the patient’s well-being is improved. There is no prevention for Meniere's disease. But the disease can be caused by head injuries, so wearing a helmet is mandatory when driving some vehicles. Also, if you limit your salt intake, you can reduce the frequency of attacks. It is also important to avoid stress, tobacco, and alcohol.
To make an appointment and get advice from a qualified specialist, call the Yusupov Hospital call center.
Make an appointment