and other chronic diseases, you must notify your doctor.
It is worth knowing that spinal myelography is performed in the presence of doctors who will provide assistance. In some cases, doctors help administer the enema and are also responsible for giving the patient a sedative to suppress the swallowing reflex.
How is the examination carried out?
Before you sign up for myelography of the lumbar spine, it is worth learning about the methodology for performing it. To begin with, the patient is asked to lie down on a special table, after which the skin at the site of the future puncture is numbed with a local anesthetic and disinfected. After this, a puncture is carried out, the needle will move inward under the control of a fluoroscope. A contrast agent is injected, after which the needle is removed and the puncture site is disinfected again. Depending on which part of the spine is being examined, the person may be asked to lie on their stomach, side, or sit up when the needle is inserted.
After the contrast is administered, the patient should lie on his stomach, and the doctor will carefully tilt the table so that the substance is distributed along the subarachnoid canal of the spine. To take a photo, a person may be asked to turn over on their side and lie still, otherwise the result will be blurry.
The procedure will take from half an hour to an hour. After this, the patient will be sent to a ward, where he will be observed for two to four hours. At this time, the person will have to lie on an elevated (about 45 degrees) headboard and drink a lot, which will allow the contrast to be removed from the body more quickly.
Myelography with three-dimensional reconstruction
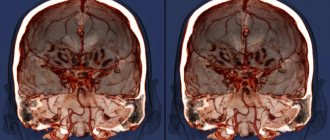
In this case, contrast myelography will be performed using a magnetic resonance imaging scanner. This involves data processing using special software. As a result, three-dimensional images will be obtained that will detect any abnormalities and pathological processes in the spine and spinal cord.
Contrast myelography
This is done using a computed tomograph. The peculiarity is that the procedure involves examination using x-rays. This is not permissible in all cases, so the decision will be made by the attending physician.
How to prepare for myelography
Before the study, the doctor will ask the patient in detail about the medications he is taking. Danger for the subject during myelography is represented by such groups of drugs as hypoglycemic (in particular, metformin), blood thinners (for example, warfarin), anticonvulsants and antidepressants. A few days before diagnosis, these medications should be stopped and replaced with other drugs of similar effect recommended by the doctor.
The patient should inform the doctor in detail about all allergy episodes he has had. Allergy to iodine and barium is of particular importance, since many contrast agents are based on these microelements.
The doctor must also know about all the patient's chronic diseases. Firstly, for some of them, myelography is completely contraindicated, and secondly, knowing about these diseases, specialists conducting the study can anticipate the development of certain complications and in a timely manner, and most importantly, respond adequately to them.
It is extremely important for women to notify their doctor if they may or may be pregnant because X-rays may have negative effects on the health and development of the fetus.
2-3 days before the study, the patient should exclude from his diet foods that cause fermentation and increased gas formation in the intestines (cabbage, baked goods, etc.) - the presence of a large amount of gas in it can “blur” the picture during the study. On the contrary, the amount of fluid consumed should be increased. It is not recommended to eat any food 8 hours before myelography, but you should still drink if you feel thirsty.
Before the puncture, susceptible patients may be prescribed sedatives; in addition, all subjects are given a cleansing enema.
During the examination, the patient removes some or all of his clothing and puts on a special hospital gown. It also removes glasses, jewelry, dentures, watches and other objects that may distort the image.
Decoding the results
Myelography with an iodine-containing drug is interpreted by a doctor with the appropriate qualifications, usually a radiologist. Based on the results of decoding, a conclusion is drawn up, which is given to the patient and with which he can go to the attending physician.
Advantages and disadvantages of the procedure
The advantages of the procedure are that it allows you to quickly identify problems that neither CT nor MRI without contrast would reveal. You can examine not only the spine, but also the spinal cord and nerve roots, which are almost impossible to see with other studies. As a result of the procedure, no traces of radiation remain in the body.
The disadvantages are that the administration of contrast does not give the most pleasant sensations: there is often a salty taste in the mouth, redness of the facial skin, a feeling of heat or burning, dizziness or headaches. Nausea or even vomiting may occur after contrast administration is stopped. Also, the procedure is not possible in all cases, since there are contraindications.
What does a spinal cord MRI show?
- Degenerative diseases of the spine, namely compression of the brain by a ruptured hernia. Depending on the degree of compression, patients will experience pain (such as electric shocks, lumbago), numbness, and impaired motor functions.
- Spinal cord injury. Injuries are divided into concussion, bruise and traumatic compression. A concussion may not manifest itself in any way, or it may manifest itself as short-term motor and sensory disturbances. With a bruise and traumatic compression, spinal shock develops with peripheral (hypotonic) paralysis and impaired pelvic functions. The shock goes away on average after 3-8 weeks.
- Spinal cord tumors, primary/secondary. For every 6 brain tumors there is 1 spinal tumor. It should be noted that primary vertebral tumors affecting the spinal cord are not brain tumors. They are divided into intra- and extramedullary (from the tissues surrounding the brain - membranes, roots, vessels, fiber). Extramedullary tumors (meningiomas, neuromas) are characterized by half conduction disturbance, radicular pain, when sneezing or coughing, pain is reflected at the site of the tumor, the same occurs when tapping on the spinous processes. With intramedullary tumors (ependymomas, astrocytomas, hemangiomas, granulomas), there is no pain, but there are motor and sensory disorders. Metastatic (secondary) damage is characterized by rapidly progressing flaccid (hypotonic) paraparesis (of both limbs), which then turns in spastic paralysis. With these pathologies, bone marrow fibrosis is often detected on MRI, as well as bone marrow edema, although these changes may be signs of other diseases.
- Demyelinating diseases of the brain (both spinal and brain). These include multiple sclerosis and acute multiple encephalomyelitis. Multiple sclerosis is a chronic autoimmune, constantly progressive disease that affects the myelin sheath of the nerves, which is responsible for the rapid passage of nerve impulses. This pathology can have many clinical pictures, but they all have similarities. Both debut and exacerbation in patients are caused by: previous viral infections; hyperinsolation, taking hot baths, saunas, etc.; pregnancy. This can manifest itself as spasticity in the lower extremities (most often), pelvic disorders (empirical urges, incontinence), headaches, and later they are joined by disturbances in swallowing, vision, hearing, and breathing. Currently, MRI is the only way to visualize foci of demyelination, in its This time marked a breakthrough in the diagnosis of MS. After the first onset, the patient is required to undergo an MRI; it is based on the scan results that a final diagnosis is made if the criteria for the detected number of lesions are met. Each focus of demyelination of the spinal cord on MRI is equivalent to that in the brain, which is taken into account when making a diagnosis. MRI of the spinal cord in multiple sclerosis is carried out simultaneously with a study of the brain, and gadolinium-containing contrast is used to search for fresh lesions. Acute disseminated encephalomyelitis has a benign course; it appears after a viral neurotropic infection (measles, influenza, rubella, herpes and others, including after vaccinations). It is characterized by an acute onset with fever, signs of encephalitis, paresis, and paralysis. With adequate treatment, symptoms disappear within a month. A distinctive feature of MRI of the spinal cord with contrast is the “symptom of rings, half rings.”
- Amyotrophic lateral sclerosis, or motor neuron disease, or Charcot's disease, is characterized by damage to the motor pathways, as a result of which a person slowly develops paralysis of all muscles. The probable cause is a gene mutation. Debuts at the age of 40-50 years. MRI of the spinal cord in ALS reveals pathology of the anterior horns of the spinal cord, especially diffusion tractography helps in diagnosis.
- Bone marrow ischemia or infarction develops when the artery supplying the spine is blocked, spasmed or compressed. In this case, an MRI of the spinal cord vessels is performed to identify the location of the source of the impaired blood supply.
- Chronic anemia, or rather one of its signs is bone marrow reconversion (replacement of adipose tissue with blood-forming cells as an attempt by the body to increase the production of red blood cells).
Contraindications for
It is impossible to undergo myelography in the following cases:
- state of fever;
- diseases of the kidneys, heart, liver in the stage of decompensation;
- severe arthritis;
- pregnancy;
- previous spinal surgeries;
- anatomical features or defects that prevent the introduction of a substance into the subarachnoid cavity;
- infectious processes on the skin in the place where contrast needs to be administered;
- inability to maintain one position during the procedure.
The final decision should be made by the doctor, since sometimes it happens that the possible risk is less than the benefit of the x-ray procedure.
Indications for spinal myelography
Myelography of the spine is indicated for the following conditions:
• Neurological disorders (numbness and pain in the limbs, etc.); • Identification of neoplasms and clarification of the reasons for their development; • Confirmation of arachnoiditis; • Detection of malignant tumors in the postcranial fossa; • Determination of nerve root damage; • Detection of stenoses in the spinal canal; • Infection of the spinal canal and nerve roots; • Detection of some herniated discs; • Pathologies of vertebral vessels.
Main services of Dr. Zavalishin’s clinic:
- consultation with a neurosurgeon
- treatment of spinal hernia
- brain surgery
- spine surgery
Advantages of myelography compared to other research methods
Myelography is the most modern research method, and therefore has the greatest information content.
The use of this method of studying the spine allows you to: • Determine all the contours of the spinal cord and nerve roots, thanks to the use of contrast agents. • Do not leave any signs of diagnostics on the patient’s body.
Unlike research methods such as CT and MRI, spinal myelography is able to identify more serious problems and pathologies that are not subject to other methods of diagnosing the spine.
After the procedure
At the end of the procedure, the patient must remain under the supervision of medical staff for several hours. If there are no complications and the patient’s health is normal, then he can leave the medical facility. During your stay in the hospital, the doctor analyzes the X-rays obtained and, if a problem is detected, makes a diagnosis and prescribes treatment.
During the day after myelography of the spine, a person should lie in bed, keeping his head slightly elevated. You should also drink as much water as possible in order to quickly return the body to its normal state. For a couple of days after the test, you should not exercise, lift weights, or make sudden movements.
After 2-3 days, it is recommended to start doing simple physical exercises on your back: bending, turning. This helps remove contrast. After myelography, the following complications may occur: bleeding in the puncture area, headaches, fever, vomiting, impaired mobility or paresthesia. If such symptoms occur, you should immediately go to the hospital. You can avoid the development of complications if you follow your doctor’s advice.
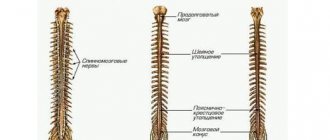
MR 3D myelography description
Modern magnetic resonance imaging scanners allow a three-dimensional (3D) reconstruction of the examination area. Using this function of the software application, it is easier to describe the images, but you should know the normal anatomical features of the structure of the spinal segment.
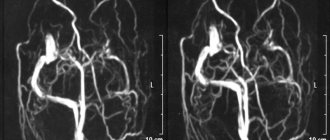
Scheme of contrast cisternography of the brain (a) and MR myelography of the spinal cord (b). Such tomograms could be obtained at the beginning of the use of magnetic resonance imaging in medicine. Technology gradually improved. Contrast intravenous MRI of the spine with 3D modeling began to be used somewhat later.
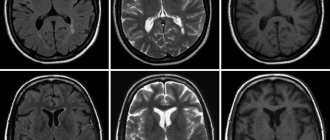
Sagittal sections from MRI of the spine. Studies were performed on a patient with stenosis at levels C3-C6 before surgery to install stents. 3D reconstruction allowed for high-quality surgical treatment.