24.11.2016
Pinchuk Elena Anatolyevna
Deputy chief physician for medical work, kmn, neurologist, doctor of physical and rehabilitation medicine
Belkin Vladimir Andreevich
Head of the Department of Early Medical Rehabilitation, Physician of Physical and Rehabilitation Medicine, Neurologist
Lipovka Nadezhda Sergeevna
Head of the Department of Medical Rehabilitation, Physician of Physical and Rehabilitation Medicine, Neurologist
Sobolev Arkady Igorevich
Doctor of physical and rehabilitation medicine, neurologist
Ischemic stroke has several stages of progression. The first stage is an acute period of ischemic stroke, which lasts up to the 21st day. During the first 3-5 days, perifocal cerebral edema develops, karyoplasmic and cytoplasmic cells shrink.
An important point in the acute period of ischemic stroke is to correctly diagnose. First of all, it is necessary to distinguish any other diseases of the nervous system from a stroke. Next, the nature of the stroke itself is determined, and what caused it (hemorrhage in the cerebral cortex or blood clot). At the last stage of diagnosis, the localization of the lesion is determined, as well as the pathogenesis of cerebral infarction during stroke.
Stages of diagnostics of the acute period
- Stage 1. The victim is urgently hospitalized. The doctor receives basic information from the words of the patient, his relatives or surrounding people. External signs of cerebral circulatory disorders, emotional background, physical stress, and blood pressure levels allow a diagnosis to be made fairly quickly and accurately. The patient's medical history is studied for the presence of other diseases that can provoke the development of ischemic stroke (arrhythmia, atherosclerosis, previous heart attack, etc.). However, the possibility of making an incorrect diagnosis exists in the case of an epileptic seizure, a brain tumor, a head injury, a hypoglycemic state, etc.
- Stage 2. The most important point of this stage is to quickly and accurately determine the nature of the disease. The tactics of first aid and further treatment will depend on this. A computed tomography scan of the brain is performed, since the clinical picture alone cannot provide completely reliable information.
- Stage 3. After a quick history has been collected, the clinical picture has been identified and a CT scan has been performed, the doctor begins to choose treatment tactics. The subtype of stroke is also determined (lacunar, atherothrombotic or cardioembolic, etc.). The correct choice of therapy will help not only provide timely assistance to the victim, including surgery, but also prevent a possible recurrence of a heart attack in the future.
Late recovery period
This period of stroke occurs the latest in time - six months after the acute one - and lasts up to two years. Usually at this stage, patients can already take care of themselves, their speech and basic body functions are restored. The focus is on fine motor skills, exercises that reinforce new functions in areas of the brain that were not damaged by the stroke.
After a year, doctors talk about a period of long-term consequences. Patients must undergo a preventive examination once a year and, if possible, treatment.
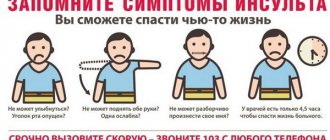
If the patient or those around him paid attention to the first symptoms of a stroke in time and immediately consulted a doctor, the chances of restoring the most important functions increase markedly. After all, the most important thing is to establish normal blood supply to the brain in the first hours after an attack. This is what guarantees minimal damage to the nervous tissue and preservation of functions.
Therapy for ischemic stroke in the acute period
In the first three weeks (during the acute period), general measures are taken:
- The required oxygen level is maintained;
- Blood pressure stabilizes;
- Cardiac activity is under medical supervision;
- The condition of the bladder and intestines is monitored;
- Passive gymnastics is carried out on all limbs of the victim;
- Prevention of bedsores;
- Antibacterial therapy, including taking antifungal drugs.
Depending on the specifics and subtype of ischemic stroke, special therapy is carried out.
Acute ischemic stroke may recur if the diagnosis is not reliable and not all emergency measures have been taken. In the acute period, secondary hemorrhage into damaged tissue of the cerebral cortex poses a great danger. As a rule, this occurs in the first 10 days after the onset of a stroke. It is almost impossible to detect this complication visually. Only with the help of computed tomography and x-ray examination do they find a new lesion and take action. The reason for this complication is the lack of necessary control over blood pressure, as well as reperfusion therapy. Some patients have serious contraindications for it.
Clinical Brain Institute Rating: 4/5 — 2 votes
Share article on social networks
Management of patients in the early recovery period of stroke
E.Yu. SUSLOVA
,
N.V.
VAKHNINA , Candidate of Medical Sciences,
Department of Nervous Diseases and Neurosurgery of the First Moscow State Medical University named after.
THEM. Sechenova, Moscow A review of the main risk factors for ischemic stroke and principles of patient management in the early recovery period of ischemic stroke are presented. Particular attention is paid to the secondary prevention of recurrent stroke and the use of neuroprotective drugs as part of the complex treatment of patients who have suffered a stroke.
Relevance of the problem
Acute cerebrovascular accidents (ACVA) are one of the most common pathological conditions in neurological practice [1]. According to the World Federation of Neurological Societies, at least 15 million strokes are registered annually in the world [1]. At the same time, it is believed that not all strokes are registered, and the real figure is much higher. In the Russian Federation, more than 400,000 strokes are registered annually, with strokes accounting for about 19% of the total mortality rate [2, 3]. About 30% of strokes lead to death in the acute period of the disease [1, 4—6]. Stroke reduces the life expectancy of men by 1.62–3.41 years, and of women by 1.07–3.02 years [3].
Etiology and pathogenesis of ischemic stroke
According to the generally accepted TOAST classification (Adams HP et al., 1993), there are currently 5 pathogenetic subtypes of ischemic stroke (IS):
- atherothromboembolic, - cardioembolic, - lacunar (due to occlusion of a small vessel), - stroke of another established etiology, - stroke of unknown etiology. As a result of numerous epidemiological studies conducted in recent years, factors have been identified that increase the risk of developing IS, among which there are unchangeable and changeable ( Table 1
).
| Table 1. Fixed and modifiable risk factors for IS | |
| Unmodifiable risk factors for AI | Modifiable risk factors for IS [5 ] |
|
|
Management of the patient in the acute period should be carried out in a specialized department of the hospital (primary vascular department). Further, in the early recovery period (ERP), for rehabilitation, the patient can be transferred to specialized inpatient or outpatient centers or discharged home. The goals of treating a patient in a RVP include restoration of lost motor, speech and other functions, secondary prevention of stroke in a particular patient, social and psychological assistance.
As a result of IS, 15–30% develop permanent disability and 40% develop moderate recovery [4, 7]. Restoring the ability to self-care and independent living largely depends on the type of neurological defect. With only hemiparesis, patients can often move independently and live without assistance. Even if sensory disorders are added, help is usually only partially necessary. If a patient develops hemianopsia as a result of AI, outside assistance may often be required when moving. The prognosis significantly worsens with the formation of severe cognitive disorders, aphasia, anosognosia, depression, pain syndrome, severe bulbar or pseudobulbar syndromes [5].
Restoring a neurological deficit primarily involves activating the patient [7]. Constant physical activity leads to a reduction in motor deficit: regular walks improve walking, specialized gymnastics helps restore hand function. It is possible to use orthoses for foot paresis, muscle relaxants for the development of severe spasticity. The goal of motor rehabilitation is to achieve maximum independence for the patient, for which, first of all, it is necessary to restore the patient’s everyday skills (dressing, toileting, eating, moving around the house and on the street). Speech therapy classes are highly effective in reducing the severity of speech disorders.
Cognitive impairment can significantly worsen the patient’s prognosis in terms of rehabilitation, quality and life expectancy; in addition, they reduce the patient’s adherence to therapy [5, 8]. Within 1 year after a stroke, 25–30% of patients develop dementia, and in ⅓ of them it is associated with decompensation of concomitant neurodegenerative changes in the brain [9]. To improve memory and other cognitive functions in patients with moderate and mild cognitive impairment, sufficient mental exercise, memory training, and the use of medications are recommended. For cognitive disorders reaching the level of dementia, acetylcholinergic (donepezil, galantamine, rivastigmine) and glutamatergic (memantine) drugs are used. With the use of these drugs, there is a decrease in cognitive and other neuropsychiatric disorders. Acetylcholinesterase inhibitors reduce acetylcholinergic deficiency that occurs against the background of damage to central acetylcholinergic structures, and memantine normalizes the pattern of impulse transmission in glutamatergic synapses. The choice of a specific drug is determined by the severity and nature of cognitive impairment, the presence of concomitant diseases, and drug tolerance.
Approximately 60% of patients develop depression in the post-stroke period, which is also a risk factor for recurrent strokes, myocardial infarction, and deterioration of cognitive functions [4]. All patients with post-stroke depression are recommended to have rational psychotherapy and the prescription of antidepressants (tricyclics or selective serotonin reuptake inhibitors) with their individual selection in each specific case. Adequate treatment of depression is important to improve the quality of life of patients and their relatives, as well as to reduce mortality for several years after a stroke [4].
Secondary prevention of IS
Secondary prevention of IS in patients who have suffered a stroke or transient ischemic attack (TIA) is of great importance. The maximum risk of recurrent IS is observed in the first days after TIA or IS, so the start of preventive measures should occur in the acute period and continue during the recovery period of stroke. Secondary prevention of IS primarily includes the correction of risk factors and is carried out using non-drug, medicinal and surgical methods.
Non-medicinal methods include giving up bad habits - smoking and drinking alcohol, diet, and dosed physical activity. Quitting smoking or reducing the number of cigarettes smoked (even among smokers with many years of experience) significantly reduces the risk of recurrent IS and myocardial infarction. Stopping alcohol intake reduces the risk of recurrent stroke and cerebral hemorrhage.
Increasing physical activity with regular aerobic exercise helps improve the condition of the cardiovascular system of patients who have suffered a stroke. The first place is occupied by walking or therapeutic exercises at home (if there is a neurological defect that makes walking difficult). The patient is recommended to gradually achieve the level of pre-stroke physical activity or exceed it if physical inactivity was observed before the stroke. In addition, physical activity helps reduce blood pressure (BP), excess body weight, and cholesterol levels [5]. A low-cholesterol diet is advisable; for concomitant diabetes mellitus, glycemic control and appropriate nutrition are advisable. Reducing excess body weight helps reduce blood pressure, cholesterol and blood glucose levels.
Antithrombotic therapy includes the prescription of antiplatelet agents for non-cardioembolic stroke (atherothrombotic, lacunar, stroke of unknown etiology) and indirect anticoagulants for cardioembolic stroke.
The result of the action of antiplatelet drugs is a decrease in platelet aggregation, which prevents their fixation on the atherosclerotic plaque and, as a consequence, the formation of a blood clot. It has been proven that long-term use of antiplatelet drugs in patients who have suffered ischemic stroke or TIA significantly reduces the risk of developing a recurrent stroke. It is advisable to prescribe antiplatelet agents with proven antiplatelet activity. These drugs include acetylsalicylic acid at a dose of 75-325 mg/day, clopidogrel at a dose of 75 mg/day, a combination of 25 mg of aspirin and 200 mg of slow-release dipyridamole. Several large studies have shown higher efficacy of clopidogrel and the combination of aspirin with extended-release dipyridamole compared with aspirin [10].
As a secondary prevention of IS in patients who have suffered a cardioembolic stroke (i.e., suffering from atrial fibrillation, valvular disease) and having an intraventricular thrombus or other risk factors for cardiac embolism, anticoagulants are used. The gold standard of anticoagulant therapy has long been warfarin, the dose of which must be gradually titrated and then adjusted depending on the international normalized ratio (INR). When taking warfarin, INR should be measured once every 2 weeks. and be maintained in the range from 2 to 3 [9, 10]. In recent years, oral anticoagulants have been actively developed and studied in patients with atrial fibrillation, which do not require regular monitoring of the INR and are not inferior in their effectiveness to warfarin: dabigatran, rivaroxaban and apixaban. These drugs are much more convenient for use by patients and have similar efficacy and safety to warfarin. However, the use of these drugs is limited due to their high cost [5, 10].
Correction of dyslipidemia requires the prescription of statins for a long time. Statins are used for both secondary and primary prevention of stroke in patients at high risk of developing IS. These drugs significantly reduce the likelihood of developing not only ischemic stroke, but also myocardial infarction in patients suffering from coronary heart disease, diabetes mellitus, or who have had stroke, even with normal blood cholesterol levels [5, 9, 11, 12]. The main importance is to reduce the level of low-density lipoprotein cholesterol and slow the progression of atherosclerosis.
Normalization of blood pressure is one of the most effective areas of secondary prevention of IS. According to a meta-analysis of randomized trials, effective treatment of arterial hypertension (AH) can prevent 30-40% of recurrent strokes [5]. Several large studies have shown that blood pressure control not only reduces the likelihood of recurrent stroke, but also helps reduce the severity and rate of progression of post-stroke cognitive impairment. As mentioned above, regular exercise and diet can help lower blood pressure, and reducing the amount of salt in food is also helpful. Drug therapy for hypertension significantly reduces the risk of recurrent stroke, myocardial infarction, and death from cardiovascular pathology [5, 13, 14]. At the same time, studies have shown that angiotensin-converting enzyme inhibitors (ACEIs), diuretics, and their combinations are effective [13–15]. The choice of antihypertensive agent also depends on the patient's comorbidities. Research results show that even a small, stable reduction in blood pressure (by 5/2 mm Hg) can significantly reduce the risk of recurrent IS (by 29%) [5, 16]. The results of the PROGRESS study showed that in patients who had suffered a stroke or TIA, the use of a combination of perindopril 4 mg/day and indapamide 2.5 mg/day for four years reduced the risk of developing a recurrent stroke by an average of 28% [12, 13] . Based on the PROGRESS study, patients who have suffered an IS or TIA are recommended to receive antihypertensive therapy even with normal blood pressure levels [5, 7]. Thus, patients who have suffered an IS or TIA are recommended to gradually reduce blood pressure to normal values over several months - below 140/90 mmHg. Art. In the absence of hemodynamically significant stenoses of the main arteries of the head (less than 70%), target blood pressure numbers should not be higher than 130/85 mmHg. Art.; with concomitant diabetes mellitus and renal failure, a more significant reduction in blood pressure below 130/80 mmHg is advisable. Art. [5, 7]. If there is a more severe stenosis (70% or more) of at least one main artery of the head, the patient should be consulted by an angiosurgeon to decide on possible surgical treatment (carotid endarterectomy, in more rare cases, stenting). When stenosis of more than 70% is detected in the carotid region on the side of the affected hemisphere in a patient who has suffered IS or TIA, surgical treatment in the early stages (in the first 2-3 weeks) has advantages over conservative management of patients. With stenosis less than 70% or in late stages (after 6 months), the benefits of surgical treatment are questionable.
Neuroprotective, nootropic therapy has been of great interest to doctors for many years. These drugs should reduce the damaging effects of pathological processes that occur in the brain during ischemia (activation of excitatory amino acids and intracellular proteases, release of calcium into the extracellular space, apoptosis, damage to cell membranes). Experimental studies on animals and in vitro have provided evidence of the effectiveness of many drugs from the group of neuroprotectors.
Ginkgo biloba (120 mg/day), choline alfoscerate (1,000 mg/day), piracetam (1,200–2,400 mg/day), vinpocetine (30 mg/day), etc.
Unfortunately, there are still no results from large randomized, placebo-controlled, multicenter studies that would prove the effectiveness of these drugs in patients who have suffered a stroke. A new drug for Russia, Duzopharm (), whose active ingredient is naftidrofuryl, deserves attention.
The mechanism of action of the drug Duzopharm is associated with the selective blockade of serotonin receptors of the 5-HT2 class (5-hydroxytryptamine). The interaction of serotonin with these receptors leads to contraction of vascular smooth muscle [17], platelet aggregation and increased vascular permeability (Kirsten et al., 1995). Moreover, the decrease in cerebral blood flow induced by serotonin [22] is more pronounced at the level of collateral vessels, the condition of which plays a decisive role in limiting the spread of the necrosis zone.
Duzopharm, by blocking serotonin 5-HT2 receptors, prevents arteriolar spasm, platelet aggregation and reduces vascular permeability, and also improves collateral blood flow and limits the spread of the infarction zone [23].
The effects of serotonin, realized through serotonin receptors of the 5-HT2 class, play an extremely important role in the development of major events at the site of vascular accident in the brain. Increased platelet aggregation, destruction of the blood-brain barrier, as well as the release of serotonin from damaged tissues contribute to a significant increase in the level of this mediator in areas of “vascular catastrophe”. Under ischemic conditions, the endothelium loses its ability to absorb serotonin, and its concentration increases significantly. In addition, a direct relationship has been identified between the absorption of serotonin and the degree of hypoxia [24]. These facts indicate an extremely pronounced negative role of serotonin in aggravating the ischemic picture, which contributes to an increase in the infarction area in the acute period of ischemia and contributes to the formation of a “vicious” circle that prevents the restoration of blood flow in the post-ischemic period.
Equally important is the development of a hypersensitivity reaction to serotonin, which occurs on the part of the vessels passing through ischemic tissues, as a result of which patients in the post-stroke period experience a strong reaction to serotonin, which became even more intense with increasing duration of the recovery period [25]. This fact indicates that the hypersensitivity of the serotonergic system persists for a long time and can play a decisive role in the development of recurrent stroke [25]. Among the prerequisites for the development of hypersensitivity to serotonin, it is necessary to note atherosclerosis and hypertension.
Naftidrofuryl has been successfully used in the treatment of acute and chronic neurovascular pathologies for more than two decades.
Duzopharm, unlike other vascular drugs, acts only in ischemic areas and does not spread to intact vessels - this eliminates the “steal” syndrome and the effect on systemic blood pressure, which seems to be an important advantage in the treatment of a patient with impaired cerebral blood flow. In addition to vascular effects, Duzopharm has nootropic and anxiolytic effects, which allows its use to be considered as a complex therapy that affects key pathological processes both in the acute period of IS and in the rehabilitation period.
Naftidrofuril has an extensive evidence base in the treatment of vascular pathology: more than 18 randomized placebo-controlled studies have been conducted.
Naftidrofuryl in in vitro studies led to the cessation of platelet aggregation and an increase in the level of metabolism in damaged brain tissue [13, 18, 19].
Naftidrofuryl improves the functional state of neuronal activity in adult healthy volunteers: after 5 days of therapy on functional MRI, the signal from the right frontal lobe, middle and inferior frontal gyri, both temporal lobes and areas of the occipital lobes was more intense in subjects receiving naftidrofuryl compared to those receiving placebo. In this case, changes were noted on the EEG, in particular a decrease in alpha activity [18].
The use of naftidrofuril shortens the hospital stay of a patient with acute stroke [20]. A review of 4 placebo-controlled studies showed the effectiveness of the addition of naftidrofuryl to standard therapy in the subacute period of IS in relation to physical activity and walking after treatment [21].
A multicenter, randomized, placebo-controlled trial of 339 subacute ischemic stroke patients meeting criteria for vascular dementia aged 50 to 85 years compared naftidrofuryl (400 or 600 mg) as adjunctive therapy versus placebo. Patients received antiplatelet (aspirin and dipyridamole) therapy and physical rehabilitation. If necessary, therapy with small doses of benzodiazepines and short-acting antipsychotics was allowed. According to the study results, the proportion of patients who experienced deterioration decreased from 42 to 25% in the placebo group and to 27% in the naftidrofuryl 400 and 600 mg groups, respectively. There was no significant difference in the dynamics of regression of cognitive impairment between the groups receiving the drug in different doses. During the study, adverse events occurring after randomization were reported in only 13% of patients. None of the symptoms reported could, in the opinion of the investigators, be considered possibly or likely related to the study drug. None of the participants showed any clinically significant changes in laboratory or hematological parameters during the study [19]. Thus, the drug Duzopharm (naftidrofuril) can be effectively used in patients who have undergone IS in order to restore lost brain functions and reduce the severity of cognitive impairment.
Conclusion
Management of a patient in the early recovery period of IS should be comprehensive, i.e., include non-drug and medicinal methods. The purpose of various methods of therapy and the importance of carrying out all activities in the recovery and subsequent periods of the disease should be explained to the patient and his relatives. Taking into account the individual characteristics of each specific patient, antihypertensive and antithrombotic drugs are prescribed, if necessary, statins, antidepressants, hypoglycemic, glutamatergic, and cholinergic drugs. The combination of several means of secondary prevention of IS (diet, exercise, taking an antiplatelet or anticoagulant drug, a statin and antihypertensive drugs) can reduce the risk of developing a recurrent stroke by almost 80%, thereby preventing 4 out of 5 possible strokes. Motor rehabilitation is not only aimed at compensating for the focal defect, but also helps improve cognitive functions and quality of life of patients. When prescribing drugs, it is advisable to give preference to drugs with proven safety and effectiveness, long-term course treatment of which can contribute to a more complete restoration of the functions of the central nervous system after a stroke.
Literature
1. Zakharov V.V. Treatment of ischemic stroke. Russian Medical Journal, 2006, 14, 4: 242-246. 2. Faizulin E.R. Rehabilitation of patients with cerebral ischemic stroke in the late recovery period at the outpatient stage: dis. ...cand. honey. Sci. Irkutsk, 2009. 172. 3. Gusev E.I., Skvortsova V.I., Stakhovskaya L.V. Epidemiology of stroke in Russia. Journal neurology and psychiatry named after. S.S. Korsakov. Stroke: adj. to zhur., 2003, 8: 4-9. 4. Parfenov V.A. Post-stroke depression: prevalence, pathogenesis, diagnosis and treatment. Neurology, neuropsychiatry, psychosomatics, 2012, 4: 84-88. 5. Parfenov V.A., Khasanova D.R. Ischemic stroke. M.: MIA, 2012: 288. 6. Damulin I.V., Parfenov V.A., Skoromets A.A., Yakhno N.N. Circulatory disorders in the brain and spinal cord. Diseases of the nervous system. Guide for doctors. Ed. N.N. Yakhno. M.: Medicine, 2005, 1: 232–303. 7. European Stroke Organization (ESO) Executive Committee; ESO Writing Committee. Guidelines for Management of ischemic stroke and transient ischemic attack. Cerebrovasc Dis, 2008: 457-507. 8. Parfenov V.A., Verbitskaya S.V. Management of a patient who has had a stroke. Neurology, neuropsychiatry, psychosomatics, 2013 (special issue 2): 23–27. 9. Yakhno N.N., Zakharov V.V., Lokshina A.B., Koberskaya N.N., Mkhitaryan E.A. Dementia. M.: MEDpress-inform, 2010. 10. Zhitkova Yu.V., Saykhunov M.V., Khasanova D.R. Prevention of cerebrovascular accidents. Consilium medicum, 2011, 9, 13: 5-8. 11. Zakharov V.V. Chronic cerebrovascular insufficiency. Difficult Patient, 2005, 12: 12-15. 12. Parfenov V.A. Prevention of recurrent ischemic stroke. Russian Medical Journal, 2008, 16, 1: 1694-1699. 13. Dufouil S, Chalmers J, Coskun O. Effects of blood pressure lowering on cerebral white matter hyperintensities in patients with stroke: the PROGRESS (Perindopril Protection Against Recurrent Stroke Study) Magnetic Resonance Imaging Substudy. Circulation, 2005, 112(1l): 1644–1650. 14. Rashid P et al. Blood pressure reduction and secondary prevention of stroke and other vascular events. Stroke, 2003, 34: 2741-2748. 15. Vakhnina N.V. Cognitive impairments and their treatment in patients with arterial hypertension. Medical Council, 2014, 5: 30-36. 16. PATS Collaborating Group. Post-stroke antihypertensive treatment study. A preliminary result. Chin Med J (Engl). 1995. 108(9): 710-717. 17. Oudart N. Naftidrofuryl Inhibits Contractions to Serotonin in Intact and De-endothelialized Cerebral Arteries in vitro. Journal of cardiovascular pharmacology. 1990. 16(3): 45-48. 18. Boeijingaa PH, Nedeleca JF, Demazièresa A, Souana ML, Gamandb S, Gillesa C, Parotc P, Stanera L, Luthringera R, Machera JP. Characterization of the CNS Effects of Naftidrofuryl (Praxilène) by Quantitative EEG and Functional MRI: A Study in Healthy Elderly Subjects. Neuropsychobiology, 2003. 48. 160–168. 19. Muller HJ, Hartmann A, Kessler C, Rainer M, Brown T, Gamand S, Lehert P. Naftidrofuryl in the treatment of vascular dementia. European Archives of Psychiatry and Clinical Neuroscience. 2001. 251. 247–254. 20. Shteiner TJ. Naftidrofuril after acute stroke: a review and hypothesis. Journal of cardiovascular pharmacology. 1990. 16. 3: 58-61. 21. Capon A, Lehert P, Opsomer R. Natfidrofuryl in the treatment of subacute stroke. Journal of cardiovascular pharmacology. 1990. 16. 3: 62-66. 22. Welch KMA, Hashi K, Meyer JS. Cerebrovascular response to intracarotid injection of serotonin before and after middle cerebral artery occlusion. J Neurol Neurosurg Psych 1973, 36:724-35. 23. Wiernsperger NF. Serotonin 5-HT2 Receptors and Brain Circulation. Journal of Cardiovascular Pharmacology™. New York: Raven Press, Ltd., 1990, 16(3): 20-24. 24. Salzman SK, Hirofuji E, Llados-Eckman C, McEwen GD, Beckman AL. Monoaminergic responses to spinal trauma. J Neurosurg 1987, 66:431-9. 25. Ricci A. Amenta F. Autoradiographic localization of 5-HT2 receptors in rat cerebral vessels. Annual Meeting of the European Neuroscience Association. Zurich, 1988: 48.
Source:
Medical Council, No. 18, 2014
Programs:
Assessment of rehabilitation potential
Rehabilitation after stroke
Restoration of cognitive functions
Diagnosis of swallowing disorders and correction
Restoration and correction of speech disorders