An acute infectious disease that occurs when microorganisms penetrate the membranes of the brain and develop an inflammatory process in the central nervous system is called meningitis. When a patient with suspected meningitis is admitted to the Yusupov Hospital, doctors conduct a neurological examination and perform a spinal tap. Only the results of a study of cerebrospinal fluid make it possible to establish an accurate diagnosis, identify the causative agent of infection, determine its sensitivity to antibacterial drugs, and select adequate antimicrobial therapy.
A blood test for meningitis reveals acute inflammatory changes. Meningococci (bacteria that cause meningitis) are found in a smear from the mucous membranes of the nasopharynx. In order to clarify the nature of the disease and determine the severity of the pathological process, patients undergo the following tests:
- polymerase chain reaction;
- determination of glucose in blood serum;
- general clinical examination of stool (coprogram);
- determination of creatinine, ALT, AST, total bilirubin, lactate and procalcitonin in blood serum.
If viral meningitis is suspected, immunoglobulins M to herpes simplex viruses type 1 and 2 (HSV-I, II) are determined in the blood serum, Ig M to the early antigen of Epstein-Barr virus (HSV-IV) and cytomegalovirus (HSV-V) in blood serum by immunochemiluminescence method.
Patients are recorded an electrocardiogram, an electroencephalogram, computed tomography and magnetic resonance imaging are performed. All instrumental studies are carried out using the latest equipment from leading global manufacturers.
After the diagnosis is established, complex therapy for meningitis begins according to Russian, European and American recommendations. When drawing up an individual treatment regimen for patients, doctors take into account the serotype of the pathogen, its sensitivity to antibacterial drugs, the severity of the disease, and the severity of symptoms. For bacterial meningitis, antibiotics begin to be administered no later than 60 minutes after the initial examination of the patient.
If the results of laboratory tests do not correspond to the clinical picture of the disease, the patient’s management tactics are discussed at a meeting of the expert council. It includes candidates and doctors of medical sciences, doctors of the highest category. They are traveling specialists in the diagnosis and treatment of infectious diseases of the central nervous system.
Cerebrospinal fluid examination for meningitis
The only reliable method for quickly diagnosing meningitis is to examine the cerebrospinal fluid. By analyzing changes in the cerebrospinal fluid and the results of other studies, doctors make a differential diagnosis for serous and purulent meningitis, identify the causative agent of the disease, determine the severity of the intoxication syndrome, and monitor the effectiveness and treatment.
The first study of cerebrospinal fluid is carried out upon admission of the patient to the neurology clinic. Analysis results can be ready 2 hours after taking cerebrospinal fluid samples. The presence of a large number of neutrophils in the cerebrospinal fluid in most cases indicates the bacterial nature of the disease. After 8-12 hours, the analysis is repeated and checked to see if a lymphocytic shift has appeared. If bacteria are detected in the cerebrospinal fluid samples, the test is repeated several times. The need to perform a lumbar puncture disappears when the clinical signs of the disease reverse, the number of cells, protein and sugar in the cerebrospinal fluid normalizes, and microorganisms disappear from the cerebrospinal fluid.
Due to the cause of the disease, purulent bacterial meningitis is heterogeneous. In 90% of cases, the disease is caused by Neisseria meningitis, streptococcus pneumoniae and Haemophilus influenzae. The most important feature of changes in cerebrospinal fluid during meningitis is pleocytosis. With purulent meningitis, the number of cells in the cerebrospinal fluid is more than 0.6 × 109/l. In this case, the study of cerebrospinal fluid is carried out no later than 1 hour after its collection.
With purulent meningitis, the cerebrospinal fluid is cloudy, whitish or green. It is dominated by neutrophils. The number of formed elements varies widely. In some cases, already in the first samples of cerebrospinal fluid, cytosis is 12 – 30 × 109/l. The severity of the inflammatory process in the membranes of the brain is judged by the nature of pleocytosis. A decrease in the relative number of neutrophils and an increase in the relative number of lymphocytes in the cerebrospinal fluid indicates a favorable course of the disease. With partial blockade of the subarachnoid space, a typical clinical picture of meningitis with relatively minor pleocytosis can be observed.
With purulent meningitis, the level of protein in the cerebrospinal fluid increases. It varies between 0.6-10 g/l. As the cerebrospinal fluid is freed from microorganisms, it decreases. A high concentration of protein is observed in severe forms of meningitis. If a high level of protein is detected during the recovery period, this indicates an intracranial complication. A particularly unfavorable prognostic sign for meningitis is the combination of low pleocytosis and high protein. The amount of glucose in the cerebrospinal fluid during purulent meningitis is below 3 mmol/l. The ratio of cerebrospinal fluid glucose to blood glucose levels in 70% of patients is less than 0.31. A favorable prognostic sign is an increase in glucose content in the cerebrospinal fluid.
In case of tuberculous meningitis, bacterioscopic examination of the cerebrospinal fluid may give a negative result. A characteristic sign of tuberculous meningitis is the precipitation of a sample of cerebrospinal fluid taken during standing within 12-24 hours. The sediment is a delicate fibrin cobweb-like mesh in the form of an overturned Christmas tree. Sometimes it can be rough flakes. In most cases, tuberculosis bacilli are found in the sediment.
With tuberculous meningitis, the cerebrospinal fluid is transparent and has no color. Pleocytosis can vary over a wide range - from 0.05. Up to 3.0×109/l. If treatment is not carried out aimed at destroying Mycobacterium tuberculosis, then the number of cells in the cerebrospinal fluid constantly increases throughout the disease. A day after the first lumbar puncture, a second procedure is usually performed. CSF samples obtained during repeat lumbar puncture often show a decrease in cells.
In most cases, lymphocytes predominate in the cerebrospinal fluid during tuberculous meningitis. There are cases when, at the onset of the disease, pleocytosis is lymphocytic-neutrophilic in nature. An unfavorable prognostic sign is the presence of a large number of monocytes and macrophages in the cerebrospinal fluid. The protein concentration in tuberculous meningitis is always increased to 2-3 g/l. Its level increases before the onset of pleocytosis and decreases after a significant decrease. Biochemical studies of cerebrospinal fluid in tuberculous meningitis early reveal a decrease in glucose levels to 0.83-1.67 mmol/l. Some patients experience a decrease in chloride concentrations in the cerebrospinal fluid.
Meningococci and pneumococci have a characteristic structure, due to which they are identified using the express method during bacterioscopic examination of the cerebrospinal fluid, which is obtained during the first lumbar puncture. If the patient is examined within the first day after hospitalization, simultaneous bacterioscopic examination of the blood cerebrospinal fluid under a microscope gives 90% positive results.
With meningococcal meningitis, intracranial pressure first increases, then mild neutrophilic cytosis is detected in the cerebrospinal fluid, then changes characteristic of purulent meningitis are determined. In this regard, in every fourth case, the cerebrospinal fluid examined in the first hours of the disease does not differ from the norm. In case of inadequate therapy, the cerebrospinal fluid may be purulent, there is a high neutrophilic pleocytosis, an increased level of protein, the concentration of which in the cerebrospinal fluid reflects the severity of the disease. With adequate therapy, neutrophilic pleocytosis decreases and is replaced by lymphocytic.
In serous meningitis of a viral nature, the cerebrospinal fluid is transparent, and slight lymphocytic pleocytosis is noted. In some cases, in the initial stages of the disease, an increased content of neutrophils is detected in the cerebrospinal fluid. This indicates a more severe course of the disease and has a less favorable prognosis. With serous meningitis, protein levels may be within normal limits or moderately elevated. In some patients, protein concentrations are reduced due to excess cerebrospinal fluid production.
Symptoms of meningitis in adults
Signs of meningitis can be divided into nonspecific and specific. The appearance of specific symptoms is characteristic of meningitis of a certain etiological nature.
Nonspecific symptoms
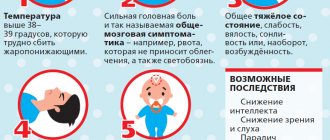
- Decreased performance, weakness, increased fatigue;
- Heat;
- Adynamia (state of powerlessness);
- Pallor of the skin;
- Increased intracranial pressure due to increased volume of cerebrospinal fluid (hereinafter referred to as CSF).
Specific symptoms of meningococcal meningitis
- Cephalgia;
- Redness of the posterior wall of the oropharynx;
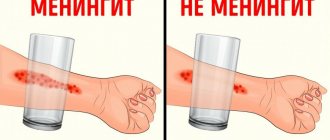
- Hemorrhagic rash formed due to damage to blood vessels;
- Photophobia;
- Psychomotor agitation;
- Hyperacusis (increased sensitivity to sounds);
- Prolonged vomiting;
- Delusional state, hallucinatory phenomena;
- Convulsive syndrome;
- Stiff neck;
- Waterhouse-Friderichsen syndrome, which is a hemorrhage in the adrenal glands in the clinic;
- Swelling of the brain due to compression of brain tissue by expanded liquor spaces;
- Tachycardia, hypotension, shortness of breath - these symptoms occur with meningococcal sepsis.
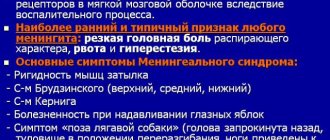
Meningeal symptoms
- Upper, zygomatic, pubic, lower Brudzinski's symptoms
- Kernig's symptom manifests itself in the fact that the patient cannot fully straighten the leg at the knee joint, which was in a bent state at the hip.
Serodiagnosis of viral meningitis
Unlike bacteria, viruses are very difficult to detect in biological fluids. Often, the diagnosis of a viral infection is made based on the difference in the results of serological tests in the acute period of the disease and during recovery. The antibody titer can be determined in the cerebrospinal fluid. This method is used to clarify the nature of the disease. In most viral meningitis, antibodies to the virus are produced in the cerebrospinal fluid, therefore the ratio of specific antibodies in the cerebrospinal fluid and blood serum increases. If the ISCT is greater than or equal to 1.5, this indicates a higher relative content of specific immunoglobulins in the cerebrospinal fluid than in the serum, and thus the infectious nature of meningitis.
Oligoclonal immunoglobulins are detected by agarose gel electrophoresis or isoelectric focusing of cerebrospinal fluid gamma globulins. These immunoglobulins appear in meningitis caused by the human immunodeficiency virus, human T-lymphotropic virus type 1, Varicella-Zoster virus, and mumps virus. Identification of oligoclonal immunoglobulins helps doctors make a differential diagnosis of infectious meningitis caused by enteroviruses, arboviruses, and herpes simplex virus, in which they are usually absent.
The hat has nothing to do with it
Often the last argument of mothers who want to convince their children to wear a hat in winter is precisely this threat: “Or else you’ll catch meningitis!” Without arguing that a hat is necessary in cold weather, we must still admit that the cause of the disease is viruses or bacteria. However, you still need to beware of hypothermia so as not to provoke a drop in immunity, due to which the body’s susceptibility to pathogens increases.
Article on the topic Hit to the head. Who is at risk of viral meningitis and how to escape from it
Other studies for meningitis
In patients with symptoms of meningitis, it is necessary to identify or exclude the enteroviral nature of the disease. For this purpose, laboratory assistants at the Yusupov Hospital perform a polymerase chain reaction. The results of the study are received within a few hours. To determine the pathogen, the semi-nested polymerase chain reaction technique is often used for the parallel determination of meningococci, Haemophilus influenzae and streptococci.
Instrumental diagnostic methods for meningitis are used for neuroimaging and functional assessment of the state of brain structures and blood flow, timely diagnosis of intracranial complications, and sensorineural hearing loss. All patients with suspected meningitis upon admission to the neurology clinic undergo ophthalmoscopy with assessment of the condition of the fundus. Young children with an open large fontanelle undergo neurosonography.
If the blood supply is stable, computed tomography or magnetic resonance imaging is performed. Neuroimaging methods are necessary for differential diagnosis with other diseases of the central nervous system in the presence of focal neurological symptoms. The absence of pathological changes in the brain during tomography in the early stages of meningitis does not exclude the risk of development in the future. All patients with meningitis in the early stages of the disease undergo recording of short-latency auditory evoked potentials to exclude or early detect sensorineural hearing loss. In order to get tested for meningitis, call the Yusupov Hospital.
Who is guilty?
Meningitis (inflammation of the meninges) most often affects children (especially under 5 years of age). Children make up 70% of those affected by this disease.
Meningitis can be viral and bacterial; in rare cases, fungi and protozoa can lead to its development. Viral meningitis, which has a huge number of pathogens, is the most common. As a rule, it is easier to treat.
Bacterial (purulent) meningitis also has many pathogens. Among them are meningococci, pneumococci, Hemophilus influenzae type b, streptococcal bacteria of group B. This type of disease often has more pronounced symptoms and gives dangerous complications.
Meningitis can also develop secondarily as a complication resulting from another disease, for example, mumps (mumps), tuberculosis, tick-borne encephalitis, Lyme disease, enterovirus infection, syphilis.
Article on the topic
You'll remain a fool! What is the difficulty of diagnosing and treating meningitis?