General concept
Meningitis is defined as an acute inflammatory process caused by any infection entering the body. This disease affects people of all age groups.
Reference! The incidence of meningitis in newborns varies from 0.02 to 0.2% . This indicator is influenced by the baby’s weight and general health.
There are several types of meningitis:
- serous. It is characterized by a predominance of lymphocytes in the cerebrospinal fluid;
- purulent. Here, neutrophilic pleocytosis is paramount. In turn, it is divided into two subspecies - primary and secondary. They differ in the places where the infection primarily occurs.
According to statistics, the most common form is secondary purulent and viral meningitis.
A fungal type of disease is also isolated, which occurs in patients with reduced immunity.
If rashes are diagnosed during an illness, this may indicate the probable cause of its appearance.
For example, meningitis is characterized by a skin rash.
Meningitis
Encephalitis
Fungus
Vomit
Rubella
Measles
24572 07 June
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Meningitis: causes, symptoms, diagnosis and treatment methods.
Definition
Meningitis is an infectious inflammation of the meninges of the brain and spinal cord, accompanied by intoxication, fever, increased intracranial pressure syndrome, meningeal syndrome, as well as inflammatory changes in the cerebrospinal fluid.
The meninges are connective tissue membranes that cover the brain and spinal cord. There are dura mater, arachnoid and pia mater.
The dura mater of the brain has a dense consistency and thickness of 0.2-1 mm; in places it fuses with the bones of the skull. The arachnoid membrane is a thin, translucent, non-vascular connective tissue plate that surrounds the brain and spinal cord. The soft shell is a thin connective tissue plate directly adjacent to the brain, corresponds to its relief and penetrates into all its recesses. In its thickness is the vascular network of the brain.
The most common inflammation is inflammation of the pia mater, and the term “meningitis” is used.
Causes of meningitis
The meninges can be involved in the inflammatory process primarily and secondary. Meningitis that occurs without a previous general infection or disease of some other organ is called primary. Secondary meningitis develops as a complication of an existing infectious process. Secondary ones include tuberculous, staphylococcal, pneumococcal meningitis. The primary ones are meningococcal, primary mumps, enteroviral meningitis and others.
The disease is transmitted by airborne droplets, household contact or nutrition.
Purulent inflammation of the meninges can be caused by various bacterial flora (meningococci, pneumococci, and less commonly, other pathogens). The cause of serous meningitis is viruses, bacteria, fungi.
According to the forecast, the most dangerous is tuberculous meningitis, which occurs when there is a tuberculous lesion in the body. The development of the disease occurs in two stages. At the first stage, the pathogen, through the bloodstream, infects the choroid plexuses of the ventricles of the brain with the formation of a specific granuloma in them. In the second, inflammation of the arachnoid and soft membranes is observed (as a rule, the membranes of the base of the brain are affected), which causes acute meningeal syndrome.
The development process of meningococcal meningitis also consists of several stages:
- contact of the pathogen with the mucous membrane of the nasopharynx;
- entry of meningococcus into the blood;
- penetration of the pathogen through the blood-cerebrospinal fluid barrier, irritation of pia mater receptors by toxic factors and inflammation.
The course of the infectious process depends on the pathogenic properties of the pathogen (the ability to cause disease) and the state of the human immune system.
Previous viral diseases, sudden climate change, hypothermia, stress, concomitant diseases, therapy that suppresses the immune system can be significant for the occurrence and course of meningitis.
Classification of the disease
According to the type of pathogen:
- Viral meningitis (influenza, parainfluenza, adenovirus, herpes, arbovirus (tick-borne), mumps, enterovirus ECHO and Coxsackie).
- Bacterial meningitis (meningococcal, tuberculous, pneumococcal, staphylococcal, streptococcal, syphilitic, brucellosis, leptospirosis).
- Fungal (cryptococcal, candidiasis, etc.).
- Protozoal (toxoplasmosis, malaria).
- Mixed.
According to the nature of inflammation:
- Serous.
- Purulent.
According to the mechanism of occurrence:
- Primary.
- Secondary.
With the flow:
- Spicy.
- Subacute.
- Fulminant.
- Chronic.
By severity:
- Easy.
- Medium-heavy.
- Heavy.
According to the prevalence of the process:
- Generalized.
- Limited.
According to the presence of complications:
- Complicated.
- Uncomplicated.
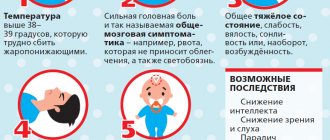
Symptoms and syndromes of meningitis
There are a number of syndromes common to all meningitis:
- meningeal syndrome - manifested by rigidity (increased tone) of the neck muscles and long back muscles, hypersthesia (increased sensitivity) of the sensory organs, headache, vomiting, changes in the cerebrospinal fluid;
- cerebral syndrome - manifested by drowsiness, impaired consciousness, nausea, vomiting, dizziness, psychomotor agitation, hallucinations;
- asthenovegetative syndrome – manifested by weakness, decreased ability to work;
- convulsive syndrome;
- general infectious syndrome - manifested by chills and fever.
Meningococcal meningitis ranks first among purulent meningitis.
Its incubation period ranges from 1 to 10 days, with an average of 2-4 days. The disease usually begins acutely against the background of complete health or shortly after nasopharyngitis. Patients can indicate not only the day, but also the hour of illness; they are worried about chills, body temperature above 38℃, severe bursting headache, aggravated by any noise and movement of the head. Patients may experience pain in various parts of the body, and touching causes excruciating sensations. Vomiting is not associated with food intake and does not bring relief. Soon, stiffness of the neck and long back muscles sets in. Patients take a “meningeal” position. Infants cry constantly, they may experience bulging fontanelles and gastrointestinal disorders. Pneumococcal meningitis, as a rule, is observed in young children against the background of an existing pneumococcal process (pneumonia, sinusitis).
With streptococcal meningitis, hepatolienal syndrome (enlarged liver and spleen), renal failure, adrenal insufficiency, petechial rash (hemorrhages due to damage to the capillaries, as a result of which blood, spreading under the skin, forms round spots, the size of which does not exceed 2 mm).
Purulent meningitis caused by Pseudomonas aeruginosa and fungi are rare. The diagnosis is established only after additional laboratory tests.
Serous tuberculous meningitis is characterized by a gradual onset, although in rare cases it can manifest itself acutely. At the onset of the disease, patients complain of fatigue, weakness, irritability, and sleep disturbances. The temperature is usually no higher than 38℃, and there is an intermittent moderate headache. On the 5-6th day of illness, the temperature rises above 38℃, the headache intensifies, nausea, vomiting, and drowsiness appear. Unconsciousness develops quickly. A divergent strabismus, a low position of the upper eyelid in relation to the eyeball, and pupil dilation may be observed.
When diagnosing mumps meningitis, it is important to identify recent contact with someone with mumps.
Clinical manifestations of damage to the meninges may develop even before the enlargement of the salivary glands.
Enteroviral meningitis is characterized by two- and three-wave fever with intervals between waves of 1-2 or more days. Other manifestations of enterovirus infection are almost always observed (muscle pain, skin rash, herpangina).
For the diagnosis of measles and rubella meningitis, an indication of contact with a patient with these diseases, as well as typical clinical symptoms of measles or rubella, is of great importance.
Diagnosis of meningitis
To confirm the diagnosis of meningitis, the doctor may prescribe a set of laboratory and instrumental studies:
- clinical blood test with determination of hemoglobin concentration, number of erythrocytes, leukocytes and platelets, hematocrit and erythrocyte indices (MCV, RDW, MCH, MCHC), leukoformula and ESR (with microscopy of a blood smear in the presence of pathological changes);
Features of the disease in infants
In newborns, purulent meningitis is mainly detected. It appears due to:
- sepsis;
- trauma during childbirth;
- untimely birth of the fetus.
Often the infection enters the body through the umbilical vessels or through the placenta. The last case is possible when the mother, while pregnant, suffered from pyelitis.
The causative agents of meningitis are:
- coli;
- staphylococci;
- streptococci.
In those who are breastfed, meningitis is considered a severe form of the disease.
In 50% of cases, death is recorded. Adult patients survive in 90% of cases.
Complete lethargy or excessive excitability - these manifestations are very similar to other pathologies.
The diagnosis is confirmed exclusively in a full hospital setting after receiving preliminary results of a cerebrospinal fluid analysis.
It is not always possible to completely cure a baby. A large percentage of complications manifests itself in the form of:
- epilepsy;
- CNS disorders;
- mental retardation;
- paralysis
Such children have to be constantly monitored by doctors and undergo tests to avoid relapse.
If we talk about purulent meningitis, it is an inflammation that forms in the meninges. This subtype ranks first among CNS lesions in newborns. The disease often leads to disability and even death.
It is quite difficult to recognize the disease. A child may be admitted to a medical facility with a common ARVI. Some children experienced local infectious processes.
Meningitis in children
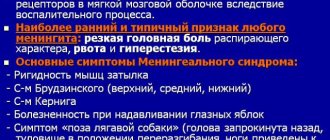
For all meningitis, meningeal syndrome , which includes cerebral, local symptoms and changes in the cerebrospinal fluid. General cerebral symptoms are characterized by manifestations in the form of a general reaction of the brain to irritation. Local symptoms occur due to swelling and damage to the cranial nerves. Sometimes symptoms of loss are observed.
A mandatory sign of meningitis is inflammatory changes in the cerebrospinal fluid with cell-protein dissociation (a significant increase in cells in the cerebrospinal fluid).
The meningeal symptom complex includes:
Increase in body temperature to high levels. With tuberculous meningitis, high fever is usually not observed.
Headache. In its pathogenesis, irritation of the receptors of the meninges is important. Headache is the main constant symptom of the disease. It is usually diffuse, intensified by sudden movements, sound and light stimuli.
Vomiting occurs without nausea and is not associated with food intake. More often it occurs when changing body position. After vomiting, the headache does not decrease.
Muscle contracture - rigidity of the muscles of the neck and back, Kernig and Brudzinski symptoms. Young children may experience the hanging sign (Lesage). Muscle contracture during meningitis occurs due to increased activity of the reflex apparatus and irritation of the roots due to increased pressure of the cerebrospinal fluid.
Autonomic disorders , which include dissociation between body temperature and pulse, pupillary disorders, skin petechiae, mental disorders (disorder of consciousness, asthenia).
Motor disorders , manifested in the form of symptoms of damage to the motor cranial nerves, focal epileptic seizures due to irritation of the motor cortex.
Sensitivity disorders , which occur in the form of general hyperesthesia. It is based on irritation of the dorsal roots and intervertebral nodes.
Pachymeningitis
Pachymeningitis is divided into cerebral (inflammation of the dura mater of the brain) and spinal (inflammation of the dura mater of the spinal cord). Based on the nature of the lesion, cerebral pachymeningitis is divided into serous, hemorrhagic and purulent . Serous pachymeningitis occurs in various infections and is characterized by a low-symptomatic or asymptomatic course (headache, vague meningeal symptoms, as well as signs of compression of the brain by the edematous membrane). Hemorrhagic pachymeningitis is characterized by the presence of hemorrhage (a condition in which hemorrhage or bleeding occurs) in the dura mater, which is clinically manifested by headache, focal and meningeal symptoms, and agitation. Occurs with atherosclerosis and hypertension. Purulent pachymeningitis is usually secondary and is associated with a primary purulent rhinootogenic infection. Purulent pachymeningitis is characterized by headache, vomiting, congestive changes in the fundus and blood changes may be observed.
Spinal pachymeningitis can be serous or purulent . Serous is characterized, as a rule, by a benign course, purulent is associated with the presence of purulent foci in the body (furunculosis, osteomyelitis, etc.).
Among spinal pachymeningitis, the following are distinguished.
Spinal epiduritis (inflammation between the layers of the membrane). In this case, the membranes at the level of the upper thoracic region are affected. Patients experience clinical symptoms of spinal cord compression (radicular pain, motor, sensory and pelvic disorders).
Chronic hyperplastic epiduritis. It is most often caused by spinal injury. The clinic is characterized by limited mobility of the spine, radicular pain in the spine. Remissions are characteristic; the protein content in the cerebrospinal fluid is increased.
Cervical hypertrophic syphilitic pachymeningitis occurs as a type of moderate compression of the spinal cord in the neck. In this case, radicular pain, symptoms of compression in the form of flaccid paresis of the arms, spastic paresis of the lower extremities, conduction-type sensitivity disorders, and dysfunction of the pelvic organs are observed.
Tuberculous spinal pachymeningitis, in which clinical symptoms depend on the degree of damage to the spinal cord.
Arachnoiditis
The following forms of the disease are distinguished: adhesive (formation of adhesions), cystic (presence of cysts), cystic-adhesive, or mixed arachnoiditis. Based on the causes of occurrence, arachnoiditis is divided into rheumatic, post-influenza, tonsillogenic, traumatic and toxic. Depending on the course, acute, subacute and chronic arachnoiditis are considered. convexital arachnoiditis is distinguished (damage to the frontal, parietal, temporal lobes and central gyri), basal and posterior cranial fossa.
Arachnoiditis can also be focal and widespread. Pathological anatomy is characterized by fibrosis and proliferation of connective tissue.
Clinical symptoms are quite wide: headache, nausea, vomiting, epileptic seizures, changes in the fundus. Shell symptoms may be absent or mild. Focal neurological symptoms depend on the location of the lesion. With a pronounced diffuse process, intracranial pressure increases and dropsy develops.
Convexital arachnoiditis is a predominant lesion of the soft membranes of the convexital surface of the cerebral cortex. In this case, the leading clinical symptoms are dysfunction of the frontal, temporal, parietal lobes and the region of the central gyri. The clinical picture is dominated by subjective complaints (headache accompanied by nausea and vomiting, sweating, dizziness, etc.) over objective symptoms (unevenness of tendon reflexes, pathological reflexes on the side opposite to the lesion, convulsive seizures, etc.).
Optochiasmal arachnoiditis is characterized by predominant damage to the soft membranes of the brain in the area of the optic chiasm (the point at the base of the brain where the fibers of the 2 optic nerves cross and diverge) and the intracranial part of the optic nerves. The leading symptom in the clinic is a decrease in visual acuity and changes in visual fields. Individual sections of the visual fields may fall out, and concentric narrowing of the visual fields, hemianopsia and blindness may also occur. Along with this, autonomic disorders (sleep disturbances, changes in carbohydrate and water-salt metabolism, etc.) are common.
Arachnoiditis of the posterior cranial fossa appears due to damage to the soft membranes of the brain in the area of the lateral and large cistern, as well as in the craniospinal region with possible disruption of the circulation of cerebrospinal fluid in the posterior cranial fossa. The course of the disease is severe, with meningeal and cerebral clinical signs, disorders of brain stem function, cerebellar disorders, congestion in the fundus, and damage to the cranial nerves.
Arachnoiditis of the cerebellopontine angle occurs most often as a result of otitis media. The clinical picture is characterized by clearly defined focal symptoms with weak cerebral symptoms. Focal symptoms are manifested by damage to the cranial nerves, cerebellar disorders, and mild pyramidal disorders. Pyramidal disorders occur on the side opposite to the lesion, cerebellar disorders on the same side.
In the cerebellopontine angle there are also tumor processes that are benign. Cranial nerves are often involved in the process, and pyramidal and cerebellar disorders may be observed. Treatment of the tumor is surgical.
Differential diagnosis of arachnoiditis and tumor presents significant difficulties. Arachnoiditis, unlike a tumor, is characterized by a remitting course and less severe focal neurological symptoms. However, cystic arachnoiditis and brain tumor are space-occupying processes that may have a similar clinical picture.
Spinal arachnoiditis can be adhesive, cystic or mixed. According to prevalence – diffuse and focal. Adhesive spinal arachnoiditis is accompanied mainly by radicular symptoms. Cystic are characterized by the clinical appearance of an extramedullary tumor.
Leptominengitis
Meningitis affecting the soft membrane of the brain. This type is divided into two volumetric groups: purulent and serous , depending on the nature of the inflammation process and changes in the cerebrospinal fluid. The development of the disease has an acute, subacute and chronic course. Meningitis is divided into primary and secondary. Primary meningitis can be purulent (meningococcal, pneumococcal, etc.) and serous (lymphocytic choriomeningitis, meningitis caused by ECHO and Coxsackie viruses, etc.). Secondary meningitis manifests itself as a complication of purulent otitis media, furunculosis, lung abscess, open head injury, and general infections (tuberculosis, mumps, syphilis, etc.).
Purulent meningitis
Purulent meningitis is a group of diseases caused by various pathogens (meningococci, streptococci, staphylococci, Haemophilus influenzae Afanasyev-Pfeiffer, Escherichia coli, Pseudomonas aeruginosa, fungi, salmonella, etc.), affecting mainly the soft membranes of the brain and spinal cord. Children of all ages, especially young ones, are susceptible to the disease, this is due to insufficient development of immunity and a weakening of the blood-brain barrier.
Features of the development of purulent meningitis in newborns
The entry points for infection are the umbilical vessels, the infected placenta when the mother has pyelitis or pyelocystitis. Predisposing factors – prematurity, birth trauma, etc.
The most common pathogens are Escherichia coli, staphylococci, and streptococci.
Clinical manifestations are characterized by severity, dehydration, gastrointestinal disorders, and the absence of a significant increase in body temperature.
High mortality rate (50-60%). The clinical picture may include hyperexcitability syndrome (the child is restless, screams monotonously, burps, throws his head back, a large fontanelle may bulge) and lethargy or apathy syndrome (the child is lethargic, reduced motor activity, weak cry, refuses to breastfeed). Recovery of newborn children is often incomplete; there are severe organic lesions of the central nervous system (hydrocephalus, epilepsy, mental retardation, paralysis and paresis of cranial nerves and limbs).
- Meningococcal meningitis
Infection with meningococcus occurs through the mucous membrane of the nasopharynx. After which meningococcus penetrates the blood and lymphatic system, where it develops. Meningococcal meningitis is manifested by the following clinical symptoms: high body temperature, severe intoxication, dizziness, vomiting, pale complexion, purulent nasal discharge, fever, skin rashes, bleeding and hemorrhage, eye pain, sometimes severe abdominal pain, increased sweating.
- Pneumococcal meningitis
Meningitis is caused by pneumococci of various serological types and is characterized by severe disease and high mortality. In 40% of cases it is primary, i.e. occurs in healthy children. In other cases, the disease develops against the background of otitis, sinusitis, and pneumonia. Young children are more often affected. Patients experience high body temperature, toxicosis, loss of consciousness, convulsions, damage to the cranial nerves, as well as paralysis and paresis of the limbs. The disease often takes a protracted course, and in the absence of treatment, death can occur on the 5-6th day.
- Meningitis caused by Haemophilus influenzae Afanasyev-Pfeiffer
Meningitis affects weakened children suffering from frequent catarrh of the upper respiratory tract, otitis media, and pneumonia. Perhaps both an acute onset and a gradual one. The course is sluggish, wave-like, gastrointestinal disorders, pneumonia, and toxicosis may occur. With timely and correct treatment, the course is favorable.
- Staphylococcal meningitis
This type of meningitis is the most unfavorable and has a high mortality rate. It is usually secondary and occurs against the background of abscesses, chronic pneumonia, osteomyelitis of the skull and spine, and sepsis. The clinical picture of meningitis is masked by the severe septic condition of the patient. A feature of staphylococcal meningitis is blockage of the cerebrospinal fluid pathways (hydrocephalus), as well as abscess formation. Difficulties in therapy are aggravated by the resistance of staphylococcus to antibiotics.
- Escherichia meningitis
The causative agent is pathogenic strains of Escherichia coli. This type of meningitis is rare and is mostly common in young children. In newborns it develops as a complication after sepsis. Escherichia meningitis is predisposed by prematurity, birth trauma, previous infectious and somatic diseases, such factors influence brain damage. Infection occurs through the umbilical vessels, infected placenta when the mother has pyelocystitis or pyelitis. Symptoms are expressed by a sharp deterioration of the condition against the background of elevated body temperature, vomiting, anorexia, and increasing intoxication. Newborns experience attacks of clonicotonic convulsions, muscle hypo- and atonia, followed by tonic tension of the limbs, indifference, their reflexes are depressed, and the fontanel may be sunken. Dysmeitic phenomena are observed in the form of loose, frequent stools.
The current is severe. Purulent foci may appear in other organs, dystrophy increases early, and arterial hypotension and exicosis often develop. Possible severe organic damage to the central nervous system.
- Salmonella meningitis
Can be caused by any Salmonella serotype. The disease occurs infrequently, usually in children during the first 6 months. life and newborns, but it is also possible in older children, adolescents and even adults. In infants, the disease develops gradually, peptic symptoms are moderate or absent. Characterized by toxicosis, septicemia or septicopyemia, enlarged liver and spleen, rash, hyperleukocytosis in the blood. The development of cerebral hypotension is likely. In older children, meningitis develops acutely against the background of a typical clinical picture of gastroenteritis. The course of the disease is severe with frequent deaths.
- Meningitis caused by Pseudomonas aeruginosa
In most cases, it occurs against the background of sepsis, which develops as a superinfection after surgery, and occurs in all age groups. The increase in its cases is associated with the use of antibiotics, leading to dysbiosis, when only resistant species of bacteria survive, including Pseudomonas aeruginosa.
The clinical picture shows signs of severe meningoencephalitis with a tendency to develop hydrocephalus. The course of the disease is often long-term, the prognosis is unfavorable. The outcome of the disease is largely determined by the time of initiation of treatment and the correct selection of antibiotics, to most of which the pathogen is resistant.
- Streptococcal meningitis
A rare disease, most often observed in newborns as a manifestation of sepsis, but can occur in all age groups. The course and clinical picture are similar to those of meningococcal meningitis; In patients with septic endocarditis, meningitis begins suddenly and is accompanied by focal neurological symptoms. Patients often experience vascular damage, leading to subarachnoid hemorrhages.
- Listeria meningitis
Occurs in all age groups. Newborns are more likely to get sick, in whom meningitis may be one of the manifestations of septicemia. The disease develops acutely, meningeal syndrome is usually well expressed, and symptoms of focal damage to the central nervous system are often observed - meningoencephalitis. Adequate timely therapy usually leads to complete recovery.
- Meningitis caused by Proteus, Klebsiella (Friedlander's bacillus)
This type of disease is very rare. In most cases, this is a manifestation of dysbiosis, which develops as a result of irrational use of antibiotics. The development of the disease is preceded by septicemia; children usually get sick in the first months of life. The primary source of infection in the case of meningitis caused by Klebsiella can be pneumonia, purulent otitis, and tracheobronchitis. This meningitis is sometimes preceded by neurosurgical intervention. Clinical symptoms may be mild. The course is severe and residual effects are often observed.
Serous meningitis
Serous meningitis occurs with serous inflammation of the soft meninges. Lymphocytic pleocytosis is observed in the cerebrospinal fluid. There are 4 possible clinical forms: serous meningitis, meningoencephalitis, clinically asymptomatic meningitis, meningism. Children in the first years of life often experience lethargy, weakness, drowsiness, delirium and hallucinations. With meningoencephalitis, focal symptoms are associated: hemi- and monoparesis of the limbs, ataxia, damage to the cranial nerves. Approximately 15% of patients experience pancreatitis and increased diastase content in the urine. In school-age boys, orchitis occurs simultaneously with meningitis or a little later - swelling of the testicles, hyperemia and swelling of the scrotum, increased body temperature. The presence of orchitis and pancreatitis confirms the etiology of meningitis.
Enteroviral meningitis caused by the Coxsackie and ECHO viruses is characterized by high co-infectivity, focality and mass distribution. They are characterized by myalgia - muscle pain, often in the abdominal muscles. The clinical picture is characterized by increased body temperature, facial hyperemia with a pale nasolabial triangle, pharynx hyperemia, conjunctivitis, injection of scleral vessels, and a polymorphic rash. Herpetic rashes are often observed. As a rule, there is a sharp headache, vomiting, and meningeal symptoms. In the cerebrospinal fluid, lymphocytic pleocytosis can be noted, the protein content is normal, the pressure is increased. Focal symptoms are usually mild and disappear quickly. The course of the disease is benign.
- Tuberculous meningitis
It occurs against the background of a primary tuberculosis focus in the body. Clinical symptoms are characterized by increasing intoxication, lethargy, workload, and an increase in temperature to febrile levels. Pleocytosis is always mixed with a predominance of lymphocytes, the fluid is xanthochromic, the glucose content in the cerebrospinal fluid is reduced due to the activity of tubercle bacilli.
Fungal meningitis
Various fungi that cause meningitis can be present in the body both short-term and long-term. Meningitis is most often caused by yeast-like fungi. The first encounter with fungi (causing candidiasis can occur in utero, during passage through the birth canal, or during breastfeeding). Infants in the first months of life and premature newborns are most often affected. The disease is usually preceded by sepsis, surgical interventions with long-term antibiotic treatment.
- Candidal meningitis
It is distinguished by a sluggish, subacute course, and can be detected incidentally during the study of cerebrospinal fluid in children with progressive hydrocephalus or convulsive syndrome. The clinical picture is characterized mainly by lethargy, adynamia, pallor of the skin, an unstable rise in temperature to 37.5-38 ° C, decreased appetite, and sometimes vomiting. Meningeal symptoms are mildly expressed or may be absent, bulging and tension of the large fontanelle is not always noted, and at a later date progressive hydrocephalus is possible.
Without appropriate therapy, mortality reaches 100%, with children dying within 1-3 months. either from cachexia or from the addition of a secondary infection. The timing of the start of treatment determines the outcome, however, even in the case of specific therapy, the course of the disease is long, and the majority of surviving children develop hydrocephalus. Note that candidal meningitis is often combined with staphylococcal infection. In this case, the clinical picture of the disease is more pronounced.
Causes
The causes of the disease can be provoked by different pathogens. If we talk about babies, they are as follows:
- hemophilus influenzae;
- pneumococcus;
- meningococcus;
- enterobacteria;
- microbacteria tuberculosis.
Meningitis is transmitted by household contact, airborne droplets, vertical, transmissive, alimentary and waterways . The disease develops against the background of a difficult pregnancy and difficult childbirth.
Reference! Outbreaks of meningitis in older children tend to be seasonal. Typically the peak occurs in winter and spring.
Symptoms in children
The clinical picture of the disease is represented by general neurological symptoms. These include the following:
- decreased physical activity;
- general lethargy;
- increased drowsiness;
- frequent vomiting;
- refusal of breast milk;
- signs of suffocation.
Newborns can suffer from temperatures exceeding 39 degrees. In some, the signs can be recognized if, when tilting the head back, convulsions appear or an increased pulsation of the fontanel is observed.
How does meningitis occur in a low-weight child? Here the clinical picture is completely different. It will make itself felt especially at the peak of the disease. At risk, first of all, are infants born prematurely and those who are already given antibiotics in the maternity hospital to maintain viability.
Important! The disease itself is characterized by rapid development. Depending on age and weight, it can also be protracted. All this creates a number of difficulties for doctors in timely and correct diagnosis of the disease.
Serous meningitis
Sometimes the doctor's way of thinking seems at least strange to parents.
Phone call. — Doctor, the child has been vomiting 5 times since the morning, the temperature is 39. What should I do? — Did the child have diarrhea? - the doctor clarifies. - Yes. - Oh, well then everything is fine.
The patient's mother is surprised. How is this “good”? Vomiting and fever are not enough for us, but also diarrhea! Is the doctor completely crazy? No. The fact is that if, in the presence of vomiting, there is also loose stool, then the differential diagnosis is greatly facilitated. Of course, there are exceptions, but in general in such a situation it is very likely that it is an intestinal infection. It’s clear that she needs to be treated and we need to figure out what she’s like. But at least for the doctor, this situation is much simpler than if the patient does not have diarrhea but is vomiting.
A typical case from practice
Here's an example. Summer. A boy, a football player, 11 years old, became acutely ill. Repeated vomiting, headache, low temperature - about 38. Was there diarrhea? No, today the chair is decorated once. The abdomen does not hurt, it is calm on palpation. It doesn't even purr.
Treatment methods
Treatment of meningitis is a very long and serious process. Attempting to administer any medications at home is strictly prohibited.
Important! The disease is treated strictly in a hospital. Folk remedies will not help get rid of the disease . All therapy should begin with establishing the root cause of meningitis.
When doctors diagnose a bacterial infection, they will most likely prescribe broad-spectrum antibiotics. As a rule, medications are administered in maximum dosages over a long course. Change medications every 12 weeks.
When the disease takes the form of a viral and fungal infection, then antiviral and antifungal drugs are administered. All injections in this case are intravenous.
If there is a fungal or viral infection, the baby may recover in 14-20 days. The bacterial type of meningitis takes the longest to treat. In general, the course depends on the severity of the disease and the general condition of the body.
Possible effects in infants
This extremely dangerous disease often results in the most negative consequences for the baby. Sometimes even long-term therapy becomes powerless. The consequences include:
- blindness;
- deafness;
- bleeding disorders;
- mental retardation;
- Within two years, a brain abscess may occur.
Reference! Infants die in 30-50% of cases if a brain abscess is detected.
Even if the child manages to survive, complications will be felt for a long time. When the disease is mild, the course of treatment is several weeks if it started on time.
We invite you to watch an interesting video on the topic:
Forecast
The prognosis should be determined based on the etiology, premorbid background and severity of the disease. The adequacy and timeliness of therapy is of no small importance.
Modern medicine has reached such heights that there are fewer and fewer deaths among infants. As for the residual period of meningitis, hypertensive and asthenic syndromes are more often recorded in children.
Important! Infants who have had this disease should be registered with a neurologist, infectious disease specialist, or pediatrician.
Bacterial meningitis
If bacterial meningitis is suspected, cerebrospinal fluid should be examined within the first 30 minutes, and if the results confirm the diagnosis of acute bacterial meningitis, antimicrobial therapy should be initiated depending on the results of Gram staining or bacterial antigen tests. However, if no causative agent can be identified or lumbar puncture cannot be performed within the first 30 minutes, empirical antimicrobial therapy should be started (adjusted based on the patient's age) as soon as blood samples are obtained. In patients with suspected bacterial meningitis who have local neurological manifestations or papilledema, a computed tomography scan (CTS) should be performed before lumbar puncture to rule out an intracranial neoplasm. In such a situation, performing a lumbar puncture is associated with the risk of cerebral hernia. However, performing CTS requires additional time, so antimicrobial therapy should be started immediately, given the risk of delaying treatment. Of course, the value of cerebrospinal fluid culture in patients receiving antimicrobial treatment (if lumbar puncture is delayed until CTS results are available) is significantly reduced, but the results of cerebrospinal fluid parameters, Gram stains, bacterial antigen tests, and blood samples obtained before treatment are likely to confirm the presence or absence of bacterial meningitis.
Recommendations regarding which drug should be empirically prescribed in an emergency situation for suspected bacterial meningitis have changed due to the development of resistance to a number of drugs in microorganisms. Although N. meningitidis strains exhibit relative resistance to penicillin G at minimum inhibitory concentrations (MICs) of 0.1 to 1 μg/ml, patients in whom these isolates are found improve after standard penicillin therapy. Moreover, the prevalence of penicillin-resistant meningococci has not yet reached levels of serious concern everywhere. Thus, in the USA it remains low and has not changed significantly over the past 10 years. For these reasons, we took into account changes in the susceptibility spectrum of H. influenzae type B and S. pneumoniae when making recommendations for empirical antimicrobial therapy.
H. influenzae type B If meningitis caused by H. influenzae is suspected, when prescribing empirical treatment, it must be taken into account that many strains produce P-lactamase; these strains accounted for 24% of all isolates in a US study between 1978 and 1981, and 32% in another US study in 1986. Resistance to chloramphenicol has also been described, with more than 50% of isolates being resistant in a report from Spain . Even in patients in whom chloramphenicol-susceptible isolates are found, the use of chloramphenicol is less preferable from a bacteriological and clinical point of view than the use of ampicillin, ceftriaxone, or cefotaxime for bacterial meningitis in childhood. The second-generation cephalosporin cefuroxime initially appeared to be as effective as the combination of ampicillin and chloramphenicol for bacterial meningitis in childhood, but its effectiveness has been questioned in more recent studies. Thus, in a study in which cefuroxime (Zinnacef, Zinnat, Ketocef) was compared with ceftriaxone in the treatment of bacterial meningitis in children, both regimens were effective, but with ceftriaxone it was much more likely to achieve CSF sterilization (0% versus 9% positive cultures after 24 h) and hearing impairment was less common (11% vs. 18%). Another randomized trial also compared cefuroxime with ceftriaxone in the treatment of bacterial meningitis in children; demonstrated faster CSF sterilization (2% vs. 12% positive cultures at 18–36 hours) and lower incidence of hearing loss (4% vs. 17%) in patients receiving ceftriaxone. This and other studies have confirmed that third-generation cephalosporins (especially cefotaxime or ceftriaxone) are as effective as ampicillin in combination with chloramphenicol for bacterial meningitis in children, predominantly caused by H. influenzae type B, and can be recommended as the drug of choice for empirical antimicrobial therapy for bacterial meningitis in children.
S. pneumoniae The need to take into account the spectrum of resistance to antimicrobial drugs has also led to changes in recommendations regarding empirical therapy for suspected pneumococcal meningitis, as strains have emerged that exhibit relative (MIC 0.1 - 1 μg/ml) or high (MIC greater than or equal to 2 µg/ml) resistance to penicillin G. Almost all resistant strains isolated from cerebrospinal fluid belong to serotypes 6, 14, 19 and 23; Most of the multidrug-resistant strains isolated in the United States have disseminated from the serotype 23 F clone, which was discovered in Spain back in 1978. The frequency of detection of penicillin-resistant pneumococci is increasing throughout the world. An American study conducted from 1979 to 1987 showed that 4.5% of pneumococcal strains showed relative or high resistance to penicillin; in a later study (1991 - 1992), 16.4% of pneumococcal isolates showed resistance to at least to one of the following antimicrobial drugs: penicillins, cephalosporins, macrolides, cotrimoxazole (Bactrim, Biseptol, Septrin) and chloramphenicol. Another American observation (1994) showed that the level of resistance to penicillin was about 20%. In Spain, the incidence of resistance increased from 6% in 1979 to 44% in 1989; the highest incidence was observed in Hungary (58% based on surveillance data from 1988 to 1989). The following factors have been reported to predispose to resistance: age of the patient (younger than 10 or older than 50 years), immunosuppression, prolonged hospital stay, children in day care, infection with serotypes 14 and 23, frequent or prophylactic use of antimicrobials (for example, to prevent inflammation of the medial ear).
Some alternative drugs for the treatment of meningitis caused by penicillin-resistant pneumococci have been tested only in vitro or in animal models, and we have chosen to limit the discussion to drugs that have undergone clinical trials. One such drug is chloramphenicol. However, resistance and clinical failure occur even in cases where the body is sensitive to chloramphenicol: in one study, 20 of 25 children showed a poor clinical response or had residual effects, and some even died. Although disc testing showed the sensitivity of the microorganism, the minimum bactericidal concentration of chloramphenicol for penicillin-resistant pneumococcal isolates was significantly higher than that for penicillin-sensitive isolates, so only subtherapeutic levels of bactericidal activity were achieved and treatment failed. Third-generation cephalosporins are considered the drug of choice for pneumococcal meningitis that exhibits relative resistance to penicillin, but there are reports of therapy failure and pneumococcal strains unexpectedly demonstrating resistance to these cephalosporins (MIC increased from 4 to 32 μg/ml or more).
Dexamethasone Some people with acute bacterial meningitis need immediate treatment with dexamethasone. This is done to mitigate the inflammatory response in the subarachnoid space associated with antibiotic-induced bacterial lysis and the multiple pathophysiological consequences of bacterial meningitis, such as cerebral edema and increased intracranial pressure. Studies conducted in the last 10 years (& adjunctive dexamethasone (0.15 mg/kg every 6 hours for 4 days) in infants and children with suspected or proven H. influenzae type B meningitis; ideally this drug should be given directly before or with the first dose of an antimicrobial drug. Two studies showed that infants and children did not benefit from dexamethasone, but this may be because the drug was given too late. In a randomized trial of giving dexamethasone for 2 or 4 days, no significant differences were found in the incidence of late residual effects, suggesting that patients with meningitis caused by H. influenzae type B may benefit from shorter duration dexamethasone therapy. those with a positive cerebrospinal fluid Gram stain), but clinical data are insufficient to recommend routine use of this drug. We still recommend prescribing dexamethasone to patients classified as high risk (Herson Todd score 4.5 or higher) or patients with severely reduced mental status, cerebral edema, or very high intracranial pressure. Additional use of dexamethasone is especially important in patients with pneumococcal meningitis caused by strains highly resistant to penicillin or cephalosporin, since due to the reduced inflammatory response of the cerebrospinal fluid, the entry of vancomycin there is reduced and sterilization occurs at a later date.
Prevention
Typically, infants receive special vaccinations for preventative purposes. Because the disease has many different forms, sometimes vaccination does not guarantee complete protection against it.
The viral species spreads primarily through airborne droplets.
To avoid infection, you must try to strictly observe the rules of personal hygiene and properly handle food.
When someone in the family is sick with acute respiratory viral infections or acute respiratory infections, the baby must be isolated from the patient.
All relatives, in addition to this, must take Interferon three times a day for a week. All this reduces the risk of infection.
A course of vitamins and minerals will be useful for prevention .
You need to eat exclusively healthy food. It is also important not to get too cold.
If your child does get sick, the first thing to do is consult a doctor. It is this timely measure that will help save the life of a small patient and minimize possible consequences for his health in the future.