Most often, meningitis occurs in children; doctors say that these cases are especially common in pediatrics. This disease has certain characteristics, for example, if treatment is started in a timely manner, the disease can be quickly cured. But at the same time, the symptoms of meningitis in children are very dangerous for the health and life of the child, especially if the child is not helped in a timely manner. The disease can be classified as a fairly rare, but extremely dangerous type of disease. In this article we will talk in more detail about the symptoms of this disease, as well as how to provide full assistance to the child.
First signs
According to Dr. Komarovsky, symptoms of meningitis in children arise quite quickly, since the incubation period lasts from two days to four days, in rare cases the incubation period extends for a week.
Temperature increase
Since the disease is quite severe, it manifests itself very quickly, first the baby feels unwell, and then the condition worsens significantly to severe.
That is why parents must detect signs of this disease in time and show the patient to a doctor.
First, fairly common symptoms appear that occur with any infection, these include:
- temperature rise to 39-40 degrees;
- severe weakness;
- the child loses his appetite;
- chills occur, alternating with bouts of fever.
Due to the prevalence of symptoms, parents often mistake these signs for a common cold, flu or acute respiratory viral infection. But later, additional signs of this disease begin to develop; these symptoms are almost the same in all children.
These signs include:
- The appearance of a hemorrhagic rash, which has a red-violet tint, and the spots may also turn yellow. The rash comes in various shapes and sizes, with spots spreading throughout the patient's body.
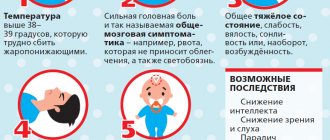
- The body temperature rises to 39-41 degrees, while the use of antipyretic medications does not give a positive result, and the temperature does not return to normal.
- The child becomes too active and excitable, or, on the contrary, lethargy and weakness occur. In one case, the baby cries a lot and sleeps poorly, in the other he sleeps a lot.
- Vomiting appears, which does not depend on food intake, and after vomiting there is no relief from the condition.
- The baby becomes more sensitive to sounds that are too loud and harsh, as well as to bright light.
- Increased sensitivity of the skin occurs, even a light touch becomes unpleasant for the patient.
If parents want to know how to recognize meningitis in children by symptoms, just consider the list of signs of this disease, which is presented above.
It is worth considering that the child’s body is individual and can react to the disease differently.
Diagnostics
Symptoms of viral meningitis in children cannot always be immediately identified, which is why doctors recommend immediately seeking help from a doctor.
Need a blood test
In the hospital, the child will be prescribed tests such as:
- A general blood test, in which you can see the number of leukocytes; if they are elevated, this will indicate the presence of infection in the body.
- Examination of the cerebrospinal fluid, as well as taking a lumbar puncture. The first analysis is collected into three tubes at once, and then immediately delivered to the laboratory. With this disease, the cerebrospinal fluid becomes cloudy and acquires a milky tint. The number of neutrophils increases to several thousand, the amount of proteins also increases, and glucose decreases significantly.
- Bacterioscopy is also carried out using cerebrospinal fluid, and swabs can also be taken from the child’s throat. In some cases, skin punctures and blood smears are required.
What are the symptoms of meningitis?
As Dr. Komarovsky says, if parents carefully monitor the health of their child, they will be able to quickly identify the presence of the first symptoms.
Headache in a child
It is enough to pay attention to the main signs, which include:
- Attacks of severe headaches in a patient, which are provoked by serious intoxication of the body. Toxins have a negative effect on the lining of the brain, causing pain as intracranial pressure increases significantly. Painful sensations can be sharp, pressing, bursting and sharp.
- The pain spreads throughout the head, so the child will not be able to indicate the location of the pain. Doctors note that these painful sensations do not subside with the use of painkillers, so if a child experiences this symptom, you should immediately call an ambulance.
- The child becomes very sensitive to bright light and loud sounds, the patient reacts negatively to light touches, as the sensitivity of the skin increases.
- Dizziness occurs and vomiting may occur. The described symptoms appear in the second and third stages of meningitis development.
Newborns may react slightly differently to the development of a dangerous disease; such babies experience additional symptoms:
- the baby becomes more whiny and nervous, or he sleeps a lot, but periodically cries out for no reason;
- there is a disturbance in the functioning of the digestive system, this manifests itself in the form of diarrhea, regurgitation and flatulence;
- in the later stages of the disease, the child experiences seizures.
It is worth noting the most dangerous symptoms of meningitis in children, these include the appearance of rashes and seizures. The fact is that the rash occurs due to the death of skin cells and tissues, which is triggered by the development of sepsis.
In this case, the disease develops rapidly and can be fatal. When the body temperature rises, spots appear on the child’s body, and convulsions occur, parents should immediately seek help from specialists.
Causes of meningitis in children
Children's meningitis can be primary (develop without previous signs of a pathological process caused by the corresponding pathogen) or secondary, when damage to the meninges is preceded by other manifestations of infection (mumps, measles, leptospirosis).
The following microorganisms can cause meningitis:
- bacteria (pneumococcus, meningococcus, Haemophilus influenzae and tuberculosis bacilli, spirochetes);
- viruses (enteroviruses of the Coxsackie-ECHO group, mumps and measles virus);
- chlamydia;
- mycoplasma;
- protozoa;
- mushrooms.
Meningitis most often affects children who belong to the following risk groups:
- premature;
- those born with intrauterine fetal hypoxia or as a result of difficult labor;
- with congenital or acquired immunodeficiency;
- who have undergone craniocerebral, spinal, vertebral trauma, neurosurgical operations and surgical interventions on the abdominal organs.
Children under 5 years of age are more likely to get meningitis. The risk of getting meningitis increases in children who attend preschool institutions and schoolchildren. Children who do not follow the rules of personal hygiene, swallow contaminated water when swimming in reservoirs, and eat food contaminated with rodent excrement are more likely to get sick. The causative agents of meningitis are transmitted by ixodid ticks.
There is a high risk of developing meningitis in children who have not been vaccinated against mumps, measles and rubella, or who have missed vaccinations with Haemophilus influenzae, meningococcus, or pneumococcal conjugate vaccines. When traveling to places dangerous for meningitis, children must be vaccinated no later than 2 weeks before the child’s departure.
The source of pathogens of childhood meningitis are sick people or bacteria carriers. Infectious agents can be transmitted by airborne droplets (with dust and saliva particles), contact (through dirty hands), waterborne, transmissible (through insect bites) and fecal-oral mechanisms. The entry points for infection are the mucous membranes of the upper respiratory tract and digestive organs. The causative agents of meningitis spread throughout the body in the following ways:
- hematogenous (through blood vessels);
- lymphogenous (lymph flow);
- geirogenic (with cerebrospinal fluid).
Meningitis in children is accompanied by the following pathological changes:
- increased production of cerebrospinal fluid;
- increased intracranial pressure and permeability of the blood-brain barrier;
- toxic damage to the brain substance;
- disorders of cerebral circulation, especially microcirculation;
- liquorodynamic disorder;
- hypoxia (insufficient oxygen supply) of the brain.
Eventually, swelling of the brain tissue develops. This is facilitated by the spread of the inflammatory process to the ventricles and brain matter, which is characteristic of purulent meningitis. With viral meningitis, cerebral edema is less pronounced, but the medulla is also involved in the pathological process. When the inflammatory process spreads to the brain, focal neurological symptoms appear.
Edema and swelling of the brain leads to its displacement with compression of the brain stem by the cerebellar tonsils. At the same time, the function of vital organs, especially breathing, is disrupted in children, which can lead to death. After suffering viral meningitis, most children do not develop complications. Children who have had bacterial meningitis may be retarded in mental development, and they sometimes develop impaired vision and hearing to the point of complete deafness.
Main signs of serous meningitis
Symptoms of serous meningitis in children can be different; this form of the disease differs in that not only inflammation of the lining of the brain occurs, but also the accumulation of purulent fluid inside the organ.
Skin sensitivity appears
The infection is provoked by an enterovirus; this disease develops quite quickly and aggressively. If a child does not receive medical care on time, then in 100% of cases there is death.
When this disease appears, parents may notice major health problems, these include:
- the appearance of hallucinations;
- increased skin sensitivity to touch;
- disturbances in the functioning of the digestive system;
- attacks of acute pain over the entire surface of the head.
There will also be other signs of this disease that are common. If parents notice the first symptoms, they should immediately call an ambulance so that specialists can provide qualified assistance to the child.
To cure this type of meningitis, the doctor may prescribe antispasmodics, as well as antipyretics, painkillers, diuretics and medications to combat viruses. In each case, the doctor separately selects therapy for the child.
Who needs to be vaccinated against meningitis, and why it is not in the National Calendar
Author:
Reznik Irina
8 minutes
26647
Meningitis annually claims the lives of dozens of Russians, and hundreds suffer from severe complications. This season was no exception: two children have died in Moscow since the beginning of the year. After the story of a woman who lost her five-year-old daughter appeared on Facebook, an active discussion began online about why there are no vaccinations against meningitis in the Russian National Calendar, and children die from what is considered a vaccine-controlled infection. Coppernews asked these questions to the experts.
Meningitis is a disease in which inflammation of the membranes of the spinal cord and brain occurs. The disease progresses very quickly and in some cases can cause severe brain damage and even death. Meningitis is divided into two main types:
- serous, caused by a viral infection entering the body
- purulent, the causative agents of which are bacteria - meningococci, pneumococci and hemophilus influenzae
In Russia, among the causative agents of purulent meningitis, the most common are meningococci types A and C - they are “responsible” for approximately 54% of purulent meningitis. Another 39% of cases of purulent meningitis are due to Haemophilus influenzae type B, and approximately 2% are due to pneumococcal infection.
Meningococcal disease is deadly and should always be treated as a medical emergency. If left untreated, 50% of cases are fatal. But even when diagnosed and treated early, up to 16% of patients die, usually within 24 to 48 hours of symptoms appearing.
Why is there no vaccination against meningitis in the National Calendar?
As explained by the head of the laboratory of vaccine prevention and immunotherapy of the Research Institute of Vaccines and Serums named after I.I. Mechnikov, Professor Mikhail Kostinov, in Russia, vaccination against meningococcal infection is included in the Vaccination Calendar for epidemic indications. That is, if it is necessary to prevent an epidemic, regions can purchase vaccines and vaccinate them en masse, especially for children. in the National Calendar when the incidence exceeds two cases per 100 thousand population. In Russia, this figure is almost an order of magnitude lower, and also significantly lower than in European countries, where such vaccination is considered mandatory.
What is considered an epidemic indication?
Such indications appear when an outbreak of meningitis is officially recorded somewhere or the incidence rate is higher than in Russia as a whole, Kostinov said. In addition, the sanitary and epidemiological situation becomes aggravated during natural disasters and major man-made accidents. So, four years ago, mass vaccination against major infections was carried out in the flooded territories of the Far East (and, by the way, after that, in the next 2-3 years, the incidence rate caused by pneumococcal infection dropped sharply here).
However, the Ministry of Health admits that the National Vaccination Calendar needs to be edited. There is hope that the changes will also affect the prevention of meningitis. Thus, at the Gaidar Forum held recently in Moscow, the Ministry of Health announced the initiative to create an independent group of experts on the development of the National Calendar of Preventive Vaccinations. The problem of the imperfection of the National Calendar was discussed during the forum discussion “Increasing the efficiency of the national immunization system.” Russian vaccine manufacturers have already expressed their desire to join the independent expert body.
Who is vaccinated without taking into account the epidemiological situation?
Such vaccination is carried out in the so-called risk groups (people with a removed spleen, with congenital immune deficiency, students, conscripts and recruits), says infectious disease specialist, MD. Andrey Devyatkin. Fortunately, we do not have an epidemic of meningococcal infection; there are isolated and group cases of the disease in some closed communities - military barracks, student dormitories. The disease affects mainly children and young people who have not yet had contact with meningococcus and acquired immune protection.
Despite the absence of an epidemiological situation, there are still a lot of cases of meningitis in all regions of the country, Kostinov believes. Therefore, in his opinion, it would be desirable to vaccinate children. Unfortunately, vaccination will have to be done at your own expense, but safety comes first.
In addition, it is recommended that people (including children over two years of age) traveling to countries where meningococcal disease is endemic get vaccinated. By the way, countries along the route of the Hajj, where the incidence rate is very high, do not issue a visa to pilgrims without a vaccination certificate.
What is the situation in Europe
According to the data cited by Mikhail Kostinov, in Europe there is much more meningococcal infection than in Russia, so all children there are vaccinated starting from the age of three months. This is explained by genetic and climatic characteristics - it’s still colder here. And, for example, in Italy, with its warm climate, vaccination against meningococcal infection, including against serotype B, which is almost never found in Russia, is carried out to all children at state expense three times, in the first and second year of life.
What serotypes are typical for our country?
According to Kostinov, one of the children who recently died in Moscow had meningococcus serotype C, the other had W-135. But in general, in Russia, the greatest epidemic danger is meningococcus serotype A. Other serotypes of meningococcus, designated by the letters of the English alphabet, as a rule, cause sporadic cases of disease, explains Devyatkin. However, in recent years, the number of severe cases of meningococcal infection caused by menigococcus serogroup W-135 (of African origin) has been increasing in the country.
As Devyatkin said, there is an endemic area in the world for meningococcal infection, the so-called meningitis belt of Africa (sub-Saharan Africa, stretching from Senegal in the west to Ethiopia and Egypt in the east). A high incidence of menigococcal infection is observed in Canada, with outbreaks occurring in France and the USA. Students of closed educational institutions and colleges are especially vulnerable. For us, the strain of menenigococcus serogroup W-135 is still new, and it is not yet clear whether cross-protection will work with it when using domestic polysaccharide vaccines (groups A and C), Devyatkin notes.
What meningococcal vaccines are available in Russia?
The most budget option is the meningococcal polysaccharide vaccine, which is used to develop immunity to serotypes A and C. But the imported Menactra vaccine has several advantages over it. Firstly, it contains polysaccharides of four serogroups - A, C, W and Y. And, secondly, it can be used in children from 8 months, Kostinov said. This is the so-called new generation conjugate vaccine ( representing complexes of bacterial polysaccharides and toxins ), which, unlike polysaccharide vaccines, is “seen” by the immune system of a child in the first year of life. The imported polysaccharide tetravalent vaccine “MentsevaxACWY” is an old generation vaccine and, like the Russian one, is used only from two years of age. There is no point in doing this before - the child simply will not develop immunity.
A separate issue is vaccination against meningococcus serotype B. Currently, no vaccine against this type of infection is registered in Russia, and some patients who want to be vaccinated go abroad, where they receive a drug called Bexsero. But the role of the vaccine against meningococcus B should not be exaggerated: according to Professor Kostinov, in our country it is very rare, and doctors practically do not know it.
For the same reason, foreign companies are in no hurry to promote such vaccines on the Russian market - after all, the drugs must be in demand. As explained by GlaxoSmithKline, the manufacturing company of Bexsero, indeed, this vaccine is not currently registered in Russia. “ We have not yet submitted it for registration in Russia. But we are considering this possibility ,” said a company representative. Producing vaccines is difficult and expensive, but for those GSK drugs that are in demand in Russia, the company, as a rule, fills the need.
Due to the fact that mass free vaccination against meningitis is currently not carried out in Russia, doctors recommend taking care of the vaccination yourself. At a minimum, the list of recommendations includes the drug Menactra. Here, for example, is the recommendation of Fedor Katasonov, a pediatrician at the GMS Clinic Center for Congenital Pathology:
“To prevent meningococcus from killing, we vaccinate our patients. About 98% of my patients receive Menactra , a vaccine that protects well against about half of meningococci and moderately protects against the other half. Some of them who travel to Europe, on my recommendation, take Bexsero there - a vaccine that reliably protects against the second half (and a little more - against gonorrhea). These vaccines are not and will not be included in our sinful calendar, they must be done at your own expense, but forgive me . Free healthcare is generally a harmful myth.”
In addition, infectious disease experts believe that patients should have access to all up-to-date vaccines, even if health officials do not consider some of them necessary for the population. Here is how Vasily Shakhgildyan, candidate of medical sciences, infectious disease doctor at the H-Clinic, commented on this question:
“I believe that the issue of registration and availability of European and North American medicines in Russia needs to be simplified. And, accordingly, make it possible to purchase them on the territory of the Russian Federation. This applies to both the Menactra vaccine and the Bexsero vaccine. Those wishing to be vaccinated against meningococcal infection with the new generation vaccine and the vaccine against meningococcal serotype B should have this opportunity. Yes, the issue of including vaccination against meningococcal infection in the official vaccination calendar (and, accordingly, doing it at public expense) requires discussion. But, I repeat, Russian citizens should have the opportunity to purchase this or that vaccine at their own expense and vaccinate their child, protecting him from meningococcal infection.”
How effective are vaccines?
As Devyatkin explained, vaccines against meningococcal infection do not guarantee long-term protection. The fact is that the effectiveness of vaccines is related to the type of pathogen. Vaccines against viral infections are most effective, especially when live viruses are used (for example, measles, rubella, oral polio vaccine). As for meningococcus, it is not a virus, but a microbe (the bacterium Neisseria meningitides), and vaccination against it is aimed at developing immunity to a specific strain of the pathogen serotype that causes a severe pathological process.
The polysaccharide of the protective capsule of the pathogen, specific for each serotype, is used as an antigen to create meningococcal vaccines. Such immunity is not permanent; at best, it will last 3-5 years. Almost all bacterial vaccines used are guaranteed to protect only for the next one-year period, and then immunity decreases. The main problem of specific (vaccinal) prevention of meningococcal infection is that it can be caused by 12 serotypes of the pathogen, and there is no universal vaccine against them yet.
How likely is it to get meningitis?
Fortunately, meningococcal infection is not a highly contagious infectious disease that is easily transmitted from person to person through fleeting contact, such as measles or chickenpox, notes Devyatkin. Meningococcal infection occurs only in humans; the pathogen is not stable in the external environment. The source of infection is a bacteria carrier or a patient with meningococcal nasopharyngitis, the mechanism of infection transmission is airborne. Therefore, for infection you need, firstly, quite long and close contact, close communication in a confined space with someone who is easily ill or a carrier of the microbe.
And secondly, for the development of the disease - a susceptible, non-immune person who has not encountered meningococcus before. Therefore, the expert believes, one should not be afraid of seasonal respiratory infections. Repeated acute respiratory infections are an opportunity to create lasting immunity, including natural anti-epidemic control against meningococcus. If a person gets sick with meningococcal nasopharyngitis, he will develop specific immunity against meningococcus. Thus, having become infected with meningococcus again, he will no longer become severely ill, and perhaps not at all.
However, one should not take every case of acute respiratory infections lightly, because respiratory symptoms can be the debut of a severe meningococcal infection, Devyatkin emphasizes. Therefore, each sick person must be isolated and immediately shown to a doctor. The main thing in the fight against meningococcal infection is the timely identification and isolation of all patients and carriers of the pathogen, immediate treatment of all patients.
Main signs of viral meningitis
The incubation period for viral meningitis in children does not last long, so symptoms appear fairly quickly.
Chills appear
The main features include:
- increased body temperature;
- bouts of severe vomiting;
- the appearance of chills;
- signs of ARVI development;
- the appearance of a rash on the baby’s skin;
- severe muscle tension;
- general weakness and drowsiness.
In this case, antiviral medications are used for treatment, and therapy is also used that helps eliminate intoxication of the body.
If the body temperature is very high, the doctor has the right to prescribe the use of medications to reduce the temperature.
Treatment
To carry out full treatment, the child must be taken to the hospital, where he is examined by a doctor.
Treatment is carried out by a doctor
To help the patient, the doctor may use:
- Antibacterial therapy. It is commonly used to treat bacterial meningitis. Only a doctor can select the appropriate drug, having previously established the type of pathogen. The doctor prescribes streptomycin punctures, which are injected into the spinal canal; this therapy is performed for tuberculosis. In case of viral meningitis, the doctor must monitor the patient and also prescribe symptomatic treatment to alleviate the child’s condition.
- The doctor uses methods that help normalize intracranial pressure. The fact is that in any form of this disease, the amount of cerebrospinal fluid increases, for this reason severe headaches occur. To reduce pressure, a puncture of the cerebrospinal fluid is taken, this helps to reduce the amount of fluid, which will reduce the pressure. Additionally, the use of diuretic medications is recommended.
- It is important to carry out symptomatic treatment; it includes the use of antipyretics, vitamin complexes, as well as antiemetic medications and painkillers.
- The doctor uses special therapy, which is aimed at reducing intoxication of the body, and also uses saline solutions to restore water and salt balance in the body.
- If there is such a need, the patient is prescribed medications that reduce the number of seizures or eliminate these seizures.
- Hormonal agents can be used against inflammation; they are used only after a doctor’s prescription.
Meningitis
Among the many human diseases, meningitis is one of the most dangerous. You can suffer from pneumonia on your feet, you can walk with tuberculosis for years, you can, with the help of “healers,” try to recover from sexually transmitted diseases for a long time. With meningitis , such “numbers” do not go through - either to the hospital, or... Meningitis is a well-known disease. At least the average person, without any special medical education, knows the word “ meningitis ” and, although the features of the disease itself are not very clear, meningitis . An emergency doctor may say: “You have a sore throat (flu, pneumonia, enterocolitis, sinusitis, etc.). Get ready to the hospital quickly." In response, he will definitely hear: “Doctor, is there no way to get treatment at home?” But if the word “meningitis” is uttered, even if not categorically: “You have meningitis!”, but with doubt: “It looks like meningitis,” you can say with confidence: a normal person will not even mention any treatment at home. This attitude towards meningitis is generally understandable - less than 50 years have passed since the time when it became possible to treat it (meningitis). But if the mortality rate from most childhood diseases decreased during this time by 10-20 times or more, then for meningitis - only 2 times. So what kind of disease is this, meningitis? First of all, it should be noted that meningitis is an infectious disease. That is, the direct cause of the disease is certain microbes. Most human infections allow us to establish a clear relationship between the name of the disease and the name of its specific pathogen. Syphilis - pale spirochete, scarlet fever - streptococcus, salmonellosis - salmonella, tuberculosis - Koch's bacillus, AIDS - immunodeficiency virus, etc. At the same time, there is no specific connection between “meningitis and the causative agent of meningitis”. The word “meningitis” itself means inflammation of the membranes of the brain , and the cause of this inflammation can be a huge number of microorganisms - bacteria, viruses, fungi. Infectious disease experts say, not without confidence, that under certain conditions any microorganism can cause meningitis in a person of any age. From this it is clear that meningitis can be different - different in the speed of development, in the severity of the condition, in the frequency of occurrence, and, most importantly, in the methods of treatment. All meningitis has one thing in common - a real threat to life and a high probability of complications. For meningitis to occur, a specific pathogen must enter the cranial cavity and cause inflammation of the membranes of the brain. Sometimes this happens when foci of infection occur in the immediate vicinity of the membranes of the brain - with purulent otitis media, for example, or with sinusitis. Often the cause of meningitis is traumatic brain injury. But most often, microbes enter the cranial cavity through the bloodstream. It is obvious that the very fact of a microbe entering the blood, the very possibility of its “introduction” and subsequent reproduction on the meninges is determined by the state of immunity. It should be noted that there are a number of, usually congenital defects of the immune system, that predispose to the occurrence of meningitis. It is not surprising that in some families all children suffer from meningitis - although this disease is not so common, in comparison, for example, with sore throat, whooping cough, chickenpox or rubella. But if the role of immunity is generally clear, then so far it has not been possible to find a convincing explanation for the fact that boys suffer from meningitis 2-4 times more often than girls. Depending on the type of pathogen, meningitis can be viral, bacterial, or fungal. Some protozoa (such as amoeba and toxoplasma) can also cause meningitis. The development of viral meningitis can accompany the course of well-known infections - chickenpox, measles, rubella, mumps, damage to the meninges occurs with influenza, and with infections caused by herpes viruses. In weakened patients, in the elderly, and in infants, meningitis caused by fungi occurs (it is clear that in these situations it is the lack of immunity that plays the leading role in the occurrence of the disease). Bacterial meningitis is of particular importance . Any purulent focus in the body - pneumonia, an infected burn, tonsillitis, various abscesses, etc. - can cause meningitis, provided that the pathogen enters the blood and reaches the meninges with the blood flow. It is clear that the well-known causative agents of purulent processes (staphylococci, streptococci, Pseudomonas aeruginosa, etc.) will be the causative agent of meningitis in this case. One of the most terrible is tuberculous meningitis - almost forgotten, it is now becoming more and more common. At the same time, there is a microorganism that causes meningitis most often (60-70% of all bacterial meningitis). It is not surprising that it is called meningococcus . Infection occurs by airborne droplets, meningococcus settles on the mucous membranes of the nasopharynx and can cause a condition very similar to a common respiratory viral infection - a slight runny nose, redness of the throat - meningococcal nasopharyngitis . It was not for nothing that I used the phrase “can cause” - the fact is that the entry of meningococcus into the body quite rarely leads to the onset of disease - the leading role here belongs to very special individual changes in immunity. In this regard, two facts are easily explained: the first is the risk of developing meningitis during contact, for example, in children's institutions is 1/1000 and the second is the frequent detection of meningococcus in the nasopharynx in completely healthy individuals (from 2 to 5% of children are healthy carriers) . The body's inability to localize the microbe in the nasopharynx is accompanied by the penetration of meningococcus through the mucous membrane into the blood. With the bloodstream, it enters the meninges, eyes, ears, joints, lungs, adrenal glands, and in each of these organs a very dangerous inflammatory process can occur. Obviously, damage to the meninges is accompanied by the development of meningococcal meningitis . Sometimes meningococcus enters the blood quickly and in huge quantities. Meningococcal sepsis , or meningococcemia, occurs - perhaps the most terrible of all childhood infectious diseases. The microbe secretes poisons (toxins), under their influence multiple blockages of small vessels occur, blood clotting is impaired, and multiple hemorrhages appear on the body. Sometimes, within a few hours after the onset of the disease, hemorrhage occurs in the adrenal glands, blood pressure drops sharply and the person dies. There is an amazingly dramatic pattern in the occurrence of meningococcemia , which is as follows. The fact is that when a microbe penetrates the blood, it begins to react with certain antibodies that try to destroy meningococcus. It has been proven that there is cross-activity of a number of antibodies - that is, if there are large quantities of antibodies, for example, to streptococcus, pneumococcus, staphylococcus - then these antibodies can have an inhibitory effect on meningococcus. So it turns out that children who are sick, have chronic foci of infections, have had pneumonia and many other illnesses, almost never get meningococcemia. The scary thing about meningococcemia is that within 10-12 hours an absolutely healthy child who has never been sick before can die! All the above information is not intended to intimidate readers. Meningitis is treatable. But the results (duration and severity of the disease, the likelihood of complications) are closely related to the time that will be lost before the start of adequate therapy. Obviously, the above-mentioned “timing of initiation of adequate therapy” depends on when human subjects seek medical attention. Hence the urgent need for specific knowledge, so that later there will be no excruciating pain... The essence of specific knowledge regarding meningitis is that the appearance of certain signs indicating the possibility of this disease requires immediate seeking medical help. Inflammation of the meninges is characterized by a number of symptoms, but many of them are not specific - that is, their (symptoms) may also occur in other diseases that are much less dangerous. Most often this is what happens, but the slightest suspicion of the development of meningitis does not allow you to take risks and requires immediate hospitalization and careful medical supervision. Let us now consider the most typical situations, each of which does not allow us to exclude the development of meningitis.
- If, against the background of any infectious disease - acute respiratory infections, chickenpox, measles, mumps, rubella, "fever" on the lips, etc. - perhaps not at the beginning of the disease (even more often not at the beginning), an intense headache appears, so strong, that it worries more than all other symptoms if the headache is accompanied by nausea and vomiting.
- In all cases, when, against the background of increased body temperature, there is pain in the back and neck, aggravated by moving the head.
- Drowsiness, confusion, nausea, vomiting.
- Convulsions of any intensity and any duration.
- In children of the first year of life - fever + monotonous crying + bulging fontanelle.
- Any (!!!) rash against a background of elevated temperature.
In addition to the symptoms described above, some reflexes change in a very definite way, and only a doctor can detect this. It is important to remember and understand that such frequent symptoms as vomiting, nausea and headache necessarily require a medical examination - God protects the best. Any rash accompanied by an elevated temperature may be meningococcemia . You (or your smart neighbors) may be confident that it is rubella, measles or “diathesis”. But the doctor must see the rash, and the sooner the better. If elements of the rash look like hemorrhages, if new rashes appear quickly, if this is accompanied by vomiting and high fever, every chance should be taken to ensure that the patient immediately ends up in the hospital, preferably immediately in the infectious diseases department. Remember: with meningococcemia , the count is not in hours, but in minutes. It should be noted that even a doctor of the highest qualifications can diagnose meningitis with absolute certainty only in one case - when the symptoms of irritation of the meninges are combined with the typical rash described above. In all other cases, the diagnosis can only be suspected with varying degrees of probability. The only way to confirm or exclude meningitis is a spinal (lumbar) puncture. The fact is that a special cerebrospinal fluid circulates in the brain and spinal cord - cerebrospinal fluid. With any inflammation of the brain and (or) its membranes, inflammatory cells accumulate in the cerebrospinal fluid; the appearance of the cerebrospinal fluid (normally colorless and transparent) often changes - it becomes cloudy. A study of cerebrospinal fluid allows not only to establish a diagnosis of meningitis , but also to answer the question of what kind of meningitis it is - bacterial (purulent) or viral, which is crucial in choosing a treatment option. Unfortunately, at a purely philistine level, there is a very widespread opinion about the enormous dangers that a spinal puncture poses. In fact, these fears are absolutely unfounded - the puncture of the spinal canal is carried out between the lumbar vertebrae at the level where no nerve trunks extend from the spinal cord, so there are no mythical paralysis after this manipulation. From a legal point of view, the doctor is obliged to perform a spinal tap if there is a real suspicion of meningitis . It should be noted that puncture has not only diagnostic, but also therapeutic usefulness. With any meningitis , as a rule, there is an increase in intracranial pressure, the consequence of which is a severe headache. Taking a small amount of cerebrospinal fluid can reduce blood pressure and significantly alleviate the patient’s condition. During a puncture, antibiotics are often administered into the spinal canal. For example, with tuberculous meningitis, the only chance to save the patient is frequent (often daily) punctures, during which a special version of streptomycin is injected into the spinal canal . Taking into account the above information, it becomes clear that the treatment of meningitis depends on the type of pathogen. The main thing in the treatment of bacterial meningitis is the use of antibiotics. The choice of specific drug depends on the sensitivity of the particular bacterium and whether the antibiotic is able to penetrate the cerebrospinal fluid . With timely use of antibacterial drugs, the chances of success are very high. With viral meningitis, the situation is fundamentally different - there are practically no antiviral drugs, the exception is acyclovir, but it is used only for herpes infection (let me remind you that chicken pox is one of the variants of herpes). Fortunately, viral meningitis has a more favorable course compared to bacterial meningitis. But helping a patient is not limited to just influencing the pathogen. The doctor has the opportunity to normalize intracranial pressure, eliminate toxicosis, improve the functioning of nerve cells and blood vessels in the brain, and use powerful anti-inflammatory drugs. Timely treatment of meningitis within two to three days leads to a significant improvement in the condition, and in the future almost always to a complete cure without any consequences. I emphasize once again: timely treatment started...
author Komarovsky E.O. published 17/01/2007 14:22 updated 07/01/2016 - Diseases and treatment