Related news
Clinical recommendations for vaccination of pregnant women against influenza and pneumococcal infection
How to stop pneumococcus? Interview with N. I. Briko
How to prevent pneumococcal infections in adults?
Prevention of pneumococcal infection
Experts advocate for stronger protection against pneumococcus
Alexander Chuchalin: “Vaccine prevention is the optimal strategy to combat pneumonia”
Vaccination of adults against pneumococcal infection: world experience
Additional materials
Seminar: “Pneumococcal infection: status, problems and opportunities for prevention”
Where have all the ear infections gone?
Humanity against pneumococcus - a story of struggle and victories
General information
Worldwide, diseases caused by Streptococcus pneumoniae (S. Pneumoniae or pneumococci) and related to pneumotropic infections represent one of the most serious public health problems.
There are invasive and non-invasive forms of pneumococcal diseases. Invasive pneumococcal infection (IPI) includes a number of severe and life-threatening diseases: bacteremia without a visible focus of infection, meningitis, pneumonia, sepsis, pericarditis, arthritis. Non-invasive forms of pneumococcal infection are bronchitis, community-acquired pneumonia, otitis media, sinusitis, conjunctivitis.
According to statistics, up to 70% of all pneumonias, about 25% of otitis media, 5-15% of purulent meningitis, about 3% of endocarditis are caused by pneumococcus S. Pneumoniae.
Pneumococcal infection is usually a complication of other infections. Examples are pneumococcal pneumonia, inflammation of the middle ear (otitis) in children after or against the background of influenza, or measles, or any other respiratory viral infection.
Pneumococcal disease is spread through respiratory droplets such as coughing (especially through close contact). The source of infection can be a person without any clinical manifestations. Information about seasonality for diseases caused by S. Pneumoniae is quite contradictory. However, a number of authors note an increase in incidence in the autumn-winter period, which is characteristic of a number of other pneumotropic infections.
Children of the first years of life are the main carriers of pneumococci, infecting adults. While the usual carrier frequency in adults is 5–7%, among adults living with children it reaches 30%.
Chance of getting sick
The highest incidence of severe pneumococcal infections is recorded in children under 5 years of age and among older people (over 65 years of age). Young children under 2 years of age, whose bodies are unable to resist infection, are especially defenseless against pneumococcus. For this age group, this is the No. 1 infection and the most common cause of severe forms of pneumonia, otitis media, and meningitis. Among the elderly, the most vulnerable are those who are permanently residing in aged care facilities.
In addition, risk groups for the incidence of pneumococcal infection include children and adults with chronic diseases of the cardiovascular, respiratory systems, diabetes mellitus, liver cirrhosis, chronic renal failure, Hodgkin's disease; children and adults with oncohematological diseases; HIV-infected; children and adults with cerebrospinal fluid leakage; children and adults after cochlear implantation; children and adults with sickle cell disease; with anatomical asplenia, or planning or having already undergone removal of the spleen. This should also include the so-called “organized” contingents (children attending kindergartens, students living in dormitories, military personnel, residents of nursing homes, prisoners and other adults and children living in overcrowded conditions). The presence of bad habits (alcohol, smoking) is also a risk factor.
Diagnostic methods
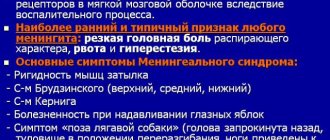
The presence of meningeal disorder is determined by an initial examination by a neurologist. Obvious signs specific to this pathology form the clinical picture. When studying the patient's medical history, a previous pneumococcal infection is revealed. The nature of the pathogenic agent can only be determined by laboratory analysis of the cerebrospinal substance. To do this, it is necessary to perform a lumbar puncture. During the procedure, not only the liquid is taken, but also the intensity of its pressure upon expiration is analyzed. A pathological intracerebral process increases the pressure in the cerebrospinal fluid.
Primary visual changes are also assessed; the internal cerebral fluid becomes cloudy with a predominance of whitish or green tones. This occurs due to the increased production of protein compounds, chlorides, blood elements, and sugar. Microscopic examination reveals pathogens - pneumococci. To recognize the nature of the pathogen, a blood and sputum test is taken from the lungs. In internal sepsis, coccal agents are common in these substances.
The following hardware methods are used to determine the state of the brain:
- computer scanning;
- Magnetic resonance imaging.
In the images of tomographic installations, foci of the spread of infection, the extent of inflammation, the volume of swelling, and the degree of displacement of brain structures are clearly visible. Diagnostics are carried out using powerful devices, so it is important to choose a clinic with modern equipment in advance. For an emergency search for a diagnostic center, the website pages provide a complete list of city clinics located in each district. You can quickly sign up for diagnostics and find out about the possibility of emergency tomography by calling the hotline located at the top of the page. The operators of the consultation center will provide full information about the procedure, guide you to the nearest institutions, make an appointment for free time, or recommend a medical organization with emergency appointments for patients.
Treatment of pathology
Therapeutic manipulations started on time lead to a significant improvement in a person’s condition by the end of the first week. Then the specific symptoms subside. Renewal of the disease, which is characteristic of pneumococcal meningitis, may occur. Recovery will be difficult and protracted. Only by the end of the first month does complete sanitation of the intracerebral fluid occur.
The disease is treated exclusively in a hospital setting. Complete rest and bed rest are prescribed. It is necessary to exclude any noise or light exposure. Food should be high in calories, but without irritating chemical effects. Hard, sour, spicy foods are prohibited.
Injection treatment with glucose is carried out synchronously with antibiotic therapy. Drinking plenty of fluids is prescribed in conjunction with taking diuretics. This will avoid long-term persistence of edema. Therapy is carried out aimed at improving cerebral circulation. Nootropics and neurometabolites are used to restore the functionality of nerve cells. Drug treatment lasts up to six months, then varies depending on the patient’s condition.
Forecast of the course and preventive measures
The positive prognosis status is determined by the speed of response measures, the speed of identifying pneumococcus as a pathogen, and timely initiation of antibacterial therapy. Despite the quality of the recovery, a large percentage of critical changes remain in brain activity after suffering pathology. At a young age, slight mental retardation, disturbances in sound perception, hearing loss, systematic epileptic seizures, etc. may be observed.
Mortality from the disease is associated with a rapid increase in edema, complications in the functionality of the heart and respiratory system, and general blood poisoning. To prevent the risk of disease, preliminary vaccination is carried out. All children are recommended to receive the vaccine before the age of two. If a risk group is identified, vaccination continues for up to five years. Next, revaccination is carried out in adulthood, after the 65-year threshold, when the immune response tends to decline.
Symptoms
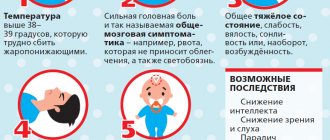
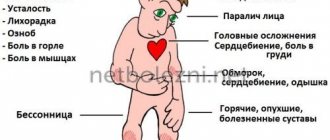
Symptoms of pneumococcal infection, which causes pneumonia, include fever, cough, shortness of breath and chest pain. Symptoms of pneumococcal purulent meningitis are a stiff neck, severe headache, fever, confusion and disorientation, and photophobia. The initial manifestations of pneumococcal bacteremia (blood poisoning, the most severe form with a mortality rate of up to 50%) may be similar to some symptoms of pneumonia and meningitis, and may also include joint pain and chills.
In this regard, doctors again and again warn about the dangers of self-medication! You should not try to cope with the disease on your own, using commercials for various drugs and their availability in pharmacy chains as a methodological guide.
Complications after an illness
Pneumococcal meningitis is particularly severe, the incidence of which is about 8 per 100 thousand children under 5 years of age. On average, about 83% of cases occur in children under 2 years of age. Despite the fact that the pneumococcus Streptococcus pneumoniae ranks third after Haemophilus influenzae type b (hemophilus influenzae type b) and Neisseria meningitidis (meningococcal infection) as an infectious agent responsible for the development of this disease, the prognosis for pneumococcal meningitis is much more serious. Complications in the form of mental retardation, impaired motor activity, epilepsy and deafness occur significantly more often than in the outcome of bacterial meningitis of other etiologies.
Pneumonia caused by pneumococcus S. pneumoniae is most often complicated by pulmonary empyema (accumulation of pus in the pleural cavity, causing a decrease in the respiratory surface of the lung tissue), which leads to death (up to 2/3 of cases for empyema). In Russia, out of 500 thousand cases of pneumonia per year, 76% have pneumococcal etiology in adults and up to 90% in children under 5 years of age. The frequency of pneumococcal pneumonia among children under 15 years of age is 490 cases per 100 thousand, in children under 4 years of age - 1060 cases per 100 thousand.
Pneumococcal bacteremia in most cases (up to 80%) occurs with symptoms of fever without a focus of infection. The incidence of bacteremia caused specifically by S. pneumoniae is 8-22% in young children. It is pneumococcal sepsis with the development of severe shock damage to organs that is the most severe and life-threatening form of pneumococcal infection. The frequency of this nosological form in children under 5 years of age averages 9,000 cases per year; the mortality rate reaches 20-50%.
According to world statistics, the proportion of pneumococcal otitis media ranges from 28 to 55% of all registered cases. Pneumococcal acute otitis media is characterized by a more severe course and a high risk of otogenic complications, including a tendency to perforation of the tympanic membrane. Pneumococcal otitis media is the most common cause of hearing loss in children.
Risk of developing pneumococcal infections:
- In healthy people, the risk is 8.8 per 100,000.
- In patients with diabetes mellitus – 51.4.
- In adults with chronic lung diseases – 62.9.
- In patients with chronic heart disease – 93.7.
- for those suffering from cancer – 300.4.
- For HIV-infected people – 422.9.
- In patients with oncohematological diseases - 503.1 per 100,000.
Vaccination of persons classified as risk groups
Immunization against PI is carried out throughout the year. If you plan to organize a mass vaccination program against influenza, then it is convenient to carry out this vaccination simultaneously with immunization against PI before the start of the season of acute respiratory diseases and influenza, which corresponds to WHO recommendations.
Immunization against PI is necessary for people of any age at risk of developing iPI. Patients with impaired immunological reactivity or due to the use of immunosuppressive therapy, genetic defects, HIV infection or other reasons may experience a reduced humoral immune response to vaccination.
- In immunocompromised patients of any age, a single vaccination with PPV-13 is initially recommended, and then (no earlier than 8 weeks later) with PPV-23; after 5 years, repeated administration of PPV-23 is necessary.
Contraindications to vaccination
The main contraindications for vaccination against PI are the following:
- pronounced, severe systemic reactions to the previous administration of the vaccine (anaphylactic reactions);
- hypersensitivity to any component of the vaccine;
- acute infectious diseases or exacerbation of a chronic process (the underlying disease).
Vaccination can be carried out after 1–2 weeks. after achieving remission or recovery from an acute infectious disease. Previous PI is not a contraindication to immunization.
Post-vaccination reactions
Overall, the incidence of serious adverse events reported within 1 month. after vaccine administration was <2%. No significant differences were observed with both vaccines.
Most often (about 20% of cases of all adverse events) in the post-vaccination period of PCV administration the following reactions occur: fever, rarely exceeding 39 ° C, excitability, loss of appetite and sleep disturbance, as well as local reactions in the form of swelling, hyperemia, soreness, thickening of the site of vaccine administration. A significant proportion of these reactions develop in the first 48 hours after vaccination and stop on their own or with the use of antipyretic and antihistamine drugs.
When performing PPV vaccination, it is possible to develop post-vaccination reactions of varying severity during the first 3 days, among which local reactions in the form of pain, redness, thickening or swelling at the injection site are most often observed. Severe local reactions such as the Arthus phenomenon are very rarely described in people who have previously had PI and, as a result, have a high level of specific antibodies. A moderate increase in body temperature can persist from several hours to 3 days after vaccination. In very rare cases, other general reactions may develop - adenopathy, arthralgia, rash and allergic reactions (urticaria, Quincke's edema, anaphylactic reaction).
After administration of the vaccine, as with all injectable vaccines, you should always be prepared to provide appropriate medical care and monitoring in the event of an anaphylactic reaction.
Features of vaccination of people with chronic diseases
- Vaccinations are carried out under the supervision of a doctor at the immunoprophylaxis office. After vaccination, the patient should be observed for ≥ 30 minutes.
- Vaccination is carried out against the background of anti-relapse (basic) therapy in consultation with a specialist. Vaccinations are carried out every 2–4 weeks. after stabilization of the process or the beginning of remission when stable clinical symptoms and target hemodynamic parameters are achieved. Exceptions are complicated myocardial infarction or its relapse (after 28 days), chronic heart failure (7 days after the end of titration of diuretics with a stable patient’s body weight), dilated cardiomyopathy (after control of hemodynamics for 4 weeks and in a stable condition without syndrome hemodynamic decompensation).
- When vaccinating children and adults with damage to the nervous system, especially with a history of febrile convulsions, it is recommended to measure the temperature after vaccination 3-4 times a day for the first 3 days; antipyretics are prescribed according to indications.
- In patients with diabetes, vaccination against PI is carried out in the absence of complaints of thirst, polyuria, loss of appetite, fasting sugar level ≤ 10–12 mmol/l, daily glucosuria
≤ 10–20 mg, absence of ketone bodies in urine. The vaccine is administered deeply intramuscularly into areas free from lipodystrophy. When vaccinated, no dose adjustment of glucose-lowering drugs or insulin is required.
- For kidney diseases, vaccination is carried out during the period of clinical and laboratory remission in patients whose estimated glomerular filtration rate (eGFR) is 30–59 ml/min/1.73 m2 (eGFR category C3) and <30 ml/min/1.73 m2 (eGFR categories C4–C5). Patients receiving replacement therapy with hemodialysis or peritoneal dialysis are vaccinated on a day free from these procedures.
- When planning the administration of immunosuppressive drugs, vaccination should be carried out 4-6 weeks in advance. before the start of immunosuppressive therapy or after 3–6 months. at the end of radiation or chemotherapy.
- In patients with HIV infection, vaccination is carried out during the period of remission of chronic diseases (after 2–4 weeks) with a CD4 T-lymphocyte count ≥ 200 cells/mm3.
Features of vaccination of persons with allergic diseases
- Vaccination is carried out under the supervision of a doctor at the immunoprophylaxis office. After vaccination, the patient should be observed for ≥ 30 minutes.
- Strict adherence to a diet with the exclusion of products to which allergic reactions have previously been noted, “obligate” allergens (chocolate, honey, nuts, fish, citrus fruits, strawberries, products with dyes and preservatives), as well as strict maintenance of a hypoallergenic lifestyle for 1 week. before vaccination and within 2 weeks. after her.
- Vaccination is performed after 2–6 weeks. (depending on the pathology) after achieving stabilization of the process, control of the disease or the onset of remission. Basic therapy for an allergic disease, agreed upon with an allergist, is carried out, against the background of which control over the disease is achieved.
- Antihistamines are prescribed for 1–2 weeks. before vaccination (depending on the nosological form) and 4–5 days after it.
- Skin testing with allergens can be completed within 1–1.5 weeks. before and after 1 month. after vaccination.
- A course of allergen-specific immunotherapy can begin after 2 weeks. after vaccination.
Treatment
A global problem in the world is the increasing resistance of pneumococci to antibiotics - this means that treatment of pneumococcal infections with antibiotics is often ineffective. The main factor in the development of antibiotic resistance in pneumococcus is the irrational use of antibacterial drugs. When conducting monitoring in 2004-2005. 11% of pneumococcal strains were resistant to penicillins, 7% to macrolides, 40.8% to co-trimoxazole. But already in 2011-2012. a similar study showed that already 29% of S. pneumoniae strains have reduced sensitivity or are resistant to penicillin, 26% of strains are resistant to macrolides, 50% of strains are resistant to co-trimoxazole. According to the latest data, up to 10% of strains of pneumococcal infection have acquired resistance to combinations of broad-spectrum penicillin with β-lactamase inhibitors, which is extremely unfavorable prognostically, since due to the rapid development of the disease (2-3 days) there is no time to determine sensitivity to antibiotics , as a rule, no, and patients with severe pneumococcal infection often die, despite the introduction of standard antibacterial drugs.
Effectiveness of vaccination
According to WHO, world experience has shown that mass vaccination reduces the incidence of pneumococcal meningitis and severe pneumonia in children by more than 80%, and the incidence of all pneumonia and otitis media by more than a third. The carriage of pneumococci in children is decreasing, and accordingly, unvaccinated children and adults get sick less. The World Health Organization projects that global use of pneumococcal vaccination will prevent 5.4 to 7.7 million child deaths by 2030.
Vaccination is the only highly effective way to significantly influence the morbidity and mortality of pneumococcal infections and reduce the level of antibiotic resistance in S. pneumoniae. With evidence of the safety and effectiveness of pneumococcal conjugate vaccines, WHO and UNICEF believe it is necessary to include these vaccines for children in all national immunization programs. At the same time, it should be noted that the maximum protective effect is achieved with routine vaccination of all children under 2 years of age, and not just patients in risk groups.
brief information
Diseases of pneumococcal etiology are an urgent problem in practical healthcare, which is due to the leading role of Streptococcus pneumoniae in the structure of respiratory tract infections.
According to experts from the World Health Organization (WHO), these are the most common bacterial infections in adults in the world. S. pneumoniae continues to be a leading cause of serious illness, including bacteremia, meningitis, and pneumonia. Representing a serious medical and social problem for many countries, pneumococcal infections (PI) are also relevant for Russia. At the same time, the problem of PI in our country is given clearly insufficient attention, despite the existing achievements in this area, the main one of which is the creation of effective methods for the prevention of these infections, aimed at reducing the costs of treating diseases caused by pneumococcus and mortality due to this reason. The effectiveness of vaccination against PI, proven in numerous studies, made it possible to consider this event as promising and recommended for inclusion in the Calendar of Preventive Vaccinations.
Vaccines
Vaccination has been used to combat pneumococcal infection for more than 30 years. Since 1981, the pneumococcal polysaccharide vaccine has been used. Since 2000, pneumococcal conjugate vaccines have been used in international practice for immunoprophylaxis of pneumococcal infection in young children.
To date, the following vaccines have been registered in Russia: two pneumococcal conjugate vaccines (10-valent and 13-valent - PCV10 and PCV 13) and one - polysaccharide 23-valent (PPV23). The latter is used in children over 2 years of age and adults. While conjugate vaccines are recommended for immunization of children from 2 months of age and adults aged 50 years and older. PCV13 is also registered in the US and EU for use in broader age groups (children 6 weeks to 17 years and adults 18 years and older). In the near future, the age indications for PCV13 are also expected to expand in Russia.
In 2013, the pneumococcal 13-valent conjugate vaccine Prevenar13 was awarded the Galen Prize as the best biotechnological product of the year.
More about vaccines
Pneumococcal infection
Pneumococcal infection
Worldwide, diseases caused by pneumococci and related to pneumotropic infections represent one of the most serious public health problems.
According to statistics, up to 70% of all pneumonias, about 25% of otitis media, 5-15% of purulent meningitis, about 3% of endocarditis are caused by pneumococcus.
Pneumococcal infection is usually a complication of other infections. Examples are pneumococcal pneumonia, inflammation of the middle ear (otitis) in children after or against the background of influenza, or measles, or any other respiratory viral infection.
Pneumococcal disease is spread through respiratory droplets such as coughing (especially through close contact). The source of infection can be a person without any clinical manifestations. Children of the first years of life are the main carriers of pneumococci, infecting adults. While the usual carrier frequency in adults is 5–7%, among adults living with children it reaches 30%.
PROBABILITY OF GETTING ILL
The highest incidence of severe pneumococcal infections is recorded in children under 5 years of age and among older people (over 65 years of age). Young children under 2 years of age, whose bodies are unable to resist infection, are especially defenseless against pneumococcus. For this age group, this is the No. 1 infection and the most common cause of severe forms of pneumonia, otitis media, and meningitis. Among the elderly, the most vulnerable are those who are permanently residing in aged care facilities.
In addition, risk groups for the incidence of pneumococcal infection include children and adults with chronic diseases of the cardiovascular, respiratory systems, diabetes mellitus, liver cirrhosis, chronic renal failure, Hodgkin's disease; children and adults with oncohematological diseases; HIV-infected; children and adults with cerebrospinal fluid leakage; children and adults after cochlear implantation; children and adults with sickle cell disease; with anatomical asplenia, or planning or having already undergone removal of the spleen. This should also include the so-called “organized” contingents (children attending kindergartens, students living in dormitories, military personnel, residents of nursing homes, prisoners and other adults and children living in overcrowded conditions). The presence of bad habits (alcohol, smoking) is also a risk factor.
SYMPTOMS
Symptoms of pneumococcal infection, which causes pneumonia, include fever, cough, shortness of breath and chest pain. Symptoms of pneumococcal purulent meningitis are a stiff neck, severe headache, fever, confusion and disorientation, and photophobia. The initial manifestations of pneumococcal bacteremia (blood poisoning, the most severe form with a mortality rate of up to 50%) may be similar to some symptoms of pneumonia and meningitis, and may also include joint pain and chills.
COMPLICATIONS AFTER AN Illness
Pneumococcal meningitis is particularly severe, the incidence of which is about 8 per 100 thousand children under 5 years of age. On average, about 83% of cases occur in children under 2 years of age. Despite the fact that pneumococcus occupies
the third position of post-hemophilic infection type b and meningococcal infection, and as an infectious agent responsible for the development of this disease, the prognosis for pneumococcal meningitis is much more serious. Complications in the form of mental retardation, impaired motor activity, epilepsy and deafness occur significantly more often than in the outcome of bacterial meningitis of other etiologies.
Pneumonia, caused by pneumococcus more often than others, is complicated by pulmonary empyema (accumulation of pus in the pleural cavity, causing a decrease in the respiratory surface of the lung tissue), which leads to death. Pneumococcal bacteremia in most cases (up to 80%) occurs with symptoms of fever without a focus of infection. The incidence of bacteremia caused specifically by pneumococcus
is 8-22% in young children. It is pneumococcal sepsis with the development of severe shock damage to organs that is the most severe and life-threatening form of pneumococcal infection. The frequency of this nosological form in children under 5 years of age averages 9,000 cases per year; the mortality rate reaches 20-50%.
According to world statistics, the proportion of pneumococcal otitis media ranges from 28 to 55% of all registered cases. Pneumococcal acute otitis media is characterized by a more severe course and a high risk of otogenic complications, including a tendency to perforation of the tympanic membrane. Pneumococcal otitis media is the most common cause of hearing loss in children.
Risk of developing pneumococcal infections:
- In healthy people, the risk is 8.8 per 100,000.
- In patients with diabetes mellitus – 51.4.
- In adults with chronic lung diseases – 62.9.
- In patients with chronic heart disease – 93.7.
- for those suffering from cancer – 300.4.
- For HIV-infected people – 422.9.
- In patients with oncohematological diseases - 503.1 per 100,000.
MORTALITY
According to WHO, pneumococcal infection is recognized as the most dangerous of all vaccine-preventable diseases and, before the introduction of universal vaccination, annually led to the death of 1.6 million people, of which from 0.7 to 1 million were children, which is 40% of the mortality rate of children of the first 5 years of life.
TREATMENT
A global problem in the world is the increasing resistance of pneumococci to antibiotics - this means that treatment of pneumococcal infections with antibiotics is often ineffective. The main factor in the development of antibiotic resistance in pneumococcus is the irrational use of antibacterial drugs. since, due to the rapid development of the disease (2-3 days), there is usually no time to determine sensitivity to antibiotics, and patients with severe pneumococcal infection often die, despite the introduction of standard antibacterial drugs.
EFFECTIVENESS OF VACCINATION
Vaccination is the only highly effective way to significantly influence the morbidity and mortality from pneumococcal infections and reduce the level of antibiotic resistance of pneumococcus
With evidence of the safety and effectiveness of pneumococcal conjugate vaccines, WHO and UNICEF believe it is necessary to include these vaccines for children in all national immunization programs. At the same time, it should be noted that the maximum protective effect is achieved with routine vaccination of all children under 2 years of age, and not just patients in risk groups.
According to WHO, world experience has shown that mass vaccination reduces the incidence of pneumococcal meningitis and severe pneumonia in children by more than 80%, and the incidence of all pneumonia and otitis media by more than a third. The carriage of pneumococci in children is decreasing, and accordingly, unvaccinated children and adults get sick less. The World Health Organization projects that global use of pneumococcal vaccination will prevent 5.4 to 7.7 million child deaths by 2030.
VACCINES
Vaccination has been used to combat pneumococcal infection for more than 30 years. Since 1981, the pneumococcal polysaccharide vaccine has been used. Since 2000, pneumococcal conjugate vaccines have been used in international practice for immunoprophylaxis of pneumococcal infection in young children.
To date, the following vaccines have been registered in Russia: two pneumococcal conjugate vaccines (10-valent and 13-valent - PCV10 and PCV 13) and one - polysaccharide 23-valent (PPV23). The latter is used in children over 2 years of age and adults. While conjugate vaccines are recommended for immunization of children from 2 months of age and adults aged 50 years and older. PCV13 is also registered in the US and EU for use in broader age groups (children 6 weeks to 17 years and adults 18 years and older). In 2013, the pneumococcal 13-valent conjugate vaccine Prevenar13 was awarded the Galen Prize as the best biotechnological product of the year. Vaccinations against pneumococcal infection have been included in the national preventive vaccination calendar since 2014. They are done for free. Vaccination 2 times at the age of 2 months and 4.5 months. Revaccination at 15 months.
Vaccination of children for whom immunoprophylaxis against pneumococcal infection was not started in the first 6 months of life is carried out twice with an interval between vaccinations of at least 2 months.
Latest epidemics
Most diseases are sporadic. Outbreaks of pneumococcal infection are uncommon, but can occur in closed communities, for example, in nursing homes, children's day hospitals and other similar institutions. However, large outbreaks of meningitis caused by serotype 1 have been reported in the African meningitis belt.
WHO estimates that of the 8.8 million children under 5 years of age who died in 2008, 476 000 (333 000 – 529 000) deaths were due to pneumococcal disease. Morbidity and mortality rates are higher in developing than in economically developed countries.