Concussion is one of the most common diagnoses in pediatric traumatology. Overall, traumatic brain injury (TBI) ranks first among all childhood injuries requiring hospitalization. Approximately 120 thousand children with concussion are admitted to Russian hospitals every year.
According to the severity, traumatic brain injury is divided into mild (concussion), moderate (mild to moderate brain contusion, with possible fractures of the cranial vault) and severe (severe brain contusions, intracranial hematomas with compression of the brain, fractures of the base of the skull). Fortunately, up to 90% of childhood TBIs are concussions, which is what this article will discuss.
The high level of injuries in children is explained by the child’s increased motor activity, restlessness and curiosity, which is combined with imperfect motor skills and coordination of movements, as well as a reduced sense of danger and fear of heights. In addition, in young children, the head has a relatively large weight, and the skill of belaying with hands has not yet been developed, so small children, as a rule, fall upside down and do not use their hands.
The causes of childhood TBI are very specific to each age group. Newborns in the total mass of victims make up 2%, infants - 25%, toddlers - 8%, preschool children - 20% and school-age children 45%.
Injuries in infants are primarily the result of the inattention and carelessness of their parents. Children under 1 year of age most often (more than 90%!) receive head injuries after falling from changing tables, beds, from parents' arms, from strollers, etc. You should never leave your baby alone in a place where he could fall. If you need to move away from your child at a distance greater than an outstretched hand, do not be lazy, put him in a crib, in a stroller with sides, in a playpen! One or two seconds is enough for the baby to roll to the edge of the changing table and fall.
From 1 year
babies begin to walk. The main cause of TBI is a fall from one’s own height, and a little later - falls from stairs, trees, roofs, windows, slides, etc. The episode of TBI itself is not always possible to identify. It should be borne in mind that if the child remained under the supervision of relatives, neighbors or a nanny, then they can hide from the parents the fact that the baby fell.
Older children
For various reasons, they themselves often hide the trauma.
In addition, children may experience brain damage without direct head trauma. These injuries usually occur when a child's body is subjected to sudden acceleration or deceleration (shaken baby syndrome). “Shaken baby” syndrome is most often observed before the age of 4-5 years
and can occur with rough handling, jumping from heights, and in young children even with excessively intense rocking.
Manifestations of a concussion
With a concussion, there are no gross, irreversible changes in the brain, and such an injury, being the most common, has the best prognosis and very rarely leads to complications.
It should be remembered that the brain of a child (and especially an infant) is significantly different from the brain of an adult. The course of a concussion in adults differs significantly from the course of this injury in a child.
In adulthood, a concussion is manifested by the following main symptoms: an episode of loss of consciousness from a few seconds to 10-15 minutes; nausea and vomiting; headache; amnesia (loss of memory) of events associated with the trauma (before the trauma, the trauma itself and after the trauma). In addition, some specific neurological symptoms are detected, such as nystagmus (twitching of the eyeballs), impaired coordination of movements and some others. The picture of a concussion in a child is completely different.
In children under 1 year
A concussion, as a rule, is asymptomatic. Loss of consciousness often does not occur; single or repeated vomiting, nausea, regurgitation during feeding, pale skin, causeless restlessness and crying, increased drowsiness, lack of appetite, and poor sleep are noted.
In preschool
More often it is possible to establish the fact of loss of consciousness, nausea and vomiting after injury. They experience headaches, increased or slow heart rate, instability of blood pressure, pale skin, and sweating. In this case, moodiness, tearfulness, and sleep disturbance are often noted.
Sometimes children experience a symptom such as post-traumatic blindness. It develops immediately after the injury or a little later, persists for several minutes or hours, and then disappears on its own. The reason for this phenomenon is not completely clear.
The characteristics of a child’s body lead to the fact that a long-term state of compensation can be replaced by a rapid deterioration of the condition. That is, immediately after the fall the child feels satisfactory, but after a while symptoms appear and begin to rapidly increase.
Diagnostic measures
Diagnosing concussion in children is quite a difficult task even for an experienced neurologist. Since, unlike more severe traumatic brain injury, this pathology is not characterized by structural changes in brain tissue that are detected using available research methods. It is also very difficult to collect complaints and a reliable history of the disease in a child.
Neurological status examination
During the initial examination, a pediatric neurologist collects complaints, life history and illnesses. Young children are not able to provide this information, so everything that happened to the baby should be remembered well and then reported to the doctor by those who were near the child at the time of the injury.
The specialist will be interested in the following questions:
- Under what circumstances did the injury occur?
- Was there a loss of consciousness, limpness, or a sharp cry in the child?
- Did you vomit or convulse after hitting your head?
- Have there been any traumatic brain injuries, etc., before this incident?
If the doctor manages to collect a reliable history, this will greatly facilitate the diagnosis and allow the correct treatment to be prescribed.
X-ray of the skull
X-ray of the skull, or craniography, is a mandatory examination method for head trauma in children. The presence of cracks or fractures in the bones of the skull excludes a concussion.
Ultrasound
Infants, thanks to an open fontanel, can undergo a neurosonographic study, which will exclude contusion lesions in the brain tissue, the presence of hematomas in the cranial cavity, as well as increased intracranial pressure. Older children undergo echoencephaloscopy, which indirectly assesses the state of the brain using the M-echo response. With a concussion, the brain does not become displaced, which indicates the absence of a more severe traumatic brain injury.
EEG
An electroencephalogram is a method of recording the electrical potentials of the brain. During a concussion, a change in the α-rhythm is revealed, namely its unevenness, and zonal differences disappear. Complexes of sharp waves can also be detected. The use of provoking tests (hyperventilation, etc.) can cause paroxysmal slow-wave activity.
CT or MRI
When carrying out neuroimaging diagnostic methods (CT or MRI), focal changes in brain tissue or expansion of the ventricular system and subarachnoid space are not detected. An indirect criterion for a concussion can be signs of swelling of the brain or its membranes detected on MRI.
Consultation with an ophthalmologist
The complex of mandatory diagnostic measures for concussion in children includes consultation with an ophthalmologist.
When examining the condition of the fundus, a pink optic disc with fairly clear boundaries is observed; vascular tone most often remains unchanged. Occasionally, slight venous congestion is detected. It must be remembered that the diagnosis of any traumatic brain injury should be carried out by a qualified specialist, since the health of your child depends on it.
We are taking urgent measures
What should parents do if their child has suffered a traumatic brain injury? There is only one answer: the child should definitely and urgently be shown to a doctor. It is best to immediately call an ambulance, which will definitely take the child to a hospital with pediatric neurosurgeons or neurologists. And this measure is not unnecessary. With minimal symptoms and complaints, the baby may have severe brain damage. The long-term visible well-being of the child, the absence of symptoms, especially with hemorrhages in the brain, often after a few hours and even days is replaced by a progressive deterioration of the condition, which begins with a change in the child’s behavior, his increased excitability, there may be nausea, vomiting, nystagmus, and in infants the fontanelle bulges , then drowsiness appears, depression of consciousness is observed.
Traumatic brain injury in children
There are several forms of TBI based on the nature and severity of brain damage:
- Brain concussion.
- Brain contusion: mild; moderate; severe.
- Diffuse axonal damage.
- Brain compression: epidural; subdural; intracerebral hematoma; depressed fracture; subdural hygroma; focus of brain contusion.
Brain concussion. With a concussion, a child may be conscious or lose consciousness for several seconds or minutes, but the bones of the skull are not damaged. The appearance of amnesia is typical, which manifests itself in different forms: retrograde (lack of memories of what happened before the TBI), congrade (lack of memories of what happened during the TBI, when the child had impaired consciousness) or anterograde (the child does not remember anything). Usually, with a concussion, amnesia is short-term, accompanied by nausea and vomiting. After regaining consciousness, they usually complain of weakness, headache, dizziness, tinnitus, sweating, flushing of the face, and sleep disturbances. Sometimes children experience vestibular hyperesthesia and pain when moving the eyeballs, short-term mild asymmetry of deep reflexes, hyperhidrosis, and small-scale nystagmus. Vital functions are not damaged. The general condition of patients usually improves during the first, less often the second, week after injury.
Brain contusion is focal macrostructural damage to the brain matter, ranging in mild, moderate and severe degrees.
A mild brain contusion is characterized by loss of consciousness for several minutes or even tens of minutes. After regaining consciousness, the main complaints are headache, dizziness, nausea and vomiting. Amnesia lasts longer than with a concussion. In children, moderate bradycardia or tachycardia and arterial hypertension are observed. As a rule, vital functions are not damaged. Neurological symptoms include mild anisocoria nystagmus, signs of pyramidal insufficiency, subarachnoid hemorrhage - meningeal symptoms. With a mild injury, there may be a fracture of the bones of the cranial vault. On the 3-5th day, consciousness is restored, the child begins to navigate space and time. But at the same time there may be memory disorders about current events and problems in intellectual activity. Neurological symptoms disappear on the 10-14th day. With a mild injury, local swelling of the brain substance, pinpoint diapedetic hemorrhages, and limited rupture of small pial vessels occur.
A moderate brain contusion leads to loss of consciousness for tens of minutes or hours. During the first 3-5 days after injury, children experience moderate stupor, speech dysfunction, severe lethargy, adynamia, drowsiness, fatigue, disorientation in space and time, amnesia (retrograde) and amnesia for events during injury. There may be fractures of the bones of the cranial vault and base, subarachnoid hemorrhage, and small focal hemorrhages. But with a bruise, not only the cortical zone, but also the white matter of the brain can be damaged. Children complain of headaches, repeated vomiting, and sometimes mental disorders are observed. Many patients have indicators of focal damage to the cerebral hemispheres in the form of contralateral hyperreflexia, central paresis of facial muscles, nystagmus, the reaction of the pupils to light decreases, pathological foot signs appear, mono- or hemiparesis, speech disorders (dysarthria), as well as motor, sensory or amnestic aphasia. In some cases, cerebellar and meningeal symptoms can be observed. The bruises resolve in about 14-18 days.
With a severe brain injury, the patient loses consciousness for several hours or several weeks. In this case, disturbances in vital functions occur, arterial hypertension or hypotension, bradycardia or tachycardia, respiratory failure, and hyperthermia appear. Clinical symptoms include: gaze paresis, paresis and paralysis of the limbs, swallowing disorders, floating movements of the eyeballs, nystagmus, bilateral mydriasis or miosis, generalized or focal seizures, speech disorders, mental changes. Often, with a severe brain contusion, there is a fracture of the vault and base of the skull, massive subarachnoid hemorrhage, brain tissue is destroyed, the configuration of the grooves and convolutions is lost, and connections with the soft meninges are severed.
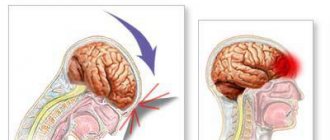
Diffuse axonal brain damage is most often caused by car accidents or falls from a great height; in these cases, the injury has a sharp acceleration and deceleration . This injury causes tension and rupture of axons in the white matter of the hemispheres and the brain stem. Symptoms of diffuse axonal brain damage are characterized by: prolonged coma. Motor excitation is replaced by adynamia, and tetraparesis may appear. Patients may experience coma, which often develops into a prolonged vegetative state. Such patients have a high mortality rate.
Compression of the brain. Compression of the brain is caused by intracranial hematomas, depressed fractures of the skull bones, areas of crushing of the brain, and entrapment of the brain stem. Clinically, compression of the brain is expressed by a life-threatening increase in general cerebral and focal disorders after a certain period of time after injury or immediately after it. This period is called the “light interval” - this is the period of time during which the victim’s consciousness is fully or partially restored between the primary and secondary loss. In patients it happens individually: for some it is complete, for others there is stunning without recovery, for others there is no recovery at all. The duration of the light interval is minutes or hours, and in some cases it is calculated in days and weeks.
There are closed and open TBI . With a closed TBI, the scalp is not damaged, there are only soft tissue wounds without disruption of the aponeurosis. Open TBI is accompanied by a fracture of the calvarial bones, the aponeurosis is damaged, there may be a fracture of the base of the skull, bleeding or liquor leakage (from the ear or nose). In addition, TBI is divided into penetrating (with damage to the dura mater) and non-penetrating (without damage to it).
In case of TBI, the following states of consciousness are distinguished: clear, moderate stupor, deep stupor, stupor, moderate coma (I), deep coma (II), terminal coma (III).
With clear consciousness, the patient has preserved mental functions: wakefulness, full orientation, adequate reactions. Amnesia is possible in the form of retro-, con- or anterograde. In children, stupor in the form of depression can be observed, while consciousness is preserved, the threshold of sensitivity to external stimuli is increased, and the patient’s activity is reduced.
Stupor is a deep depression of consciousness, in which coordinated defensive reactions and opening of the eyes in response to pain and other irritants are preserved.
Coma is a shutdown of consciousness; the patient does not perceive himself or the world around him. Coma I - the patient's eyes are closed, pupillary reflexes are preserved, protective movements are discoordinated. Coma II – there are no protective movements to pain, pupillary reflexes are depressed, spontaneous breathing and cardiovascular activity are impaired. Coma III - muscle atony, bilateral fixed mydriasis, immobility of the eyeballs, severe respiratory distress, tachycardia, low blood pressure.
Hematomas usually lead to compression of the brain during TBI:
An epidural hematoma is a traumatic hemorrhage between the inner surface of the skull bones and the dura mater, causing local and general compression of the brain. Most often, rupture of dural vessels creates the preconditions for the formation of an epidural hematoma (EH) at the site of impact. Among all cases of TBI, the frequency of EG is 0.5-0.8%. The volume of the EG is on average 80-120 ml, the diameter is 7-8 cm, the predominant localization is the temporo-parietal, temporo-frontal, temporo-basilar regions. EG consists of liquid blood and clots, pressing on the underlying dura mater and brain matter. The most common source of bleeding in EG is the damaged middle meningeal artery and its branches, sometimes meningeal veins, sinuses and diploe vessels. Symptoms are characterized by: lucid interval, homolateral mydriasis, contralateral hemiparesis, bradycardia, and arterial hypertension are common.
Subdural hematoma is a traumatic hemorrhage between the dura mater and the arachnoid mater, causing general or local compression of the brain. Unlike EG, subdural hematoma (SH) occurs not only on the side of the injury, but also on the opposite side. The volume of SG ranges from 30 to 250 ml, on average 80-150 ml. They can occupy an area of 10x12 cm or more. The formation of SG is usually associated with rupture of the pial veins. Often the source of HS is damaged superficial vessels of the cerebral hemisphere (cortical arteries). SGs are located predominantly on the convex side of the hemispheres in the parieto-frontal, parieto-temporal regions, sometimes spreading to the anterior and middle cranial fossae. The classic variant of the course of acute HS is rare and is characterized by a three-phase change in the state of consciousness: primary loss at the time of injury, a clear interval of up to 2 days, secondary loss of consciousness. Focal symptoms are expressed in the form of homolateral mydriasis, contralateral paresis, then secondary stem syndrome develops. Focal symptoms include speech disorders, hemiparesis, and extrapyramidal symptoms.
As a result of TBI, subdural hygroma in the form of a limited accumulation of cerebrospinal fluid in the subdural space with compression of the brain. Subdural hygroma occurs due to rupture of the subarachnoid cisterns, most often at the base of the brain. The clinical picture usually includes meningeal symptoms, often mental disorders such as frontal syndrome, and progressive bradycardia and convulsive syndrome are typical.
Complications and consequences of traumatic brain injury
Complications of TBI are divided into intracranial and extracranial . Among intracranial complications, the most dangerous are meningitis, encephalitis, and brain abscess. Brain abscess can be early, developing within the first 3 months. after TBI, and late, after 3 months. after injury. Usually an abscess is one of the outcomes of encephalitis, so in its development it goes through 3 stages: purulent-necrotizing encephalitis, the formation of a pyogenic capsule and the manifestation of an abscess, the terminal stage.
Extracranial complications of TBI include pneumonia, acute heart failure, and impaired liver and kidney function.
The most common consequence of injury is asthenic syndrome with increased fatigue, irritability, lack of self-confidence, a tendency to limit external contacts, and isolation. Many patients develop vegetative dystonia syndrome, characterized by arterial hyper- and hypotension, sinus tachybradycardia, and impaired thermoregulation.
One of the severe consequences of TBI is post-traumatic epilepsy, which develops in 10-20% of victims. Usually forms during the first 18 months. after TBI. Its clinical manifestations depend on the nature of the TBI. Thus, in patients who have suffered a brain contusion, a focal type of epileptic seizures is more often observed, in those who have suffered a concussion or compression of the brain, a generalized type is observed. It is assumed that convulsive syndrome in the first 2-3 months. The consequences of TBI include gross morphological disorders of brain tissue in the form of an intracerebral cyst, atrophy in the frontal and parietal lobes, and intracerebral calcification.
Among the clinical forms of TBI in childhood, concussion and mild brain contusion predominate. It should be emphasized that TBI in children is characterized by a discrepancy between the degree of its severity and the developing consequences. It should be noted that at an early age, children still have open fontanelles, the skull bones are pliable, and the sutures have not yet healed, so there are no general cerebral symptoms in the presence of an intracranial hematoma. At the same time, the high hydrophilicity of tissues in children contributes to an easier occurrence of cerebral edema. In children, especially young children, loss of consciousness can last 1-2 seconds, which is usually difficult to detect. Children are often stunned, lethargic, and drowsy. Only in children over 4 years old can the presence of retrograde amnesia be established. Vomiting may be one-time or repeated over several days. Infants with TBI experience frequent regurgitation and dyspeptic symptoms.
With brain contusions in children, general cerebral symptoms predominate over focal ones, behavior often changes, and vegetative manifestations are pronounced. Of the focal symptoms, pyramidal insufficiency is the most consistent, but young children may not have these symptoms. Asymptomatic or low-symptomatic TBI in childhood, the predominance of general cerebral symptoms over focal symptoms even in cases of brain compression make early diagnosis of TBI in children difficult. In infants, bone fractures often occur, which is explained by the thinness of the skull bones and the absence of the diploic layer. Features of brain damage at this age include rupture of brain tissue due to injury. Hemorrhagic manifestations are rare, but ischemic foci often occur in the basal ganglia and internal capsule. Intracranial hematoma is less common in childhood than in adults. Among them, epidural hematoma is most often observed; the source of bleeding is the vessels of the dura mater. In early childhood, the dura mater is well supplied with blood.
In children, symptoms of brain compression by a hematoma are initially mild. Subdural hematoma in the first half of life is usually caused by rupture of veins near the superior sagittal sinus. It is known that one of the reasons for the rupture of these veins may be excessive motion sickness in children. With a subdural hematoma in children there is often no clear space. Isolated traumatic intracerebral and intraventricular hemorrhages in young children are rare; they are observed mainly at school age.
The consequences of TBI in childhood depend on the severity of the injury, age and premorbid background. The most severe consequences of TBI are in young children. This is due to insufficient differentiation of cells in the cerebral cortex, weakness of inhibitory processes, and incomplete myelination of nerve fibers.
Diagnosis of concussion
In the hospital, the child is examined by a pediatric neurologist, neurosurgeon or traumatologist. He carefully ascertains complaints, collects anamnesis (history of the disease), and conducts a general and neurological examination. Additional diagnostic methods are prescribed. The main ones are skull radiography, neurosonography (in young children), echo-encephalography (Echo-EG). If necessary, computed tomography of the brain (CT), magnetic resonance imaging (MRI), electroencephalography (EEG), lumbar puncture.
Radiography
skull is performed in most patients. The purpose of this study is to identify skull fractures. The presence of any damage to the bones of the skull automatically transfers the injury to the category of moderate or severe (depending on the condition of the child). Sometimes in young children with a favorable clinical picture, linear fractures of the skull bones are revealed on radiographs. It is impossible to judge the state of the brain substance from radiographs.
Neurosonography
(NSG) is an ultrasound examination of the brain.
Neurosonograms clearly show the substance of the brain and the ventricular system. You can identify signs of cerebral edema, areas of contusion, hemorrhages, and intracranial hematomas. The procedure is simple, painless, quickly performed, and has no contraindications. It can be done multiple times. The only limitation of neurosonography is the presence of so-called “natural ultrasound windows” - a large fontanelle or thin temporal bones. The method is very effective in children under 2 years
. Later, ultrasound becomes difficult to pass through the thick bones of the skull, which dramatically degrades image quality. Equipment for performing neurosonography is available in most children's hospitals.
Echo-encephalography
(Echo-EG) is also an ultrasound research method that allows you to identify displacement of the structures of the midline of the brain, which may indicate the presence of additional space-occupying formations of the brain (hematomas, tumors), and provide indirect information about the state of the brain substance and the ventricular system. This method is simple and fast, but its reliability is low. Previously, it was widely used in neurotraumatology, but with the availability of modern diagnostic tools, such as neurosonography, computed tomography and magnetic resonance imaging, it can be completely abandoned.
The ideal method for diagnosing brain damage and diseases is computed tomography.
(CT). This is an x-ray research method in which high-definition images of the skull bones and brain matter can be obtained. CT can diagnose almost any damage to the bones of the vault and base of the skull, hematomas, bruises, hemorrhages, foreign bodies in the cranial cavity, etc. The accuracy of this study is very high. Its main disadvantage is that the CT machine is expensive, and not every hospital has it.
Magnetic resonance imaging
(MRI) is the most accurate, but complex and expensive method of examining the central nervous system. It is rarely used to diagnose acute traumatic brain injury because it does not allow the bones of the skull to be seen, is less accurate for recognizing acute hemorrhages, takes longer than computed tomography, and often requires anesthesia when examining small children - the child must lie absolutely still for 10 -20 minutes, but small children cannot do this; In addition, very few clinics can boast of having magnetic resonance imaging scanners.
Advertising
Electroencephalography
(EEG) allows you to study the bioelectrical activity of the brain. It is used for special indications to assess the severity of traumatic brain injury and identify foci of epileptic activity. A focus of epiactivity is an area of the cerebral cortex with pathologically altered activity of neurons (nerve cells), which can lead to epileptic seizures.
Lumbar puncture
- this is the collection of cerebrospinal fluid (the fluid that bathes the brain and spinal cord) from the spinal canal at the lumbar level. Changes in the cerebrospinal fluid may indicate injury or hemorrhage (the presence of blood) or an inflammatory process, meningitis. Lumbar puncture is performed extremely rarely and only for special indications.
What is a concussion and why is it dangerous?
A child's fall, violation of rules of conduct on the playground, or simply an unfortunate set of circumstances can result in not only a bump or a cut in the skin, but also a more serious head injury.
Concussion is the most common type of consequence among all types of damage to the brain. It is characterized by reversible disruptions in the functioning of the central nervous system. The mechanism of development of the condition is based on disruption of connections between the cells of the medulla.
Experts distinguish three stages of development of a bruise:
- acute – the period of onset of symptoms of pathology, which lasts up to 10 days;
- intermediate – six months from the moment of injury, during which brain functions should be fully restored;
- long-term – up to 2 years from the moment the first symptoms appear, when either complete recovery should occur, or pathological consequences may appear.
In childhood, as a result of bruises and falls, a mild degree of pathology is usually observed, which does not threaten any permanent negative consequences. In some cases, there is still a possibility of developing serious complications. These include cerebral edema, hemorrhages, and post-traumatic epilepsy. Among the long-term consequences, early aging of the central nervous system organ stands out. It significantly reduces life expectancy and affects the general condition of a person.
Consequences of TBI
Research on traumatic brain injury shows that even mild trauma can cause undesirable consequences.
Under the influence of trauma (the moment of mechanical damage to the brain substance) and its consequences, the functions of various parts of the brain are disrupted, and, consequently, the work of the organs and systems subordinate to them (endocrine, digestive systems, etc.). Blood flow may be impaired, including the outflow of venous blood from the cranial cavity. The regulation of vascular tone suffers - they can narrow inadequately, leading to increased blood pressure. All this worsens the course of metabolic processes in the brain, as a result of which brain cells can be replaced by cystic cavities, that is, holes filled with fluid form in their place, and in the place where these cysts are, certain brain functions are lost. For example, the frontal lobes are responsible for intelligence, which means that the presence of cysts in this place reduces it. In addition, it is known that the brain normally has spaces inside and outside filled with cerebral (cerebrospinal) fluid. After injury, it can accumulate excessively in them - and consequently, intracranial pressure increases. The fluid under pressure compresses the substance of the brain, causing its slow atrophy5 (this phenomenon can also occur during the formation of cysts).
The triggering of pathological mechanisms of injury depends on its severity: the more severe it is, the more pronounced the disorders, the worse the outcomes, and the longer the recovery period.
5Atrophy (from the Greek atrophia; a - absence of a sign or quality, trophe - nutrition) - a decrease in the mass and volume of an organ or tissue as a result of a nutritional disorder, accompanied by a weakening or cessation of their functions.
For mild traumatic brain injury, the prognosis is usually favorable, provided that the recommended regimen and treatment are followed. After recovery, phenomena of asthenia are possible - the child quickly gets tired, becomes inattentive, and irritable. At the same time, the baby is more inhibited, which can lead to repeated injuries. These phenomena can affect the child’s intellectual development in the future.
In case of moderate TBI, the phenomena of asthenia may be accompanied by increased intracranial pressure, frequent headaches, and loss of coordination.
With severe TBI, the prognosis can be unfavorable - mortality in these cases reaches 15-30%. After recovery, a wide variety of consequences are possible: from varying degrees of motor impairment, severe convulsive attacks to severe mental disorders and consciousness, which leads to disability.
With open TBI, purulent-inflammatory complications often occur (for example, meningitis - inflammation of the membranes of the brain, etc.), which can also lead to death.
There is still no clear answer to the question of how long it takes for the body to fully recover, even after a mild TBI. It was believed that after such an injury, recovery occurs within a few days, a maximum of 2-3 weeks. But studies have shown that 1-3 months after a concussion, at least half of the children show certain deviations from the norm, which sometimes persist for a longer time. The speed of recovery depends primarily on the severity of the injury, the age and previous health of the child.
Among various injuries to the body, head injuries account for 30-50% of all injuries in children. And every year this figure increases by 2%.
Advertising
Signs of a concussion in a child under 1 year of age
Most children begin to speak by age two and are able to express emotions, which helps parents understand whether their child is sick or not. Family members may notice uncharacteristic signs of behavior in a young child:
- Loss of orientation in space.
- Loss of coordination.
- Lethargy.
- Loss of consciousness.
- Pale skin tone on the face and body.
- Bad, restless sleep.
- Sudden loss of appetite.
- Nausea, vomiting.
- Abdominal pain.
- Headaches (“rumbling in the head”).
- Loss of concentration.
Attentive parents who notice these symptoms should immediately consult a doctor. In newborn infants, the first symptoms are very vague as they are often similar to other disorders.
After an injury, you should pay attention to the following symptoms:
- Restless crying.
- Decreased appetite, even to the point of absence.
- Frequent regurgitation.
- Enlargement or displacement of the fontanel.
- Paleness of the skin.
- Restless sleep or lack thereof.
Attention! The first symptoms of TBI can appear both in the first hours after injury and within 24 hours. Therefore, it is necessary to carefully monitor the condition and well-being of the child during this period.
Diagnostics
When an injury occurs, a child undergoes consultation with a pediatrician, traumatologist, neurologist and surgeon. In addition, a blood test and a visit to an ophthalmologist to check the fundus of the eye are prescribed. In some cases, instrumental studies are required, including:
1. Ultrasound examination. Helps determine the condition of brain tissue.
2. Neurosonography. Allows you to detect the presence of hematomas, hemorrhages and edema.
If the child’s age allows for a wider range of studies, the following instrumental methods are prescribed to assess the severity of the concussion:
1. Radiography. Shows the presence of bone damage in the skull.
2. Magnetic resonance imaging. Allows you to identify hemorrhages and neoplasms.
3. Electroencephalography. Identifies areas of the brain that have increased activity.
4. Lumbar puncture, which is the collection of material for the study of fluid from the spinal cord.
5. Echoencephalography. Shows the condition of the cerebral ventricles, the presence of hematomas or displacements.
Depending on the symptoms and examination data, the severity of the concussion is determined. Doctors will always offer the option of hospitalization if a child has a brain pathology of any severity. However, if the disease is mild, outpatient observation may be suggested.
What to do first if a child falls
We strongly advise parents whose children have suffered a head injury: even if, in your opinion, nothing bothers the baby, he fell from a small height, stopped crying, etc., immediately seek help from the following doctors: a pediatric neurologist, a traumatologist, a neurosurgeon. To do this, you need to call an ambulance at home and you and your child will be taken to a specialized hospital. Or, go to the emergency surgery department of any large children's hospital yourself, where the child will be consulted by the specified specialists. If they do not confirm the pathology, you can safely return home.
Failure to consult a doctor is dangerous due to late diagnosis of the injury, worsening of the child’s condition, and the possibility of coma. All this requires treatment in intensive care, and in some cases, surgical intervention. Delayed consultation with a doctor increases the risk of death and complications, lengthens the recovery period and worsens its outcome, to the point that the child may become disabled.
Treatment tactics for TBI
After the examination and clarification of the diagnosis, treatment tactics are determined. Drug treatment is prescribed (therapy aimed at eliminating cerebral edema, lowering intracranial pressure, correcting metabolism and blood flow in the brain, etc.). Surgical treatment is used (and necessary) primarily to eliminate compression of the brain. It is prescribed to children with depressed fractures of the skull bones and intracranial hemorrhages.
Parents need to realize that only a comprehensive, adequate examination of the child allows for correct and timely treatment of brain injury, achieving recovery and avoiding disability.
Where is TBI treated?
According to existing rules (standards), all children with traumatic brain injury must be hospitalized. Children with a concussion (mild traumatic brain injury) can be treated in the neurological and neurosurgical departments. Patients with more severe forms of injuries should be treated in a neurosurgical department (if one is available in a particular region).
Carrying out justified, targeted treatment requires a comprehensive examination of the child, which is only possible in a hospital.
This examination includes thorough examinations of the nervous system, vestibular system, organs of vision, hearing and other studies.
In the emergency department, the child is examined, signs indicating damage to the skull bones or brain injury are identified, the parents are asked about the child’s condition after the fall, etc.
The first symptoms in a baby
- Strong restless crying, with short-term cessation of breathing.
- Paleness of not only the skin, but also the mucous membranes. Often due to lack of blood flow, bluish lips and areas of skin may appear.
- Regurgitation, body temperature can rise to 38 degrees.
Excessive crying and elevated body temperature are the main indicators of traumatic brain injury. Infants are often left with bruises and contusions after injury , but due to the elastic skull, severe injuries are unlikely.
Much more dangerous signs of a concussion in a child under 1 year of age, requiring immediate hospitalization, are:
- Swelling, displacement, curvature of the fontanel.
- Decreased or absent reflexes.
- Impaired motor function of the eye - rolling of the eyes (or eyes), squint, drooping eyelid.
- Complete lack of appetite.
If parents do not consult a doctor in time, a concussion carries a number of complications:
- Strabismus.
- Developmental delay (or even mental retardation).
- The child will suffer from headaches.
- Hyperkinesis is uncontrolled movements of body parts.
- Vegetative-vascular disorders.
Features of concussion in children under 2 years of age
According to statistics, 9 out of 10 children with TBI are diagnosed with a concussion. The reason for this is that in children under two years of age the head is larger and heavier, and the coordination of the body does not allow it to react in a timely manner to a fall, so in infancy the child’s head is the first to suffer.
The harder the impact, the greater the likelihood of a concussion, despite the fact that the bones of the baby’s skull are strong, and the cerebrospinal fluid prevents the brain cells from colliding with the tissues of the skull.
Reference. Liquor is a fluid that circulates in the anatomical spaces of the spinal cord and brain.
In children under one year of age, the fontanel has not yet closed and with a sharp blow, it can easily become dislodged, which will lead to serious health problems in the future. You may also be interested in the reasons for the appearance of balls on the scalp in children.