Additional vaccination against polio in questions from parents and answers from Dr. Komarovsky
Poliomyelitis is a viral infection (viral means there are no drugs that can kill the pathogen). It is transmitted through the mouth: by water, that is, as a disease of dirty hands. The only effective method of prevention is vaccination.
Read about polio and polio vaccines here (small document).
***
To understand further text, here is some brief information about vaccines.
OPV (oral polio vaccine) is a vaccine containing a live, attenuated polio virus. Dripping into the mouth - 2 drops on the tongue.
IPV is a polio vaccine containing inactivated (killed) polio virus. It is administered by injection (injection). IPV may be included in combination vaccines, such as Infanrix and Pentaxim.
Questions and answers
My child is vaccinated according to the calendar (in whole or in part). Should I agree to additional polio vaccination? If yes, then why is it needed?
Active circulation of polio viruses has been confirmed in Ukraine. It (this circulation) can be interrupted by simultaneous mass vaccination of children with OPV, which is carried out in several rounds.
Children who are correctly vaccinated according to the calendar using IPV have virtually no risk of getting sick, but can be carriers (and spreaders) of the virus, since IPV (unlike OPV) does not form local immunity in the intestines.
That is why additional OPV vaccination is recommended for such children. The purpose of additional polio vaccination is not so much to protect a given child, but to stop the circulation of the virus in the country.
It is fundamentally important that for children initially vaccinated with IPV, subsequent OPV vaccination is absolutely safe.
My child is not vaccinated at all. Can he receive polio drops?
If the child is more than 2 months old and has never been vaccinated against polio, vaccination should begin with IPV.
OPV is administered no earlier than 2 weeks after IPV.
I know that the vaccine was thawed and then frozen again. What does it mean? Is it dangerous?
For those vaccinated, it means nothing and poses no danger. WHO, the vaccine manufacturer and the Ministry of Health have confirmed that repeated freezing of the vaccine does not affect its effectiveness and safety. Some journalists, some businessmen close to the Ministry of Health who have lost the opportunity to make money by purchasing a vaccine, and all professional opponents of vaccinations do not agree with this, so you have the opportunity to read about this regularly.
Can I determine if the vaccine was stored incorrectly?
WHO experts and the vaccine manufacturer officially advise that OPV is heat sensitive, so its quality must be carefully monitored using temperature indicators.
Parents have the opportunity to personally verify the suitability or unsuitability of the vaccine.
All bottles are equipped with a thermal indicator (usually located on the label). The thermal indicator is a square located inside a circle. If the bottle is exposed to excessive heat, the square will darken. You can only use bottles where the inner square is lighter than the outer circle.
Is the polio vaccine dangerous for a child?
Both OPV and IPV are among the safest vaccines. The only serious complication of OPV is the so-called vaccine-associated polio (VAP). The vaccine is live, so some unvaccinated children (on average 1 in 3 million) may develop the disease after vaccination. It is in order to avoid VAP that vaccination begins with IPV - the inactivated vaccine creates immunity sufficient to prevent VAP.
In other words:
- IPV is not dangerous in principle;
- OPV is dangerous to the unvaccinated;
- OPV is not dangerous for those previously vaccinated with IPV.
Is a child vaccinated with a live polio vaccine dangerous to others?
A child vaccinated with OPV releases live virus into the environment for some time, i.e., it is a source of infection. For those fully or partially vaccinated against polio, there is no risk. For those who are not vaccinated at all, theoretically there is a risk of the disease, and it is 1 case per 7–14 million vaccinations. However, even this risk can be reduced by observing basic rules of personal hygiene (reminder: polio is a disease of dirty hands).
Taking into account the extremely low probability of developing VAP in contacts, there is no need for any isolation, bans or quarantines, and such measures are not taken in any country in the world.
***
In conclusion, a few words about my attitude to the “document” of an anonymous group of authors who are hiding under the guise of the “Civil Rights Defense League.”
The main thing in my opinion is my enormous disappointment due to the fact that many people are seriously considering and actively disseminating this anonymous verbiage, built on incomplete, unreliable and deliberately false information and, moreover, created by an organization that is professionally engaged in anti-vaccination activities.
We also recommend listening.
author Komarovsky E.O. published 26/10/2015 13:22 updated 31/01/2018
Vaccines
There are two types of vaccines to prevent polio—live oral polio vaccine (OPV) and inactivated polio vaccine (IPV). OPV provides essential protection for children against polio. If used repeatedly, it protects the child for life. All available evidence indicates that OPV is not teratogenic and is safe for pregnant women and HIV-infected individuals. However, rare serious adverse events associated with OPV may include vaccine-associated paralytic polio (VAPP) among vaccinated individuals and their contacts, and the emergence of vaccine-derived polioviruses (VDPV). The incidence of VAPP is estimated to be 2–4 cases per million births per year in countries using OPV. The introduction of at least one dose of IPV before OPV vaccination leads to the elimination of VAPP. Let us remind you that in the National Calendar of Preventive Vaccinations of the Russian Federation, the first two (!) vaccinations against polio are given with inactivated polio vaccine!
IPV is considered a highly safe vaccine whether given alone or in combination with other vaccines. There is no evidence of a cause-and-effect relationship with adverse events other than mild local erythema (0.5-1%), tissue induration (3-11%), and tenderness (14-29%).
More about vaccines
What vaccination is given against polio?
Parents often ask at what age is the polio vaccine given? A doctor can answer this question, since much depends on the vaccination plan and what drug is used for vaccination. Until 2010, not a single case of polio was recorded in Russia, so children were vaccinated using an inactivated vaccine
, which did not contain live viruses.
Injections of the drug were given to the child in the first two years of life
, and then revaccination was carried out
at the age of 14
. Unfortunately, inactivated, i.e. The “dead” vaccine is not capable of providing a child with protection against the “wild strain” of polio, so they decided to replace the inactivated vaccine with a “live” one.
The “live” vaccine contains live but weakened viruses.
, it is believed that a live vaccine helps the body develop the necessary immune response to the “wild strain” of the polyvirus.
However, a live vaccine is not used throughout the entire vaccination course; the first two vaccinations for babies are still given using an inactivated vaccine
.
Polio
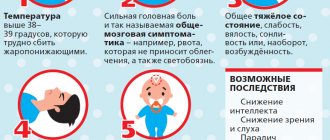
The incubation period for various forms of polio averages 8–12 days.
Inapparate form
Poliomyelitis is a carriage of the virus, which does not manifest itself clinically and can only be detected in the laboratory.
Abortive (visceral) form
polio accounts for more than 80% of all cases of the disease. Clinical manifestations are nonspecific; Among them, general infectious symptoms predominate - fever, intoxication, headache, moderate catarrhal symptoms, abdominal pain, diarrhea. The disease ends after 3-7 days with complete recovery; no residual neurological symptoms are noted.
Meningeal form
Poliomyelitis occurs as benign serous meningitis. In this case, two-wave fever, headaches, and moderately severe meningeal symptoms (Brudzinsky, Kernig, stiff neck) are noted. After 3-4 weeks recovery occurs.
Paralytic form
Poliomyelitis has the most severe course and outcomes. In the preparalytic period, general infectious symptoms predominate: fever, dyspepsia, rhinitis, pharyngitis, tracheitis, etc. The second wave of fever is accompanied by meningeal phenomena, myalgia, pain in the spine and limbs, severe hyperesthesia, hyperhidrosis, confusion and convulsions.
Approximately on days 3-6, the disease enters a paralytic phase, characterized by the sudden development of paresis and paralysis, most often of the lower extremities, with preserved sensitivity. Paralysis due to poliomyelitis is characterized by asymmetry, unevenness, and predominant damage to the proximal limbs. Somewhat less frequently, paresis and paralysis of the upper limbs, face, and trunk muscles develop with polio. After 10-14 days, the first signs of muscle atrophy are observed. Damage to the vital centers of the medulla oblongata can cause paralysis of the respiratory muscles and diaphragm and cause the death of a child from acute respiratory failure.
During the recovery period of polio, which lasts up to 1 year, tendon reflexes are gradually activated and movements in individual muscle groups are restored. The mosaic nature of the lesion and uneven recovery causes the development of atrophy and muscle contractures, growth retardation of the affected limb, the formation of osteoporosis and bone tissue atrophy.
In the residual period, residual effects of poliomyelitis are observed - persistent flaccid paralysis, contractures, paralytic clubfoot, shortening and deformation of the limbs, hallux valgus, kyphoscoliosis, etc.
The course of polio in children can be complicated by pulmonary atelectasis, pneumonia, interstitial myocarditis, gastrointestinal bleeding, intestinal obstruction, etc.
Prevention
In 1988, governments created the Global Polio Eradication Initiative
(GPEI) to rid humanity of this disease forever. Following widespread use of the polio vaccine, the incidence of the disease fell sharply in many industrialized countries. Since 1988, the number of polio cases has decreased by more than 99%, from 350,000 to 73 cases reported in 2015, according to WHO. All infants and children should be vaccinated against polio. The American Academy of Pediatrics recommends vaccination at 2 months, 4 months, and 6 to 18 months, and a booster dose at 4 to 6 years of age, and childhood vaccination confers immunity in >95% of recipients.
Adults are usually not vaccinated. Unvaccinated adults traveling to endemic or epidemic areas should be vaccinated with IPV; Vaccination includes 2 doses administered 4–8 weeks apart and a 3rd dose 6–12 months later. At least 1 dose - before travel. Vaccinated adults traveling to endemic or epidemic areas should receive 1 dose of IPV again. Immunocompromised patients and their households should not use OPV.
If we talk about the prevention of polio at the household level, it means: refusal to swim in dirty bodies of water that are not suitable for this; compliance with personal hygiene rules; refusal of potentially dangerous products. In this sense, raw milk is undesirable - a pathogen is often found in it; quarantine measures if a child with a disease is detected in a children's group.