General information
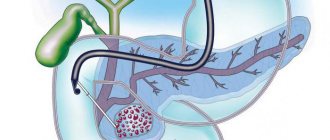
Poliomyelitis is a highly infectious viral disease primarily affecting young children and is caused by one of three serotypes of poliovirus (1,2 or 3). It affects the nervous system and can lead to general paralysis in a matter of hours. The virus is transmitted from person to person primarily through the fecal-oral route or, less commonly, through some common carrier of infection (for example, contaminated water or food) and multiplies in the intestines. Many infected people have no symptoms but shed the virus in their feces and can thus transmit the infection to others.
Prevention of polio
The main preventive measure is vaccination of children, which is carried out at an early age and then again. There is a special vaccination calendar, on the basis of which pediatricians recommend undergoing this procedure. When vaccinated correctly, lifelong immunity and resistance to poliovirus are developed.
If we talk about the prevention of polio at the household level, it means:
- refusal to swim in dirty bodies of water that are not suitable for this;
- compliance with personal hygiene rules;
- refusal of potentially dangerous products. In this sense, raw milk is undesirable - a pathogen is often found in it;
- Quarantine measures if a child with a disease is detected in a children's group. At the same time, all objects and things are processed and disinfected.
Now polio is quite rare - this is due to centralized vaccination, thanks to which children from an early age develop immunity to the polio virus, and therefore calmly tolerate contact with it.
Chance of getting sick
Polio mainly affects children under 5 years of age. The disease still exists, although WHO estimates that since 1988, the number of polio cases has decreased by more than 99%, or from 350,000 to 359 cases reported in 2014 and further in 2015 to 73 cases. In 1988, the number of countries experiencing transmission of wild poliovirus (WPV) exceeded 125, in 2014 there were only 9, and in 2015 only 2 countries reported cases of polio caused by WPV (Afghanistan and Pakistan).
But as long as there is at least one infected child in the world, children in all countries are at risk of contracting polio.
Questions and answers on the topic of polio
Is it necessary to get the OPV vaccine?
Parents have the opportunity to refuse such vaccination - they can write a written refusal and not undergo this procedure. However, doctors warn against such a decision: remember that if 10% of children get sick, the consequences will be irreversible, and for some children such a refusal will cost their lives. Currently, OPV vaccination is the only way to be 100% protected against the polio pathogen.
How is the polio vaccine given?
The vaccination is done twice, starting from the age of three months. The injection is given intramuscularly and contains the virus killed by formaldehyde.
How effective is vaccination against this disease?
Since the active fight against polio (1988), thanks to vaccination, it has been possible to reduce the number of cases from 350 thousand people per year to 359 cases (in 2014). These data speak for themselves: after receiving the vaccine, the disease becomes harmless and no longer threatens the person.
Symptoms and nature of the disease
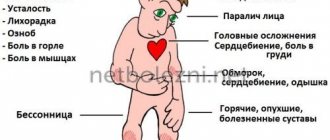
The incubation period is usually 7-10 days (ranges from 4 to 35 days). The first symptoms are fever, fatigue, headache, vomiting and pain in the limbs.
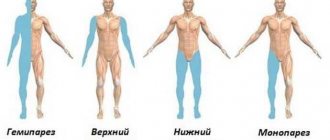
Complications after an illness
Acute flaccid paralysis (usually of the legs) develops in one in 200 cases of infection. Persistent, irreversible paralysis and resulting deformities of the lower extremities are a common consequence of the disease.
Poliomyelitis is also dangerous due to other complications: pneumonia, pulmonary atelectasis, interstitial myocarditis; Sometimes acute dilation of the stomach and severe gastrointestinal disorders with bleeding, ulcers, and perforation develop.
Academician Zverev discovered a sevenfold increase in antibodies after caring for a patient
Virologists answered the most pressing questions about revaccination and antibodies
The mandatory requirement for everyone to be vaccinated and revaccinated against coronavirus is increasingly dividing people. Happy holders of the coveted vaccination certificate boast online that they were allowed to eat in public catering... Opponents of vaccination, especially those for whom doctors do not recommend vaccination against coronavirus, ignore the “threats” of the authorities, and regarding the ban on visiting cafes and restaurants, they respond invisibly to the restrictors of freedom: “I’ve never really gone to restaurants—and now I’ll get by.”
There is another group of citizens for whom vaccinations, according to scientists, may be contraindicated for a long time. These are people who have recovered (including asymptomatic people) whose antibodies are still strong. We decided to talk about all the fears and doubts of those who have not been vaccinated with the capital’s virologists.
So, we remind readers that from June 28, all public catering outlets were closed to all Muscovites who had not been vaccinated by order of Mayor Sergei Sobyanin. Many of them closed completely after this order.
According to Russian Health Minister Mikhail Murashko, even those who have already been vaccinated once should be revaccinated to enhance the effect. For now, this should be done once every six months, but in the future, when the number of diseases decreases, repeat vaccinations can be done once a year.
Citizens who asked a logical question about existing antibodies received a clear answer: they should not test IgG immunoglobulins (their presence, in principle, should indicate the presence of immunity to the SARS-CoV-2 coronavirus). This is where we started our conversation with experts.
Should coronavirus antibodies be tested before vaccination?
Theoretically, antibodies are an indirect sign that a person still has protection and could be given some relief from going for a vaccination, scientists argue. But... the problem is that until doctors have developed requirements for recording antibodies, there is no agreement on where the immunoglobulin line should be, after which vaccination will be considered optional.
“For now, a high titer of antibodies is an abstraction,” comments a specialist from the City Clinical Hospital named after. Pirogov. - Why? The titers of different test systems are not comparable: in some, the reference (normal) values start from 1300, in others - from 1.1. In other words, some measure in boas, others in monkeys, others in baby elephants, etc. There are now about a hundred such systems for measuring antibodies of different sizes on the market, from different manufacturers. It is very difficult to bring them to some common denominator. The regulator, that is, the Ministry of Health, must compare all these hundred tests and identify the threshold after which all clients who apply can feel safe. This is ideal, but it is still very far away; this work is very labor-intensive. Therefore, during a pandemic, when the incidence is growing, it is easier to simply vaccinate everyone again. Even if your antibody titer is high, additional administration of a vaccine (any of those registered in our country) will not make you worse. Everyone is afraid of a cytokine storm... But it only happens against the background of a real infection - it shouldn’t happen with a vaccine.
Why is it safe to get vaccinated again?
“The recommendation to be vaccinated or revaccinated with a vaccine, even if it is the same Sputnik-V or Sputnik-Light again, does not pose any danger,” says the head of the department of the Institute of Molecular Biology. Engelhardt, Pyotr Chumakov. – After about six months, the number of antibodies in those who have been vaccinated decreases, and therefore additional vaccination will only enhance protection and will lead to the emergence of so-called superantibodies. Yes, side effects from the introduction of the vaccine, unfortunately, occur in weakened people, but the developers never promised a hundred percent result, but only 90 percent effectiveness.
Petr Chumakov once again explained to our readers the essence of vector vaccine technology. When creating Sputnik-V, a live adenovirus is used, or rather, not the adenovirus itself, but one of its particles, which carries information about the S-protein of the coronavirus. The particle enters the cell and begins to synthesize S-protein, which eventually appears on the cell surface. But it itself does not reproduce (it does not have products for replication). The immune system of the vaccinated person “notices” the foreign S-protein and begins to produce antibodies. The cell, which played the role of an “incubator” for the coronavirus protein, soon disappears irrevocably along with the S-spike.
“Genetic changes in the body after the introduction of such a vaccine are impossible,” explains Chumakov. – This technology has been tested for decades and, by the way, it should theoretically have much fewer side effects than inactivated vaccines precisely due to the fact that a live virus is used here and a small amount of foreign protein is introduced.
Should those who have been ill wait to get vaccinated?
Molecular biologist Petr Chumakov believes that vaccination after an illness can be waited for six months or even more:
– I think that those who have recovered from COVID-19 are not seriously threatened even after a year - their bodies have a memory of this disease, no worse than the bodies of those vaccinated. Even if such people become infected again, they will most likely experience the disease asymptomatically, or at most like a cold. And at the same time, by the way, they will acquire even stronger immunity, which can then last for a lifetime.
And here is the special opinion on this matter of virologist, head of the department of Sechenov University, academician of the Russian Academy of Sciences Vitaly Zverev:
– People who have already received the vaccine or, moreover, have been ill, do not need to do anything. Everyone seems to have forgotten the name of this virus. In its name, “SARS” comes first. Its epidemic occurred in 2003. Immunity against this virus is still preserved in those who were ill and survived SARS. That is, 17 years have already passed! Most likely, the new coronavirus will have the same long-lasting immunity, because they are very similar in antigenic structure.
Therefore, I think that those who have been ill have immunity, and it is they who mainly create that valuable collective immunity that everyone is talking about.
Moreover, we are talking about both those who have been seriously ill and those who have had mild COVID-19. There is not a single vaccine that provides stronger, longer-lasting immunity than previous illness. I can refer to my own experience. I had coronavirus, and after about a year the antibodies were no longer detectable in my blood. But after I had to care for a “Covid” patient, I did not become infected, and after checking my antibodies, I was convinced that they “grew” again 7(!) times. If all those who recovered from the disease were re-infected, we would already have millions, not thousands of new patients. But this doesn’t happen. So I urge you to take care of those who have had COVID-19. This is our gold fund.
Photo: pixabay.com
Link to publication: mk.ru/
Effectiveness of vaccination
In 1988, governments created the Global Polio Eradication Initiative (GPEI) to rid humanity of the disease forever. Following widespread use of the polio vaccine, the incidence of the disease fell sharply in many industrialized countries. Since 1988, the number of polio cases has decreased by more than 99%, from 350,000 to 73 cases reported in 2015, according to WHO.
Just 20 years ago, polio caused paralysis in 1,000 children every day. In 2010, 1,349 children were paralyzed. This decrease was the result of global efforts to eradicate the disease. In fact, this is the largest peacetime mobilization of people in history.
In 2014, only three countries in the world (Afghanistan, Nigeria and Pakistan) remained endemic for polio; in 2015, Nigeria was removed from this list, while in 1988 the number of such countries exceeded 125. Failure to eradicate polio in these remaining persistent foci could result in up to 200,000 new cases of the disease occurring annually worldwide within 10 years. The world can be freed from the threat of polio if everyone commits to it - from parents to government workers and from political leaders to the international community.
Frequently asked questions about polio
Credits : World Health Organization
What is polio?
Poliomyelitis is a highly contagious disease caused by the poliovirus. It attacks the nervous system and can cause paralysis or even death in just a few hours.
How is polio transmitted?
Wild poliovirus (WPV) enters the body through the mouth through water or food that has been contaminated with feces from an infected person. The virus multiplies in the intestines and is shed in the feces of an infected person, through which it can be transmitted to other people.
What are the symptoms of polio?
The initial symptoms of polio are:
- heat
- fatigue
- headache
- vomit
- neck stiffness
- pain in the limbs.
Who is at risk of contracting polio?
Polio mainly affects children under 5 years of age.
What are the consequences of polio?
Poliomyelitis causes the following consequences:
- One in every 200 people infected with polio will experience permanent paralysis (usually in the legs).
- Of those paralyzed, 5% to 10% die from respiratory muscle paralysis caused by the virus.
Is there a cure for polio?
No, there is no cure for polio. Polio can only be prevented through immunization. There is a safe and effective polio vaccine, oral polio vaccine (OPV). OPV provides essential protection for children against polio. If used repeatedly, it protects the child for life.
Global fight against polio
What is the Global Polio Initiative?
In 1988, governments created the Global Polio Eradication Initiative (GPEI) to rid humanity of the disease forever. The initiative is a global partnership involving national governments, WHO, Rotary International, the US Centers for Disease Control and UNICEF. Since the creation of the GPEI, the number of polio cases worldwide has decreased by more than 99%. Just 20 years ago, polio caused paralysis in 1,000 children every day. In 2010, 1,349 children were paralyzed.
Where is wild poliovirus still circulating today?
Polio transmission has never stopped in 3 countries - Afghanistan, Nigeria and Pakistan. However, polio can and does spread from these countries to neighboring and more distant countries. It must be remembered that the emergence of polio anywhere is a threat to children throughout the world. He has no regard for boundaries or social status and moves easily.
Can polio spread to other polio-free countries?
Polio does not respect borders: any unvaccinated child is at risk. For every case of paralysis, between 200 and 1,000 children become infected asymptomatically. Therefore, identifying polio is difficult, as is preventing its movement. Children living in areas where immunity levels are low are especially vulnerable. The best defense against imported polio is eradication of the virus. Only in this case will all children be safe.
What needs to be done to eradicate polio?
To stop polio we must:
- engage the entire community in efforts to reach every child left behind;
- develop special plans to reach children from mobile, migrant, conflict zones or remote areas;
- strengthen routine immunization, which is the nation's best defense against polio;
- improve surveillance in high-risk areas;
- encourage governments to reach the poorest people with other public services;
- continue to have the highest level of political commitment from national governments and multilateral institutions;
- close the funding gap - US$590 million is still required to fund activities in 2011-2012;
- make a donation.
Why is so much attention paid to polio and not to other diseases?
Polio is one of the few diseases that can be completely eradicated, as was the case with smallpox. By eradicating polio, we will benefit children around the world, and no child will ever have to suffer the pain of paralysis caused by polio. Most diseases, such as HIV and malaria, cannot be eradicated because the ability to do so does not yet exist. Polio does not have a direct host (i.e. it does not affect animals, and its virus cannot exist in animals, in the same way that malaria exists in mosquitoes, for example); There is a safe and effective vaccine to protect children from polio; it does not survive for long periods of time in the environment and although it is contagious, its infectious period is relatively short. Polio eradication efforts are also helping to strengthen routine health care. Polio eradication efforts have created an active polio surveillance network in all countries, which is now integrating other diseases, including measles. Polio eradication infrastructure is also used to provide other health services, such as the distribution of deworming tablets, vitamin A and mosquito nets.
Oral polio vaccine (OPV)
Why are children given oral polio vaccine?
The polio vaccine is the only means of protection against polio, a paralyzing disease for which there is no cure. It is important to ensure that every child under 5 years of age is immunized against polio. The oral polio vaccine is safe and effective, and because it is administered orally, it can be given by volunteers.
Are there any side effects of the oral polio vaccine?
Oral polio vaccine (OPV) is one of the safest vaccines ever created. It is so safe that it can be given to sick children and newborns. It is used worldwide to protect children from polio and has saved at least 5 million children from permanent paralysis caused by polio. In extremely rare cases, the attenuated virus in the oral polio vaccine may mutate and become virulent again. The risk of getting polio for children is much higher than the risk of side effects from using the polio vaccine.
What are the teachings of Islam regarding the polio vaccine?
Oral polio vaccine (OPV) is safe and has been declared halal by Islamic leaders around the world - Grand Sheikh Tantawi of Al-Azhar University, the Grand Mufti of Saudi Arabia and the Indonesian Ulema Council.
Is it safe to give multiple doses of OPV to children?
Yes, it is safe to give children repeated doses of polio vaccine. This vaccine is intended to be given multiple times to provide complete protection. In tropical regions, several doses of polio vaccine, sometimes more than 10, must be used to ensure complete protection for a child. This vaccine is safe for all children. Each additional dose further strengthens the child's immunity against polio.
How many doses of OPV does a child need to provide protection?
The oral vaccine must be given several times to be fully effective. The number of doses needed to immunize a child depends entirely on the child's health and nutritional status and the number of other viruses to which he has been exposed. Until a child is fully immunized, he or she is at risk of contracting polio. This highlights the need to immunize all children during each round of national immunization days. The polio virus can be hidden in the body of every unvaccinated child.
Should a child be given OPV during polio campaigns and routine immunization?
Yes. Oral polio vaccine (OPV) is safe and effective, and each additional dose means the child receives additional protection against polio. Multiple doses of OPV are required to achieve complete immunity against polio. If the child has received the vaccine previously, additional doses received during national or subnational immunization days will provide valuable additional immunity against polio.
Is OPV safe for sick children and newborns?
Yes. Oral polio vaccine is safe for sick children. In fact, it is extremely important to vaccinate sick children and newborns in campaigns because their level of immunity is lower than that of other children. All sick children and newborns should be vaccinated in upcoming campaigns to give them the protection they need from polio.
Why do some industrialized countries use a different polio vaccine than developing countries?
All but two countries in the world (Sweden and Iceland) used oral polio vaccine (OPV) to eradicate polio and continued to use OPV generally until the late 1990s, when some switched to inactivated polio vaccine due to progress made towards the eventual eradication of polio. (when the risk of wild poliovirus has decreased). Most countries use OPV because it has the unique ability to induce local gut immunity, meaning it can interrupt transmission of wild poliovirus in the natural environment. This is not possible with IPV, an inactivated polio vaccine that stimulates only a very low level of immunity against poliovirus in the intestine, resulting in individual protection against polio, but, unlike OPV, cannot prevent the spread of wild poliovirus.
Source
published 11/02/2015 09:48 updated 23/10/2015 — Vaccination, Infectious diseases, Vaccination, Infectious diseases, WHO materials
Vaccines
There are two types of vaccines to prevent polio—live oral polio vaccine (OPV) and inactivated polio vaccine (IPV). OPV provides essential protection for children against polio. If used repeatedly, it protects the child for life. All available evidence indicates that OPV is not teratogenic and is safe for pregnant women and HIV-infected individuals. However, rare serious adverse events associated with OPV may include vaccine-associated paralytic polio (VAPP) among vaccinated individuals and their contacts, and the emergence of vaccine-derived polioviruses (VDPV). The incidence of VAPP is estimated to be 2–4 cases per million births per year in countries using OPV. The introduction of at least one dose of IPV before OPV vaccination leads to the elimination of VAPP. Let us remind you that in the National Calendar of Preventive Vaccinations of the Russian Federation, the first two (!) vaccinations against polio are given with inactivated polio vaccine!
IPV is considered a highly safe vaccine whether given alone or in combination with other vaccines. There is no evidence of a cause-and-effect relationship with adverse events other than mild local erythema (0.5-1%), tissue induration (3-11%), and tenderness (14-29%).
More about vaccines
Historical information and interesting facts
Expert opinion
CM. Harit
Professor, Doctor of Medical Sciences, Head of the Department of Prevention of Infectious Diseases of the Research Institute of Children's Infections
In Europe and the USA and Japan and Australia and other countries, vaccinations are given with a killed polio vaccine, in our country the child receives the first 2 vaccinations with the same killed vaccine and only the subsequent ones with a live one...
Scientific research on polio dates back to the work of the German orthopedist J. Heine (1840), the Russian neurologist A. Ya. Kozhevnikov (1883) and the Swedish pediatrician O. Medina (1890), who showed the independence and contagiousness of this disease.
Iron Lung apparatus, circa 1950
Before the polio vaccine was invented, patients were placed in an iron lung machine that stimulated breathing. It was he who served as the prototype of modern anesthesia machines and devices for artificial ventilation of the lungs.
On April 112, 1955, a large-scale study was successfully completed in the United States, confirming the effectiveness of the Jonas Salk vaccine, the first vaccine against polio. The importance of this event cannot be overestimated. In 1954, more than 38 thousand cases of polio were reported in the United States, and after 10 years of the use of the Salk vaccine, in 1965, the number of cases of polio in the United States was only 61.
All over the world, attenuated (weakened) strains obtained by Dr. Sabin - serotypes 1, 2 and 3 - are used for the production of live polio vaccines.
3 serotypes. No indigenous wild poliovirus type 2 has been detected in the world since 1999. 26-31% of VAPP cases are associated with vaccine virus 2, which is a component of trivalent OPV. It has therefore become critical to move from the use of trivalent OPV (containing virus serotypes 1,2 and 3) to bivalent OPV (containing only serotypes 1 and 3) in national immunization programs and to coordinate this transition internationally. In 2015, the World Health Assembly agreed that all WHO Member States currently using OPV should prepare for a global phaseout of the type 2 poliovirus component of OPV. In April 2021, all stocks of trivalent OPV were seized and destroyed from all service delivery points, and their seizure was confirmed by WHO.
Is a child contagious after polio vaccination?
Poliomyelitis is a dangerous viral infection that, when infected, puts the health of a child or adult at risk. Therefore, the vaccine against the disease is included in the National Vaccination Calendar.
Parents are wondering whether it is possible to become infected with polio from a vaccinated child. Fear is associated with the introduction of a weakened but living strain of the pathogen to the patient.
What types of vaccines are used?
There are 2 types of vaccinations, which are selected by the therapist after a general examination and laboratory tests:
- Alive . Used since 1960, contains an active strain of 3 types of pathogens. They are weakened by growing in unsuitable conditions. The virus is alive, but does not cause infection. The vaccine is administered orally because the disease spreads into the human body through the mouth. Humoral cellular immunity is formed. There is a small risk that the infection will worsen when conditions are favorable, which may lead to infection.
- Not alive . Pathogenic microorganisms are completely inactivated. This is done using formaldehyde. The injection is done subcutaneously, intramuscularly. Only humoral immunity is formed. The disadvantage is the lack of protection of the digestive tract: the risk of disease increases even with immunization.
To produce any of these types, 3 strains of pathogens are used.
If a person has been ill with one of these viruses, but has not been vaccinated, re-infection with the other two varieties is possible. Therefore, it is recommended to get vaccinated even in case of illness.
Features of the live vaccine
The vaccine is created in such a way that when it enters the digestive tract, it simulates infection . Therefore, the immune system is unable to distinguish between the spread of a real viral agent and a vaccine.
The microflora of the gastrointestinal tract is optimal for reproduction and spread of infection.
If a person's immune system is weakened, insufficient antibodies are produced. Therefore, the virus has the opportunity to reproduce. It spreads through the mucous membrane, penetrating the bloodstream.
An infection can occur that is dangerous to the life and health of the patient, which is why many countries refuse this method of vaccination.
In Russia, the drug is used everywhere, but each patient has a choice: take the drug with activated strains orally or get a subcutaneous vaccination.
In the latter case, there is no risk at all, since the pathogen is destroyed. Only the antigenic composition remained in the drug.
Is a child contagious after vaccination?
Parents of unvaccinated children worry about spreading the disease. They ask pediatricians whether a child can become infected after vaccination. If a patient is given an inactivated vaccine subcutaneously or intramuscularly, there is no risk of infection.
When using a live vaccine, the patient is at risk of developing the disease. But this happens very rarely.
The process can begin after the first injection. If re-vaccination has been carried out, the risk is reduced. During the third procedure it is absent.
Infection by injection of the drug is possible in patients with the following diseases or conditions:
- congenital or acquired immunodeficiency;
- infants with abnormalities in the development of the immune system;
- pregnant women.
Any child who has been vaccinated orally with active microorganisms should not attend educational institutions for 60 days.
Once infected, polio can be transmitted to other people in the following ways:
- water;
- food;
- contact-household.
This type of infection resolves without complications. With the right treatment, the disease goes away quickly and in a milder form.
Therapy is prohibited without consulting a doctor. It is prescribed only when laboratory tests are completed and the diagnosis is confirmed.
How many days after vaccination with a live vaccine can a child be infectious?
The incubation period after administration of the drug is 2 months. During this time, the child is limited in his access to communication with other children or adults.
This is especially true for those who have not previously been vaccinated.
Even if the patient does not have obvious signs of infection from the drug, there is a risk of an asymptomatic form of the disease. It is unknown whether it is contagious when the live strain is administered.
After passing the incubation period, you need to re-visit the pediatrician, who gives permission to visit educational institutions.
Have there been cases of polio infection from a vaccinated child?
No such cases were identified. However, doctors do not exclude the risk of spreading a dangerous, highly contagious infection, which can be transmitted through household items, dirty dishes, and shared food.
No outbreaks of the disease have been reported in any kindergarten, school or university. This is especially true for groups that recruit children who have completed all the necessary vaccinations.
An unvaccinated child has contact with a vaccinated person: what are the consequences?
This form of infection is possible if the immunity of an unvaccinated baby is weak. In this case, the child is at risk, and after contact you need to monitor him.
Special treatment measures cannot be carried out, since infection is possible only in rare cases.
It is recommended that you see a doctor for testing if you experience 1 of the following symptoms:
- increased body temperature;
- pain in the throat, head;
- sudden loss of strength, malaise, weakness;
- frequent vomiting for no reason;
- muscle stiffness;
- signs of meningitis.
The pediatrician conducts a general examination. Infection is indicated by reduced muscle functionality, difficulty swallowing and breathing reflexes.
If a disease is suspected, laboratory tests are prescribed. To do this, they take a swab from the nasopharynx, feces, and cerebrospinal fluid. This is due to the fact that the pathogen spreads throughout the gastrointestinal tract and nervous system. Conduct virological testing, for example, PCR. The antigenic composition of polio is determined.
If the test detects polio antigens, comprehensive treatment is prescribed. Bed rest, painkillers, artificial ventilation, therapeutic exercises, physiotherapy, and diet are prescribed .
Parents should remember that without obvious signs of illness there is no need to worry. Self-medication is prohibited.
Conclusion
In the fight against polio in the twentieth century, a vaccine was developed that is still effective today.
Weakened children are prescribed only vaccination using an inactivated strain. The drug is safe, but does not guarantee one hundred percent protection after contact with an infected person.