The meningitis vaccine can save a person from this serious and dangerous disease. Meningitis 50 years ago was considered an incurable pathology. Today, forecasts depend on the timeliness of the patient seeking professional medical help, as well as on the qualifications of the doctors themselves. At the Yusupov Hospital, leading neurologists and infectious disease specialists in Russia are treating meningitis. In the hospital, at any convenient time, you can consult with doctors regarding all the pros and cons of vaccination.
The meningitis vaccine is actually capable of protecting the human body from a rapidly occurring dangerous inflammatory disease, which also entails serious complications. In the absence of adequate treatment, meningitis can take the life of a patient within 24 hours.
The main objective of vaccinations against meningitis is to develop a protective mechanism against the causative agents of the disease - meningococcus, pneumococcus and Haemophilus influenzae. In many developed countries, such as Great Britain, France, Germany, the USA, etc., vaccinations against meningitis are included in the national vaccination calendar.
In order to draw the public's attention to the dangers of meningitis, as well as to raise people's awareness regarding the characteristics of meningitis, its symptoms, routes of infection, treatment and prevention, World Meningitis Day was declared on April 24.
Vaccine options
There are three types of vaccines available to combat this disease.
- Polysaccharide vaccines have been available to prevent meningococcal disease for more than 30 years. Meningococcal polysaccharide vaccines designed to combat the disease are bivalent (groups A and C), trivalent (groups A, C and W) or quadrivalent (groups A, C, Y and W135).
- It is impossible to develop polysaccharide vaccines against group B bacteria due to antigenic mimicry with polysaccharides in human neurological tissues. Therefore, group B vaccines, used in particular in Cuba, New Zealand and Norway, were outer membrane protein (OMP) and were intended to combat epidemics caused by specific strains. Other universal group B protein vaccines are in the final stages of development.
- Meningococcal group C conjugate vaccines have been available and widely used since 1999. Since 2005, quadrivalent group A, C, Y, and W135 conjugate vaccines have been licensed for use in children and adults in Europe, Canada, and the United States. The new group A meningococcal conjugate vaccine, introduced in 2010, has a number of advantages over existing polysaccharide vaccines: it produces a stronger and more durable immune response to group A meningococcus; reduces the carriage of bacteria in the throat. It is expected to provide long-lasting protection not only to vaccinated people, but also to family members and others who would otherwise be exposed to meningitis. The vaccine is available at a lower cost than other meningococcal vaccines; it is expected to be particularly effective in protecting children under two years of age who do not respond to conventional polysaccharide vaccines.
The following names of vaccines are used: polysaccharide - meningococcal group A vaccine, polysaccharide dry, polysaccharide meningococcal vaccine A+C, Meningo A+C, Mencevax ACWY and Menugate (conjugated tetravalent, against ACWY serotypes) and Menactra (conjugated tetravalent, against ACWY serotypes).
Vaccination is especially indicated for the following groups at high risk of meningococcal disease:
- persons who had direct contact with patients infected with meningococci of serogroups A, C, Y or W-135 (in the family or in closed institutions);
- persons with deficiency of properdin and complement components;
- persons with functional or anatomical asplenia;
- persons with cochlear implants;
- tourists and persons traveling to hyperendemic areas for meningococcal disease, such as sub-Saharan Africa;
- employees of research, industrial and clinical laboratories who are regularly exposed to N. meningitidis in aerosol-forming solutions;
- students of various universities, and especially those living in dormitories or apartment-type hotels;
- conscripts and new recruits.
It should be added that the European Commission has currently approved the drug Bexsero, produced by the Swiss pharmaceutical company Novartis, intended to protect patients of all age groups, including children over two months, from meningococcal infection serogroup B.
Vaccine preparations
The drugs used for vaccination help cope with pathogens of half groups A, C, W-135, Y. List of the names of vaccines of this type against meningitis, approved by WHO:
- Minengo A (French production). The drug helps prevent cerebrospinal meningitis. It can be done for children over 1.5 years old;
- Menactra (American made). This subtype helps the immune system resist pathogens. Can be given to children aged two years and older;
- Mencevax (Belgium). The medicine reduces the risk of meningococcal infection.
If we talk about the vaccine against Haemophilus influenzae, then ACT-HIB is used here. It is based on particles of the cell wall of the pathogen. The drug is available in the form of a dry powder. Before introducing it, it is customary to add a solvent. The vaccine is given in the shoulder or thigh.
Vaccines are used against pneumococcal meningitis under the names:
- Pneumo 23 (children from two years old);
- Prevenar 13. Can be used for children from two months to five years. Four injections are enough to provide lifelong protection.
Principles and purposes of vaccination
Meningococcal disease is potentially fatal and should always be treated as a medical emergency. Meningococcal meningitis occurs in small clusters worldwide, with seasonal variations and a varying percentage of epidemic bacterial meningitis cases.
Meningococcal meningitis is a bacterial form of meningitis, a serious infection that affects the lining of the brain. It can cause severe brain damage and, if left untreated, is fatal in 50% of cases. But even when diagnosed early and treated properly, up to 16% of patients die, usually within 24 to 48 hours of symptoms appearing.
It is important to remember that there are endemic areas of meningococcal infection in the world, the so-called meningitis belt of Africa (sub-Saharan Africa, stretching from Senegal in the west to Ethiopia and Egypt in the east). High incidence is observed in Canada, with outbreaks occurring in France and the USA. Students of closed educational institutions and colleges are especially vulnerable.
How great is the risk of getting sick?
Approximately 10-20% of people are carriers of meningoccal infection. Not all of them are sick - the carrier himself may be healthy. The bacteria live in the nasopharynx and are transmitted by airborne droplets. The sick person is contagious for about 3 weeks, of which 1 week is the incubation period, when the disease does not manifest itself in any way. You cannot get infected from animals or objects.
“We are riding the wave of a rise in meningococcal meningitis.”
The infectiousness of this infection is quite low. However, the incidence of meningococcal disease has a wave-like nature, and 2021 appears to have seen a surge in incidence. For example, V.S. Kovalev, a pediatrician at the Children's Research and Clinical Center for Infectious Diseases of the FMBA in St. Petersburg, in an interview given in February 2021 to the website miloserdie.ru, notes that such rises occur approximately once every 20-25 years, and now Russia is on the rise.
“A large number of people in Russia have already fallen ill with meningitis”
The Business Information Agency of Khakassia cites data from Rospotrebnadzor, according to which the epidemiological threshold for meningococcal infection was exceeded back in March 2021:
According to Rospotrebnadzor, in the first six months of this year, 549 Russian residents fell ill with meningococcal infection. This is 23% more than in the same period last year.
Vaccine effectiveness
Vaccination is carried out once, the effectiveness is about 90%, immunity is formed on average within 5 days and lasts 3-5 years. In December 2010, a new meningococcal group A conjugate vaccine was introduced throughout Burkina Faso and parts of Mali and Niger, where a total of 20 million people aged 1–29 years were vaccinated. Subsequently, in 2011, these countries reported the lowest ever number of confirmed cases of meningitis A during the epidemic season. Immunization with polysaccharide vaccines leads to a rapid rise in antibodies, which persist in children for at least 2 years, and in adults - up to 10 years; revaccination is carried out every 3 years. Conjugate vaccines maintain immunity for 10 years and develop immunological memory.
WHO recommends polysaccharide vaccines A and C for persons over 2 years of age from risk groups, as well as for mass vaccination during an epidemic - both for individual protection and to create collective immunity and reduce carriage. A type C conjugate vaccine has been created and used in Europe, which has led to a sharp decrease in the incidence of meningitis C; England, Holland and Spain have included this vaccine in their calendars.
The effectiveness of meningococcal vaccine was also assessed in post-registration studies. Thus, in the fight against an outbreak of meningococcal infection in the United States, 36 thousand people aged 2 to 29 years were vaccinated. As a result of the case-control study, 85% effectiveness was revealed, and among children from 2 to 5 years old it was 93%.
What can be done to reduce the risk of complications after vaccination?
Before vaccination, the child must be examined and examined by a doctor. Even during pregnancy, the fetus is examined using various methods for diseases and developmental abnormalities. The mother must clearly undergo all examinations suggested by the doctor during pregnancy. Before vaccination, children in the maternity hospital are examined by a neonatologist. If suspicious conditions are detected, vaccination is not carried out, and additional examinations are prescribed. Only after them, in the absence of contraindications, the child can be vaccinated. In addition, the maternity hospital screens all newborns for the most common genetic abnormalities. Parents should not refuse to undergo the examination.
Vaccinations in the clinic are carried out only after a doctor’s examination and temperature measurement. The mother can pre-measure the baby’s temperature at home before coming to the clinic. If there is a suspicion that the child is not healthy, it makes sense to postpone the vaccination for several days and observe the child. Children who are not regularly observed by a pediatrician should be examined before vaccination (general urine and blood tests). In children with chronic diseases, you need to make sure that there is remission. They are usually examined by specialized specialists and, if necessary, examined. You should not completely refuse vaccinations in children with severe chronic diseases. You need to create an individual calendar for them. Such children have a high risk of complications from infectious diseases. Children with allergic diseases should try to avoid contact with the allergen before vaccination.
Online consultation with pediatrician Olga Nikolaevna Tekutyeva
Registration online
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
Post-vaccination reactions
Vaccines against meningococcal disease are well tolerated. In 25% of vaccinated people, a post-vaccination local reaction is possible in the form of soreness and redness of the skin at the injection site. Sometimes there is a slight increase in temperature, which normalizes after 24-36 hours. These vaccines are not required for routine immunization in our country, but you need to know about them, especially for those parents whose child is at high risk of developing meningococcal infection, or those who are planning a vacation in countries with unfavorable conditions for the spread of this infection.
When are anti-pneumococcal vaccinations against meningitis given to adults and children?
Many countries implement mandatory immunization of patients against pneumococcal infection. Since the beginning of the year, in the Russian Federation, such immunization has been included in the national vaccination calendar. Vaccination allows the body to receive the antigen in a safe minimum amount, which eliminates the possibility of a full-blown disease in the future.
In our country, vaccination is carried out using two types of serum: Pneumo-23 and Prevenar. Both of these drugs are characterized by the absence of side effects and high efficiency. The Prevenar vaccine can be administered to children over three months of age. Pneumo-23 is administered to children over 2 years of age.
When to vaccinate?
Domestic vaccines - meningococcal A, A + C - are used from 18 months, and are also administered to adolescents and adults. These drugs can also be administered to children under 18 months of age if there is a sick person in the family or depending on the epidemic situation in the region. However, this measure does not create long-term, lasting immunity, and vaccination must be repeated after 18 months. Polysaccharide vaccines "Meningo A+C" and "Mencevax ACWY" are administered to children from 2 years of age. For vaccination of children over 9 months of age, the conjugate vaccine "Menactra" can be used, in this case it is prescribed twice with an interval of at least 3 months, and after 2 years is done once. The level of protective antibodies lasts up to 10 years.
Tips and tricks
Despite the frightening list of possible adverse reactions and complications from vaccines, the main thing to remember is that severe consequences are extremely rare and they know how to deal with them, and local and general reactions are not so frequent, mild and not dangerous to health.
However, for several days or weeks after vaccination (how long depends on the specific vaccine), you should carefully monitor your child's well-being:
- High fever for 3 or more days, shortness of breath, convulsions, frequent vomiting, severe headache and other noticeable and persistent deviations from normal health are a reason to call a doctor.
- The administration of a vaccine is always an additional burden on the body, sometimes quite significant, so in the first days after vaccination you should rest more and avoid noticeable physical and emotional stress.
- When the temperature rises above 38°, antipyretic drugs are used in combination with physical methods - cold compresses, wiping with a damp sponge. It is especially important to reduce the temperature in children prone to seizures and with hypertensive-hydrocephalic syndrome.
- Carefully monitor the condition of the body if a vaccinated child, especially a child, has a high risk of allergic reactions.
- During the first 2 weeks before and after vaccination, it is better to avoid foods that are obligate allergens: seafood, honey and chocolate, eggs, strawberries, raspberries, citrus fruits.
- In the first 7-10 days, try to avoid contact with other people to reduce the risk of colds. This is especially true for people with reduced immunity and chronic diseases.
- It is recommended to do a general urine test 3 to 4 weeks after vaccination to identify possible kidney complications: this is especially important for children with diseases of the urinary organs. The analysis will also allow timely detection of deviations and take the necessary measures.
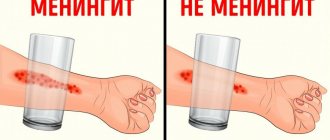
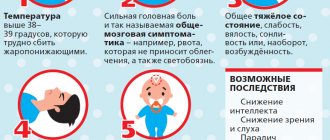
SYMPTOMS AND DANGERS OF THE DISEASE
The first symptoms of meningitis are similar to the common cold, which complicates diagnosis. An infectious disease leads to an increase in body temperature, the development of a severe headache, vomiting and nausea. In some cases, a hemorrhagic rash appears on the skin. The danger of meningitis lies in the possibility of developing cerebral edema and secondary encephalitis (infection of brain tissue). As a result, meningoencephalitis develops, which is characterized by severe neurological symptoms. It persists for a long time after recovery and often becomes a cause of disability for the patient. However, the greatest danger is posed by a brain abscess, which occurs as a consequence of secondary bacterial meningitis against the background of pathologies of the ENT organs (sinusitis, otitis media, sinusitis). The pathology provokes the development of cerebral edema and displacement of the midline structures. Therefore, patients need not only drug treatment, but also surgical intervention.