general characteristics
The brain is the main organ of the nervous system. Doctors are still studying it. The adult human brain contains 90-95 billion neurons. The cell bodies of neurons form the gray matter of the brain, and the nerve fibers (neuron processes) form the white matter.
Rice. 1. Sections of the brain.
This organ has the following types of membranes:
- soft or vascular;
- arachnoid (cerebrospinal fluid - cerebrospinal fluid - circulates between the arachnoid and soft membrane, which serves as a kind of shock absorber and protects against shock, and also supports trophic and metabolic processes between the blood and the brain);
- hard.
The brains of men and women differ in their mass. In representatives of the stronger sex, its weight is 100-150 g more. However, mental development does not depend in any way on this indicator.
The functions of generator and impulse transmission are performed by neurons. Inside the brain there are ventricles (cavities) in which cerebrospinal fluid is formed. Paired cranial nerves extend from the brain to different parts of the human body. There are a total of 12 such pairs in the body.
Structure
The main organ of the nervous system consists of three parts:
TOP 4 articles
who are reading along with this
Spinal cord: structure and functions
Speech
Spinal cord: structure and functions
Memory
- two forebrain hemispheres;
- trunk;
- cerebellum.
It also has five departments:
- terminal or anterior, constituting 80% of the mass;
- intermediate;
- average;
- posterior, which includes the pons and cerebellum;
- oblong.
The white matter of the cerebral hemispheres of the forebrain is presented in the form of nerve fibers, which can be of three types:
- association – connect cortical areas in one hemisphere;
- commissural - connects the two hemispheres;
- projection – connect the cortex with the underlying formations.
Gray matter consists of neuron bodies; in the cerebral hemispheres, this substance forms the cortex and subcortical nuclei.
Rice. 2. Lobes of the cerebral cortex.
The following table will help you understand in more detail the structure and functions of various parts of the brain:
results
At the stage of neurophysiological mapping, the results obtained were compared with the MRI picture of the representation of functional zones, synchronized at the navigation station (Table 2).
Table 2. Results of direct electrical stimulation of the cortex in the FZZ area and white matter near the pyramidal tract
When comparing the mapping results with fMRI and tractography data, in 12 (18%) patients a wider representation of speech zones was revealed, which, in our opinion, is explained by the error in performing test tasks during fMRI and the existing preoperative neurological deficit (elements of sensory aphasia). All patients in On the 1st day after surgery, contrast-enhanced MRI control was performed (Figs. 9 and 10). Total tumor removal (100% of the tumor) was achieved in 39 (60%) patients (see Fig. 1, 9, 10), subtotal (80-95% of the tumor) - in 16 (24%), 10 (16%) patients partial removal of the tumor was performed (the tumor had invaded the internal capsule, speech centers or primary motor centers). At the time of discharge, the patients' condition on the Karnofsky scale was 80±10 points. The patient's hospital stay after surgery was 7±1 days. In 47 (72%) patients, there was no deterioration in the neurological status. In 18 (28%) patients in the early postoperative period, an increase in neurological deficit was noted in the form of an increase in paresis by 1-2 points or aggravation of speech disorders: in 11 patients the motor deficit increased by 1 point, in 7 patients the severity of aphasia increased (the group included 5 patients who did not undergo awake, and 2 patients who underwent surgery with mapping of speech zones). In 8 patients, partial regression of paresis was noted within 7 days after surgery (by an average of 1 point). When tracking the follow-up after 4 months in 18 patients in the group with increased neurological deficit, 10 of them showed regression of the neurological deficit. After 4 months, neurological deficit at the postoperative level remained in 5 patients: 3 had hemiparesis of 2-3 points, more pronounced in the arm, 3 had elements of motor aphasia, 2 had hemiparesis of 3-4 points, more pronounced in the leg. Thus, persistent neurological deficit after 4 months persisted in 8 (12%) patients, which corresponds to world literature data.
Rice. 9. Preoperative and control images: MRI of the brain, T1-weighted image with contrast, axial projection. a — preoperative image: a picture of a space-occupying formation of the left insular lobe, intensively accumulating contrast agent; b — postoperative image on the 1st day after surgery: the tumor was completely removed, there was no accumulation of contrast agent.
Rice. 10. a — preoperative images, T2-weighted image in axial projection before surgery: a volumetric formation of the left frontal lobe is determined (in the projection of Broca’s area) with pronounced perifocal edema; b — postoperative images, T-weighted image on the 1st day after radical removal of the tumor of the left frontal, insular and temporal lobes of the brain: there are no signs of residual tumor tissue.
Table “Structure and functions of the brain”
| Department | Structural features | Functions |
| End or front | It consists of two hemispheres, which are connected to each other by the corpus callosum. The surface of the hemispheres has many grooves and convolutions. | The right hemisphere is responsible for the left side of the body, and the left hemisphere is responsible for the right side. The centers for the regulation of voluntary movements, the centers of conditioned reflexes and mental functions are located here. The temporal lobe of the cerebral cortex regulates hearing, taste and smell, the occipital lobe regulates vision, the parietal lobe regulates touch; frontal – speech pronunciation. |
| Intermediate | Consists of the hypothalamus and thalamus. | The thalamus is a mediator in the transmission of stimuli to the hemispheres and helps to adequately adapt to changes in the environment. The hypothalamus regulates the functioning of metabolic processes and endocrine glands. Manages the work of the cardiovascular and digestive systems. Regulates sleep and wakefulness, manages food and drink needs. |
| Rear | It consists of the cerebellum and the pons, which is presented in the form of a white thick cushion located above the oblongata. The cerebellum is located behind the pons and has two hemispheres, the inferior and superior surfaces and the vermis. | This department provides the function of an intermediary in the transmission of impulses to higher parts of the brain. The cerebellum is responsible for coordination and precision of movements. |
| Average | Located from the anterior edge of the bridge to the optic tracts. | Responsible for hidden vision, as well as the implementation of orientation reflexes (turning the body in the direction of sound). |
| Oblong | It is a continuation of the spinal cord. | Controls balance, contains the centers of breathing, swallowing, sneezing and coughing, vomiting, cardiovascular and digestive. |
Material and methods
In the period from 2014 to 2015, in the Department of Neurosurgery No. 2 of the National Medical Center named after.
N.I. Pirogov treated 65 patients (43 (66%) men and 22 (34%) women aged 32 to 68 years) with glial tumors of the brain. During the initial neurological examination, motor deficits of varying severity were detected in 46 (71%) patients (6 patients were diagnosed with hemiparesis with a decrease in strength to 1 point, in 15 - to 2-3 points, in 25 - to 4 points). 17 (26%) patients were diagnosed with aphasia (12 of them had a combination of speech and motor disorders, 5 had isolated speech disorders). In 40 (62%) patients, tumors were localized in the frontal and temporal lobes. Isolated damage to one lobe was present in only 9 patients: insular in 4, frontal in 2, and temporal in 3. In 37 (58%) patients, the tumor affected the left hemisphere, and in 24 (36%) - the right. In 4 (6%) patients, the tumor spread to both hemispheres of the brain (Table 1).
Table 1. Localization of glial tumors in operated patients
64 patients underwent primary surgery. One patient was operated on 2 times during the observation period: initially for a tumor of the frontal, temporal and insular lobes on the left (involving Broca's area and Wernicke's area) and again 16 months later due to continued growth of the tumor. Both operations were carried out using the asleep-wake-asleep protocol. Control of the radicality of tumor removal (MRI with contrast) was performed in all patients on the 1st day after surgery (Fig. 1).
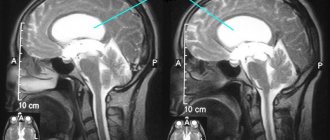
Rice. 1. Images of preoperative planning at the navigation station. MRI brain, T1-weighted image with contrast. a - frontal; b - sagittal; c — axial projection. A space-occupying formation (1) of the left temporal and parietal lobes of the brain (in the projection of the superior temporal, angular and supramarginal gyri) with fuzzy, uneven contours, with pronounced perifocal edema, intensively accumulating contrast agent is determined. Arrows indicate the motor cortex (2), pyramidal tracts (3) and speech areas (4); d — 3D model of the brain with projection of the FZ and tumor.
Along with MRI in standard modes, 50 (77%) patients underwent fMRI at the stage of preoperative diagnosis due to the presence of speech disorders in 17 patients and involvement of the internal capsule in 4 patients (in addition, the group included 9 patients who had no manifestations of aphasia , but the risk of its development after surgery was high). The fMRI technique is based on recording regional hemodynamic changes that occur when the cerebral cortex is activated in response to specific stimulation (alternating phases of rest and motor, mental or other activity). Based on the results of the examination, the relationship of the tumor with the motor pathways, Wernicke’s and Broca’s areas was established in these patients (Fig. 2 and 3).
Rice. 2. Images from the navigation station MRI of the brain, T1-weighted image with contrast, sagittal (a) and axial (b) projections: a volumetric formation is determined (1) in the right temporal and parietal lobes of the brain, with fuzzy uneven contours, with pronounced perifocal swelling, intensively accumulating contrast agent. The pyramidal tracts (2) passing anterior to the tumor are indicated; c — 3D model of the spatial relationship of the tumor (1) and pyramidal tracts.
Rice. 3. Preoperative and control images MRI of the brain, T2-weighted image, sagittal and frontal projections. Preoperative T2 (a) and Flair (b) images: a picture of a space-occupying lesion in the left frontal lobe involving the premotor area and the anterior parts of the precentral gyrus; postoperative T1 (c) and Flair (d) images on the 1st day after surgery. The tumor was completely removed.
In patients with frontotemporal tumor localization in the dominant hemisphere and proximity to speech centers, in order to reduce the risk of the appearance or increase of postoperative motor, sensory and amnestic aphasia, tumor removal was carried out with intraoperative awakening (according to the asleep-awake-asleep protocol) (16 patients). For this purpose, a team of anesthesiologists and neurosurgeons had a conversation with the patient on the eve of the operation, during which all stages of the future surgical intervention were considered. Particular attention was paid to the moment of awakening in the operating room. The anesthesiologist sought to ensure that the patient had a conscious understanding of what he would see in the operating room. It was discussed what sensations he would experience when he woke up, what the peculiarities might be when waking up. In addition, testing with pictures was carried out, during which the patient named and described the objects depicted, and also practiced mental counting, memorizing a sequence of words, and reading. The criteria for selecting patients for the asleep-awake-asleep protocol were the absence of pronounced mnestic disorders, i.e., the ability to enter into full verbal contact, the absence of pronounced mental lability, and the absence of gross motor and sensory speech deficits. During testing, obvious mnestic disturbances or pronounced sensorimotor aphasia were revealed in 5 patients, as a result of which they decided to refrain from performing a conscious craniotomy.
During the operations, IONM was performed using the Natus Xltek protektor apparatus. The purpose of IONM is to dynamically monitor spontaneous and evoked bio-electrical activity of the brain (motor evoked potentials). During neurophysiological monitoring, motor evoked potentials were assessed using transcranial electrical stimulation based on the activation of pyramidal cells of the corticospinal tract (Brodmann area 4 of the precentral gyrus). Stimulating electrodes were located in the projection of points C3, C4, according to the international scheme 10-20 [3]. Depending on the surgical approach, different electrode placement options were used. To assess the conduction of electrical impulses along the pyramidal tracts, all patients underwent transcranial electrical stimulation, regardless of the severity of the neurological deficit. Motor responses were recorded using needle electrodes installed in muscles ( m .
Orbicularis Oculis , m . Orbicularis Oris , m . Deltoideus , m . Thenari / Hypothenari , m . Rectus Femori , m . Tibialis Anterior
). Transcranial stimulation (Fig. 4) was performed in single trains of 4 short high-frequency stimuli (500 Hz). Tension parameters were selected individually until representative M-responses were obtained from all tested muscles. Registration of M-responses was carried out under conditions of amplifier sensitivity of 50 μV/div with a notch filter of 50 Hz. During the operation, motor responses were recorded on both sides. The difference in amplitude and latency varied depending on the initial neurological deficit and options for installing stimulating electrodes.
Rice.
4. Monitoring of the pyramidal tracts (transcranial stimulation) during removal of glioma of the lower parts of the precentral gyrus of the frontal and lower parts of the postcentral gyrus of the parietal lobe of the left hemisphere. The test muscles were chosen. Deltoideus (a), m. Thenari (b, c), m. Tibialisanterior(d, d). The orange arrow indicates the M-response obtained from the muscle being tested. The red arrow indicates a series of stimuli. Motor cortical mapping (Fig. 5) was used in 50 patients with involvement of the precentral gyrus or premotor cortex. For this purpose, the technique of direct stimulation of the cortex with a bipolar electrode was used in packs of 4 stimuli with an internal frequency of 500 Hz and a stimulus strength of up to 25 mA with registration of motor responses from the tested muscles of the contralateral side.
Rice. 5. Motor mapping of the middle and lower parts of the precentral gyrus before encephalotomy in a patient undergoing removal of a glioma of the frontotemporal localization. The test muscles chosen were m. Longinalis superior (a), m. Orbicularis oris (b), m. Deltoideus (c), m. Thenari (g), m. Tibialis Anterior (e), m. Rectus.
Patients ( n
=16) with the tumor localized in the projection of the speech zones, tumor removal was carried out according to the asleep-awake-asleep protocol [4]. After depression of consciousness by intravenous administration of a propofol solution at a dose of 1.0-1.5 mg/kg, analgesia with a fentanyl solution at a dose of 2.5-3.0 mcg/kg and muscle relaxation with rocuronium at a dose of 0.7 mg/kg, tracheal intubation was performed and mechanical ventilation began in normal ventilation modes. Control of the patient's level of consciousness was ensured by inhalation of desflurane in doses of 0.3-0.6 MAC under conditions of monitoring the depth of depression of consciousness (target BIS values were 50-60). To assess the level of muscle relaxation, a neuromuscular conduction monitor using the TOF technique was used. The skin incision line was infiltrated with a solution of 0.2% ropivocaine in total doses not exceeding 300 mg, taking into account regional anesthesia. Anesthesia of the dura mater (DRM) was carried out by applying pads with lidocaine. After craniotomy was performed and the level of restoration of neuromuscular conduction, TOF 0.9 or more, was achieved, the supply of desflurane was stopped, the patient was awakened and extubated. Mapping of the FZZ of the brain was performed in 2 stages. Before awakening the patient, the motor areas bordering the formation were verified using direct electrical stimulation of the cortex. After awakening and extubation, verbal contact was established, and then speech zones were mapped (Fig. 6). For intraoperative verification of Wernicke's area, tasks were selected to repeat a series of frequency words in threes, which allows diagnosing disorders of phonemic hearing and the volume of auditory-verbal perception (as well as the pronunciation side of speech), testing with naming pictures, reading and counting. The intraoperative speech testing procedure was practiced with patients on the eve of surgery; only tasks that were available for stable, error-free execution were included in the test set. During stimulation of the cortex with a bipolar stimulator in Broca's and Wernicke's areas with rhythmic bursts of 4 stimuli with a strength of 15-20 mA, various types of speech impairment were recorded in some patients: speech-arest (5 patients), elements of motor aphasia, literal paraphasia with replacement of sounds by acoustic proximity and verbal paraphasia with substitution of words based on acoustic proximity, characteristic of phonemic hearing impairment (7).
Rice.
6. Intraoperative mapping of speech zones. Intraoperative photo (a). The trepanation window is formed in the left frontal-temporo-parietal region. The dura mater has been opened. After the patient woke up, mapping of speech zones was performed. Broca's area (22, 21, 25 - yellow outline), Wernicke's area (16-18, 20 - green outline) and the lower parts of the precentral gyrus (22, 26 - blue outline) were identified. On fMRI (b), the speech centers are indicated in green; the tumor is localized in the left insula. After verification of Broca's and Wernicke's areas, the tumor was removed with neurological and neurophysiological control of the preservation of speech functions and motor tracts (Fig. 7). In 2 patients, after mapping of speech zones, motor restlessness and emotional lability developed, which required resumption of endotracheal anesthesia (average time awake was 30±12 minutes).
Rice. 7. Intraoperative photo. Stage of tumor removal with intraoperative mapping of speech zones. At the awake stage, mapping of speech zones was carried out. The marks indicate Wernicke's area, discovered during direct stimulation of the cortex during the awakening stage. The green outline indicates the projection of the tumor.
In the remaining 14 patients, testing continued throughout the entire tumor removal (awake time was 120±20 minutes). After tumor removal, patients were again anesthetized, intubated with brief muscle relaxants, and surgery was completed under general anesthesia with continued monitoring via transcranial stimulation.
In 11 (17%) patients with tumor spread into the internal capsule, stimulation of the motor pathways was performed (Fig. 8). The stimulation threshold was decreased stepwise from 10 to 5 mA (according to the literature, a change of 1 mA corresponds to a change of distance of 1 mm). Changing the stimulus strength to a minimally representative one made it possible to remove the tumor in close proximity to the internal capsule. In 5 (8%) patients during tumor removal due to the appearance of a motor response to a stimulus strength of 5 mA, removal was stopped due to the extremely high risk of neurological deficit.
Rice. 8. Removal of a frontal lobe tumor with intraoperative mapping of motor areas. a — intraoperative photo: the stage of tumor removal of the left frontal lobe, the arrow indicates a bipolar stimulator used during mapping of motor pathways in the white matter. On fMRI, arrows indicate the motor representation of the arm (b) and leg (c), the tumor is located in close proximity to these zones and is in contact with the pyramidal tracts.
Regardless of the tumor location and the chosen anesthesia protocol (including awake craniotomy), all patients underwent background monitoring of transcranial motor evoked potentials. In 8 patients, the amplitude of the M response decreased by more than 50% during tumor removal. When assessing the postoperative neurological status, all of them were included in a group of 11 patients whose motor deficit increased. In 21 patients, a temporary decrease in amplitude was noted (by no more than 40%), which is apparently explained by the presence of a brain displacement effect after tumor removal or the effect of short muscle relaxants at the stage of re-intubation according to the asleep-awake-asleep protocol.
In 43 (66%) patients, the histological diagnosis corresponded to glioblastoma (WHO Grade IV), in 7 (11%) - fibrillary astrocytoma (WHO Grade II), in 6 (9%) - oligodendroglioma (WHO Grade II). Anaplastic astrocytoma (WHO Grade III) was verified in 9 (14%) patients, of which 2 patients were re-operated using mapping due to continued tumor growth.